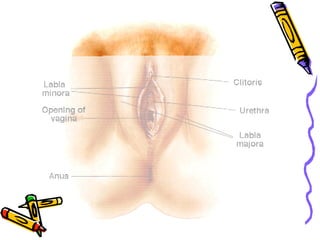
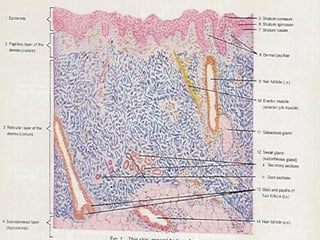
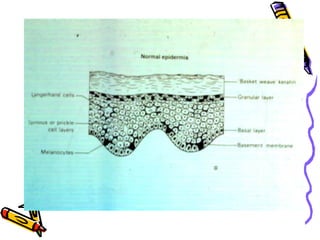
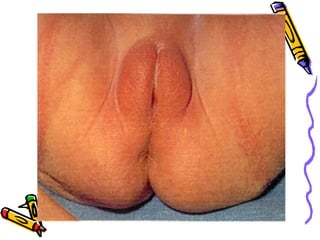
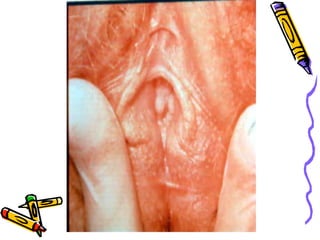
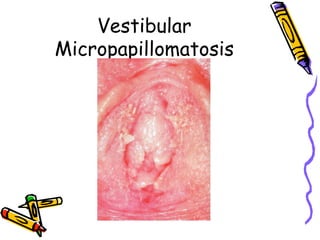
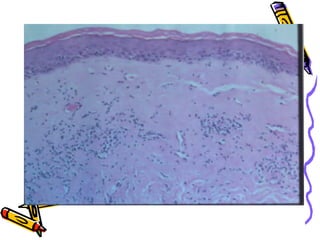
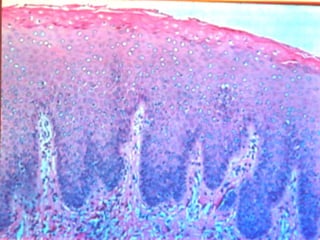
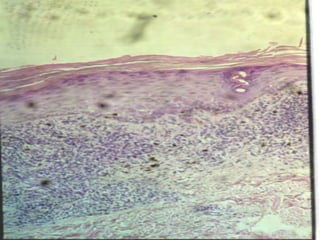
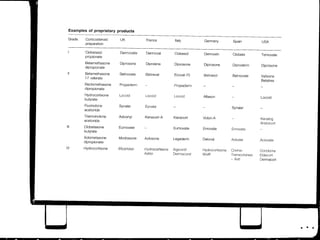
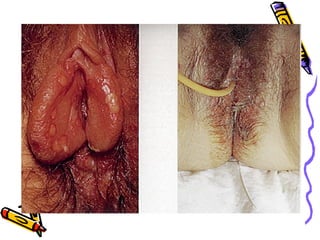
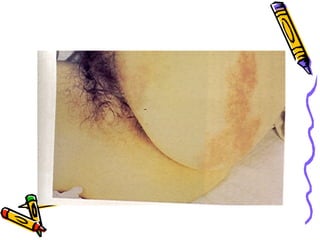
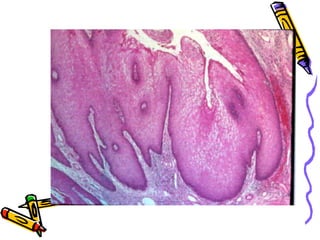
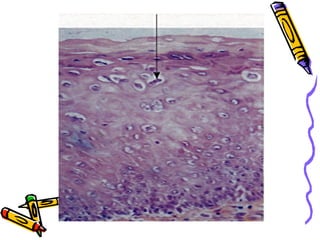
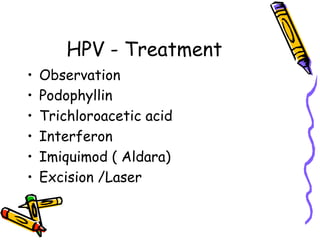
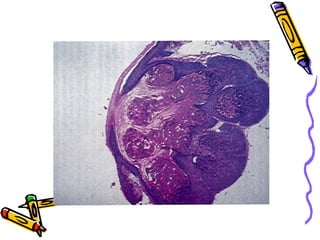
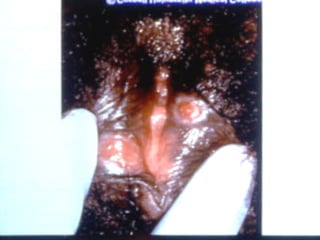
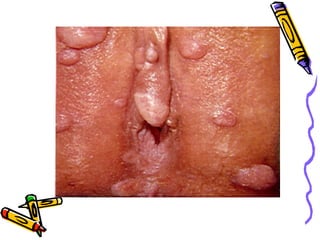
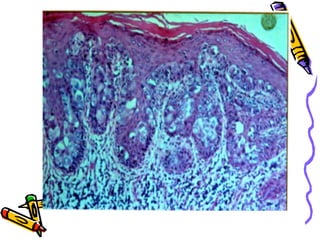
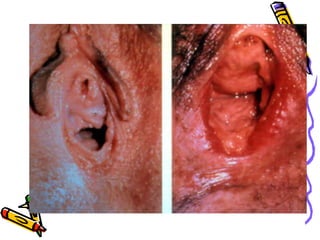
