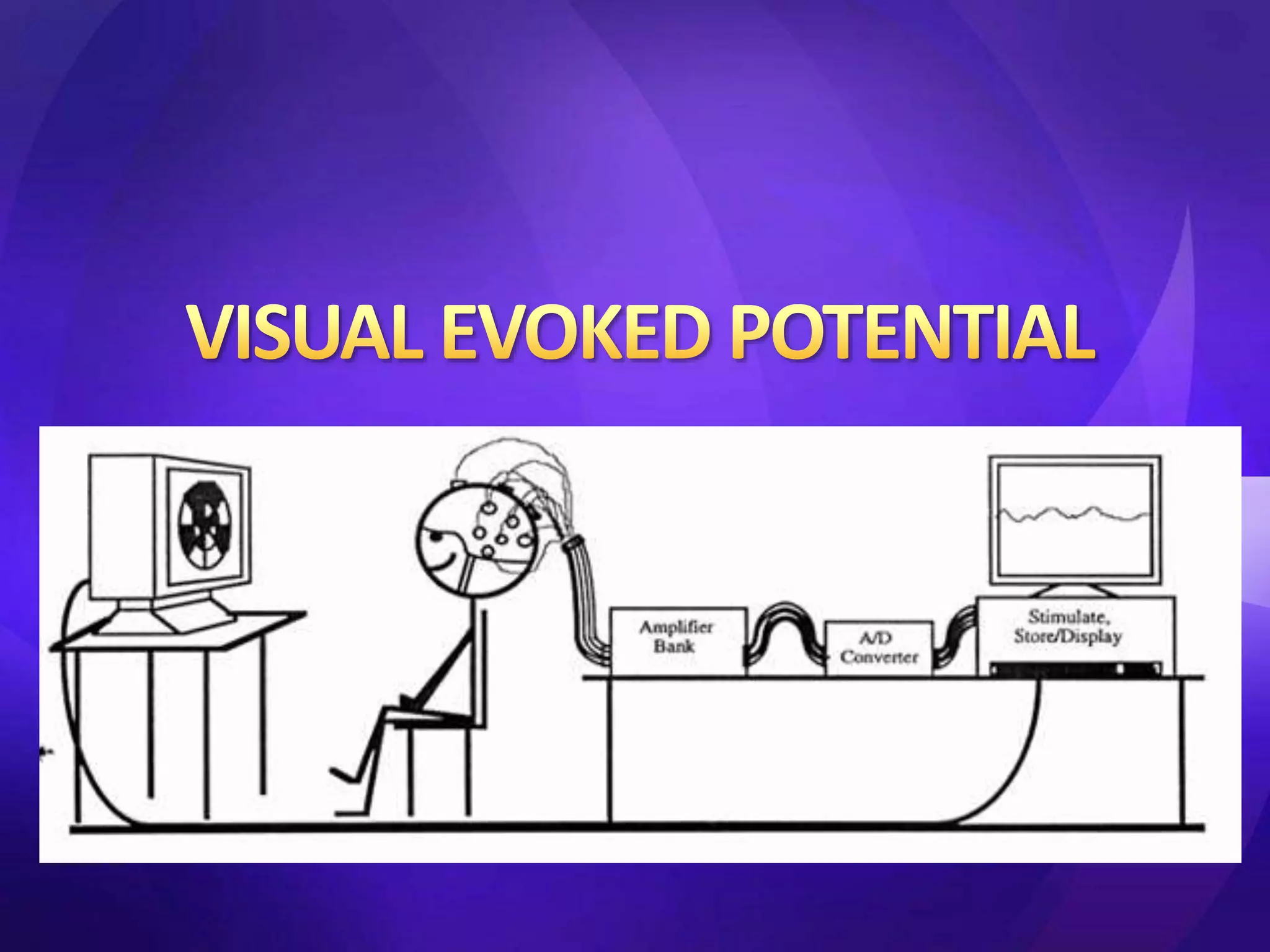
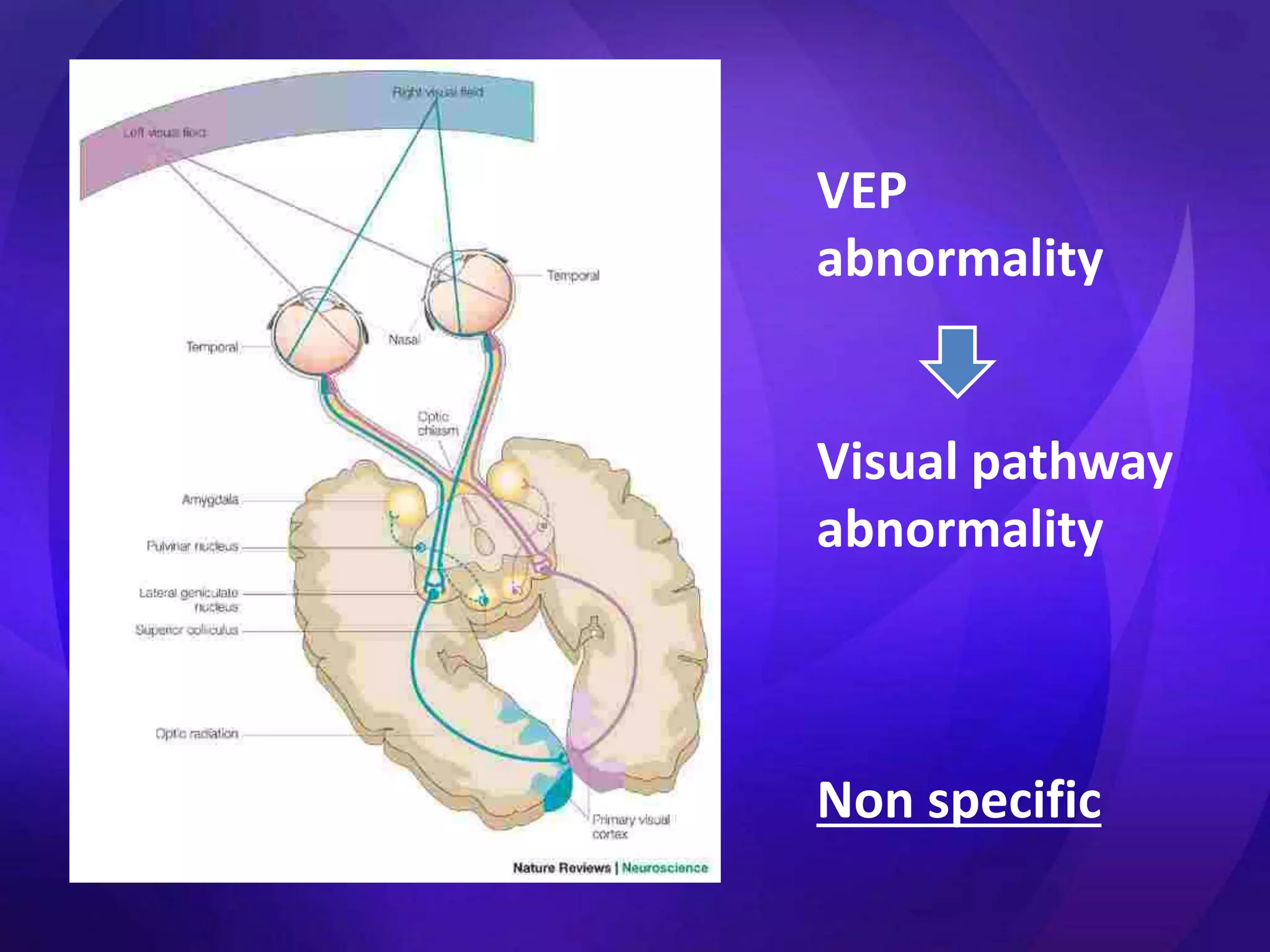
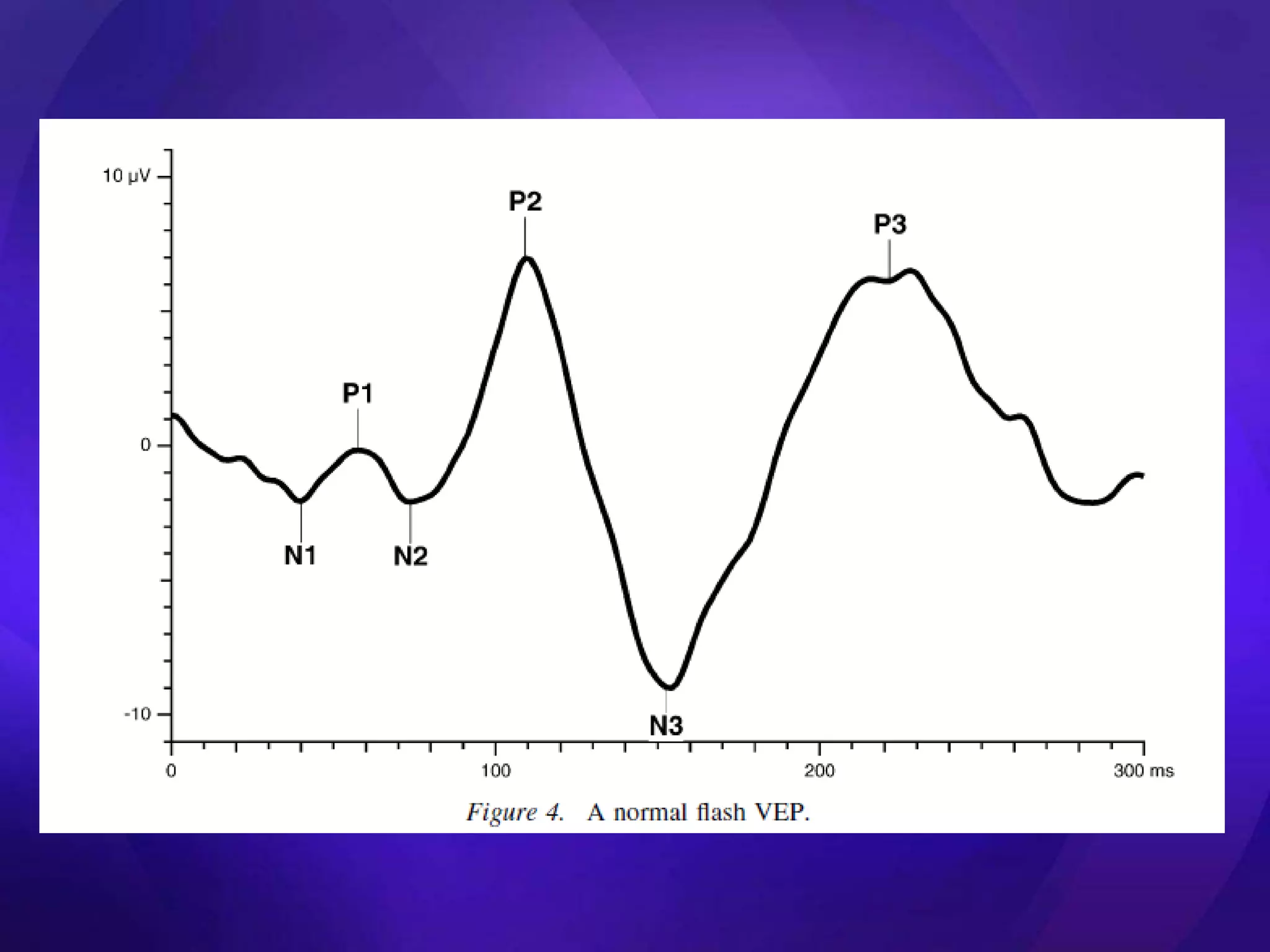
The document discusses visual evoked potentials (VEPs), which involve recording electrical signals from the visual cortex in response to visual stimulation. It notes that VEPs have smaller amplitudes than EEGs but can objectively assess macular function and the functional state of the visual system. It describes how steady state VEPs use rapid stimulation to produce sinusoidal waveforms while transient VEPs use discrete deflections with low rates of stimulation. It also discusses the use of flash VEPs, pattern VEPs, and other techniques and provides details on stimulation methods, components of VEP testing equipment, factors that influence VEPs, and abnormal findings that may be observed in various conditions.