Dr. Jean Peiffer
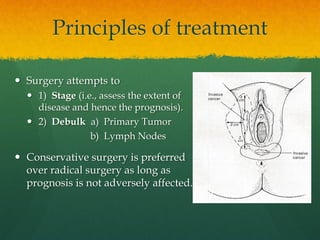
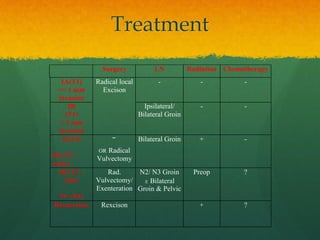
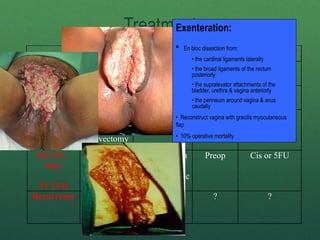
- Wide excision of vulva and perineum
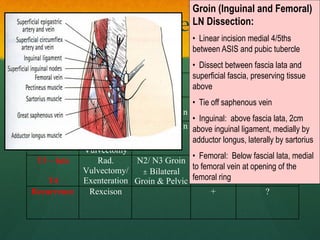
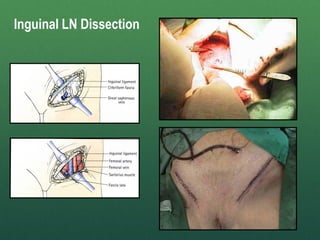
- Bilateral inguinal lymphadenectomy
- Primary closure
- Mortality <5%
- Recurrence <10%
- Standard treatment for >50 years
- Morbidity high: wound breakdown, lymphedema, sexual dysfunction
- Replaced by less radical surgery when LN status shown to be most important prognostic factor
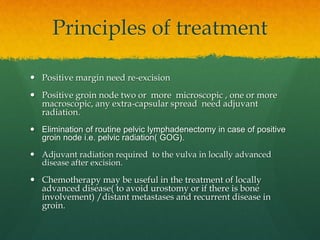
- Still indicated for large fixed tumors with close or positive margins
- Adjuvant radiation reduces recurrence rates
- Quality of life better with less radical surgery when oncologically sound
- Basset’s operation established vulvar cancer surgery as a subspecial