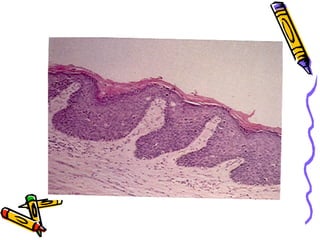
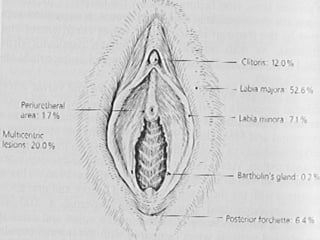
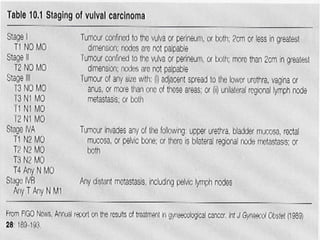
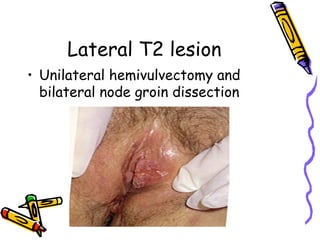
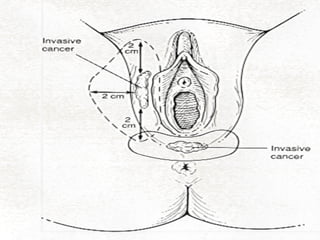
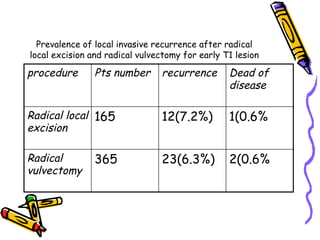
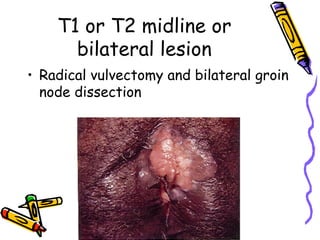
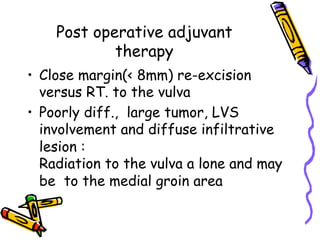
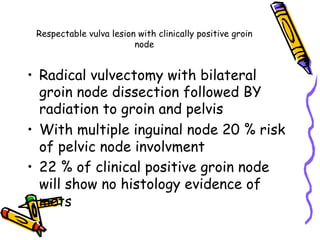
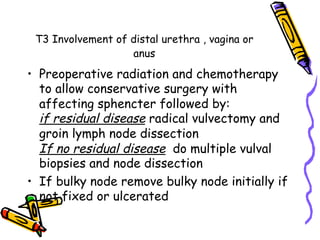
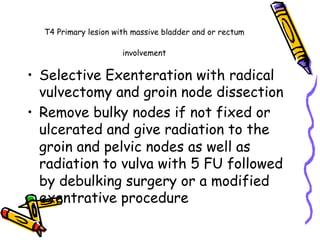
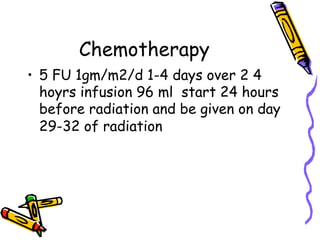
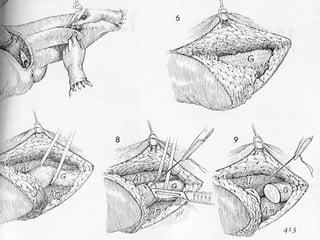
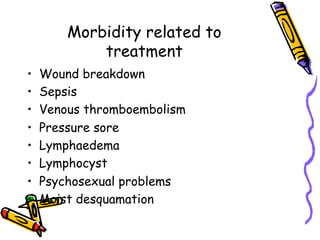
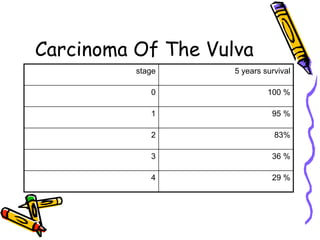
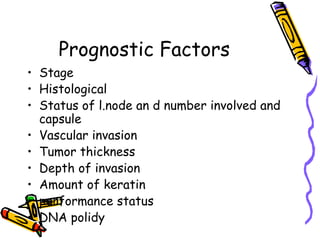
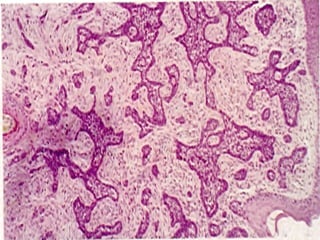
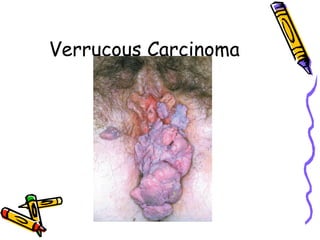
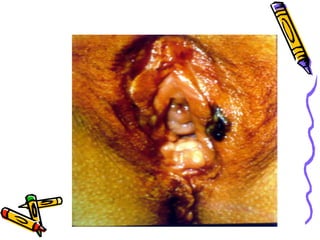
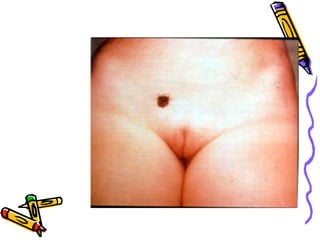
