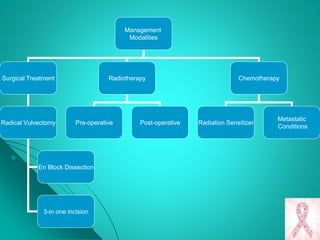
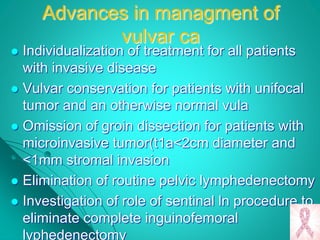
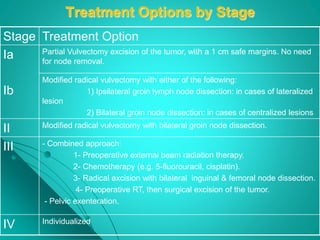
This document discusses cancer of the vulva, including its incidence, risk factors, types, diagnosis, staging, prognosis, and management. Some key points:
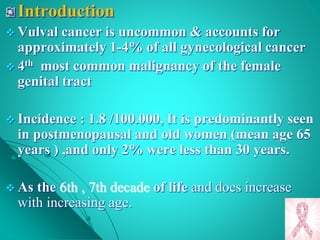
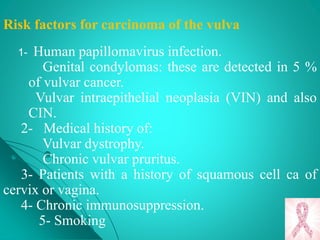
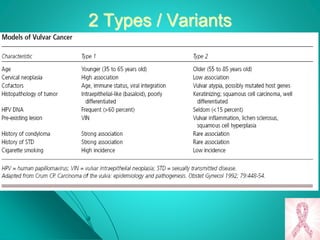
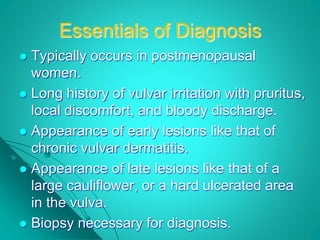
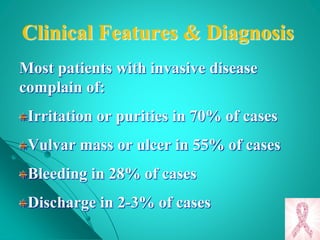
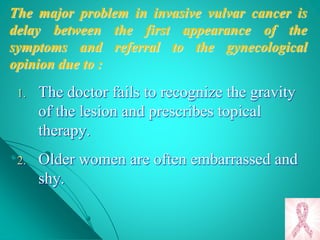
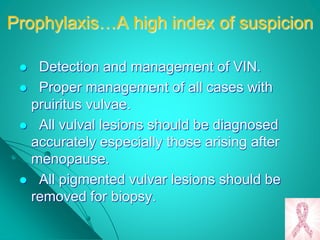
- Vulvar cancer accounts for 1-4% of gynecological cancers and predominantly affects postmenopausal women. Risk factors include HPV infection, smoking, and history of other gynecological cancers.
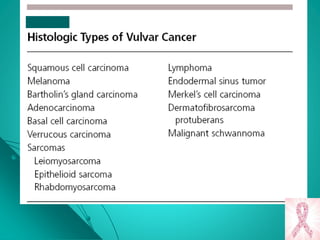
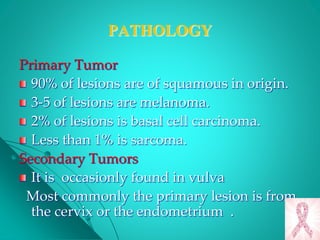
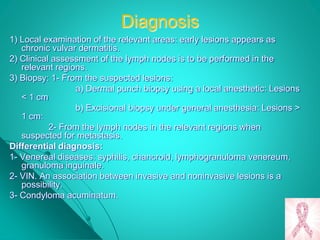
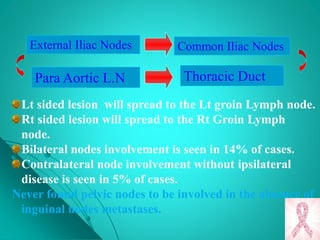
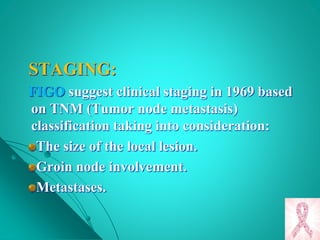
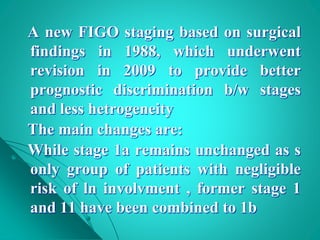
