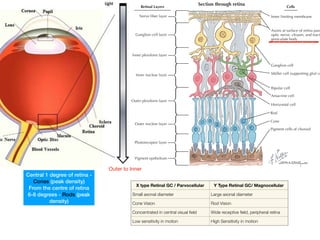
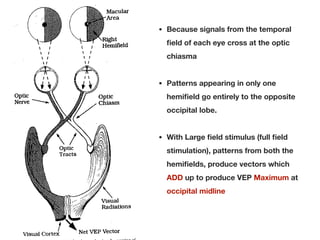
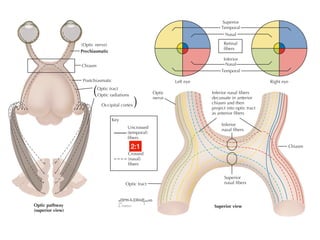
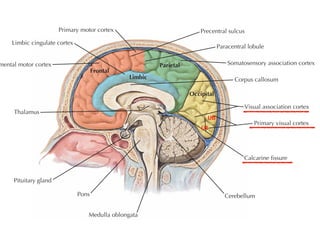
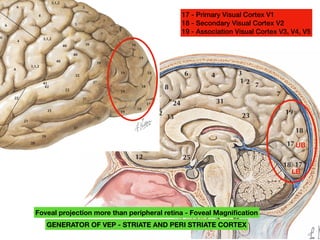
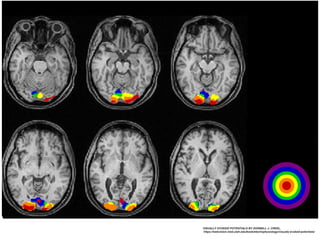
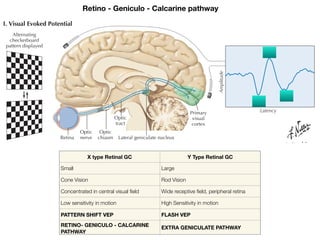
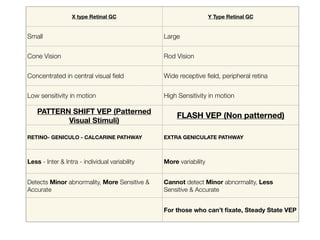
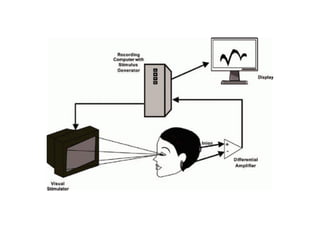
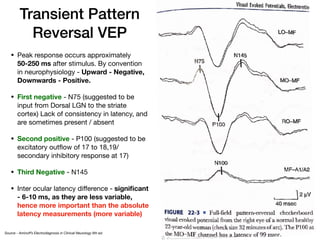
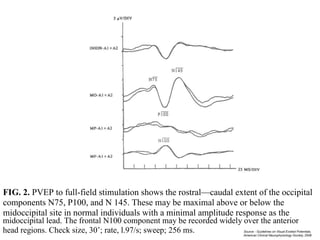
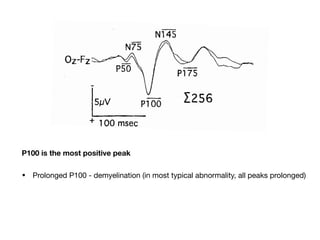
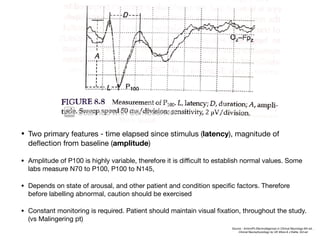
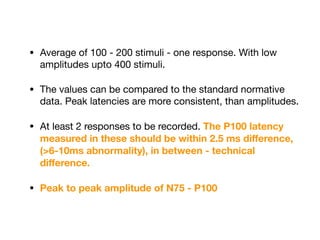
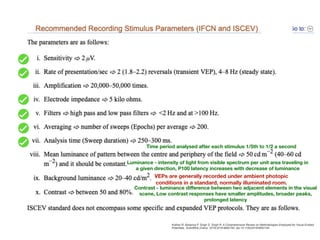
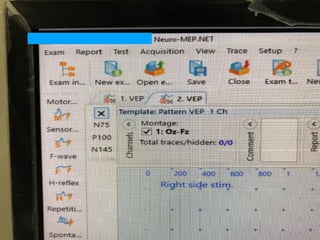
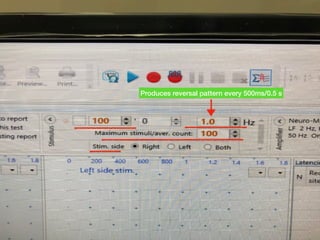
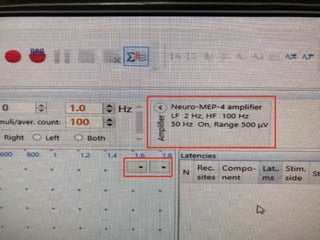
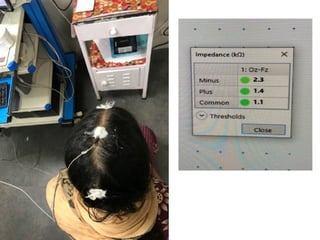
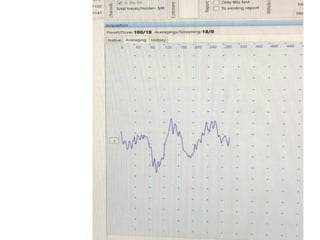
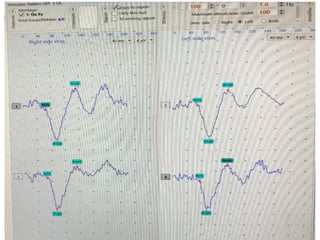
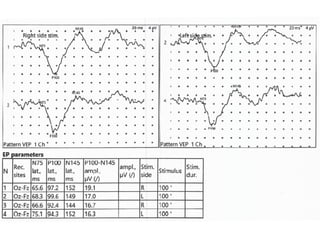
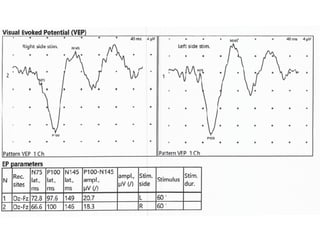
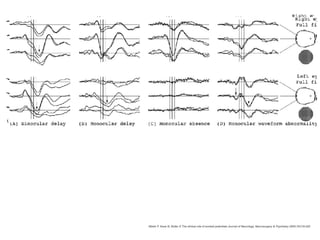
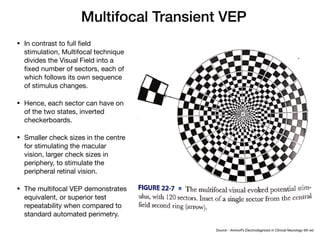
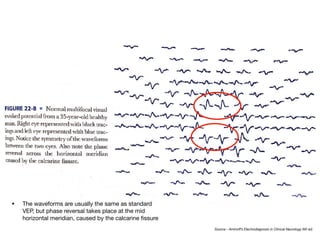