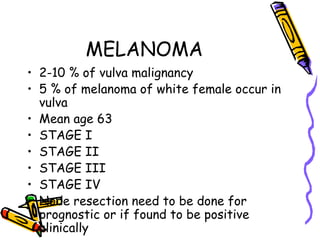
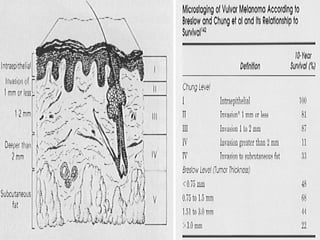
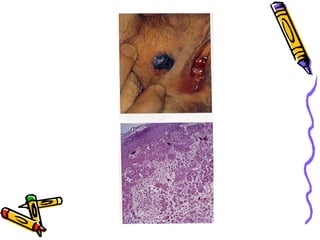
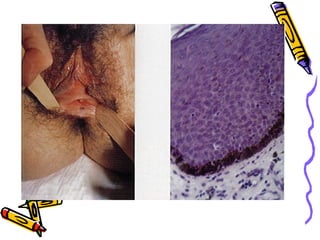
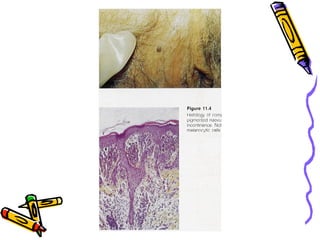
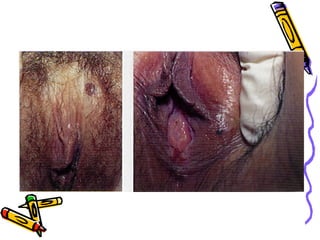
This document discusses benign and malignant diseases of the vulva. It covers symptoms, general pathology, diagnosis of white, red and brown lesions. Nonneoplastic epithelial disorders like lichen sclerosis and squamous cell hyperplasia are examined. Malignant diseases like HPV, VIN, and carcinoma are addressed. Cancer epidemiology, management including staging, surgery, radiation and chemotherapy are summarized. Prognostic factors and recurrence are also reviewed. Key points emphasize inspection, biopsy, medical therapy for benign conditions and challenges in vulvar cancer treatment.