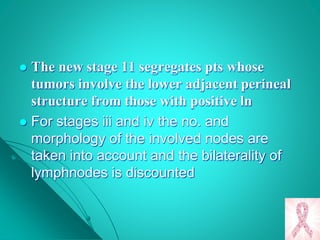
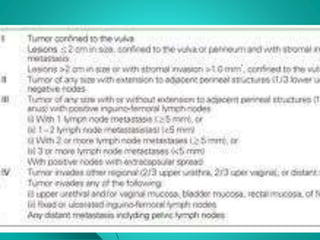
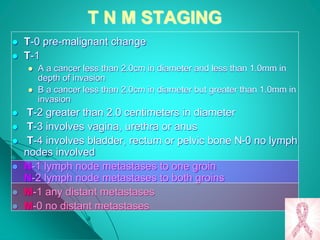
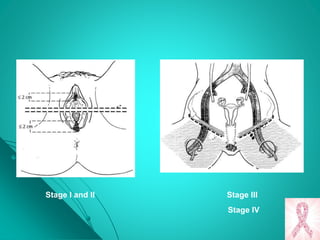
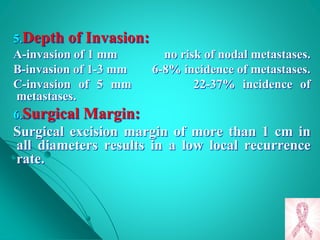
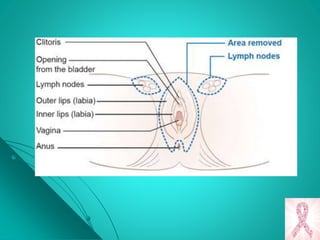
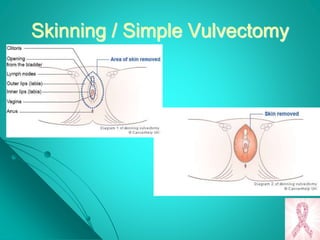
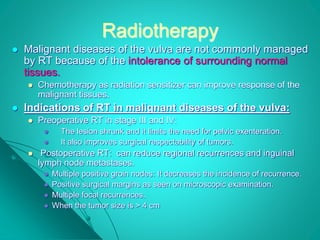
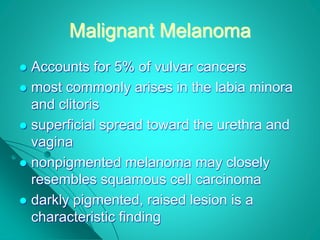
- Squamous cell carcinoma makes up 90% of cases. Diagnosis requires biopsy of any suspicious lesions. Staging is based on tumor size and spread to lymph nodes or distant sites.
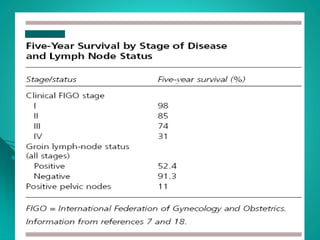
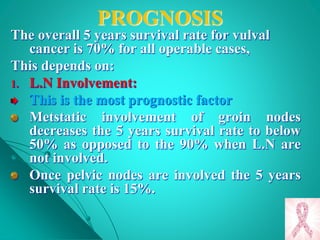
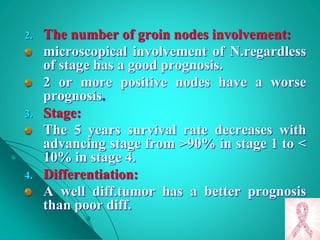
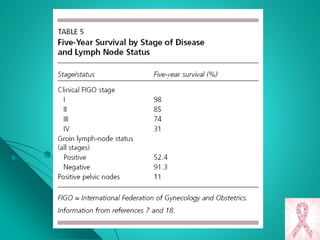
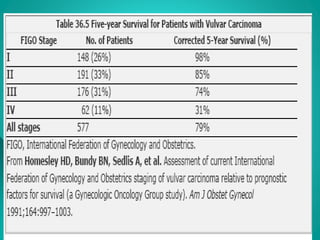
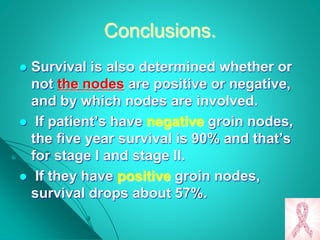
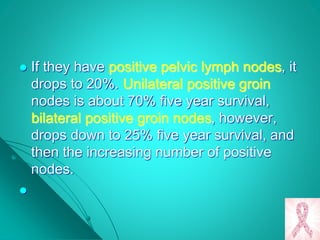
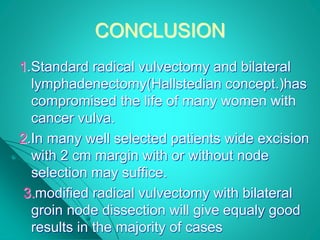
- Prognosis depends on lymph node involvement, with 5-year survival rates over 90% for stage I but under 50% if nodes are