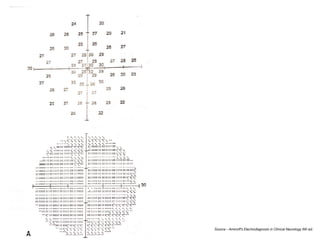
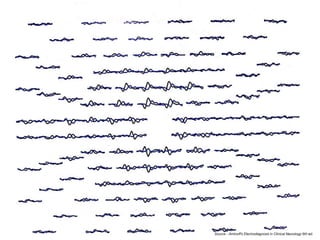
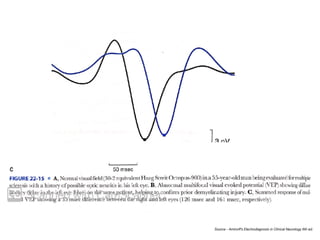
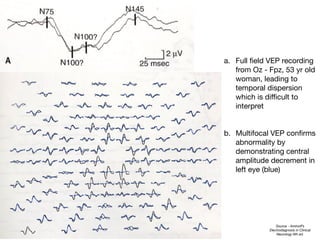
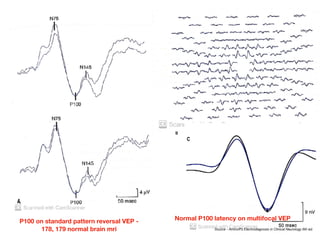
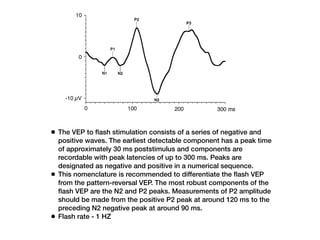
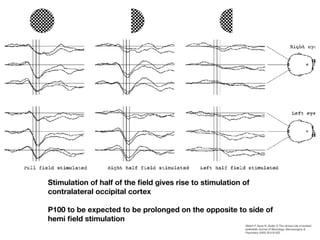
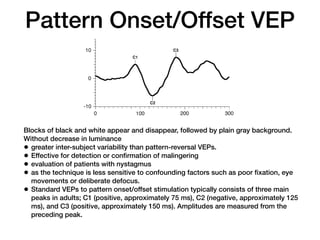
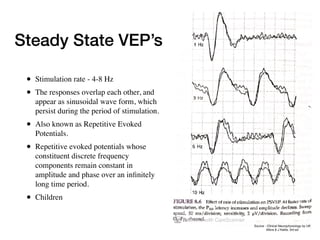
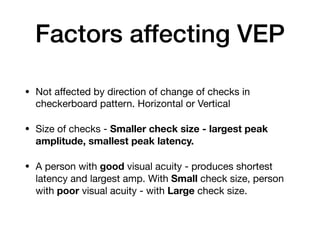
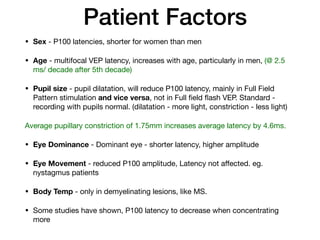
Visual evoked potentials (VEPs) record electrical signals from the scalp in response to visual stimuli. VEPs are useful for objectively assessing visual function, especially of the retina and optic nerve. The VEP involves presenting a visual stimulus such as a flashing light or alternating checkerboard pattern. Electrodes placed on the scalp record the P100 waveform generated in the striate and peristriate cortex in response to the stimulus. Analysis of the P100 latency, amplitude, and interocular latency difference can help detect and localize abnormalities in the retina, optic nerve, optic tract, and visual cortex.