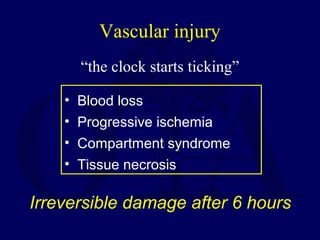
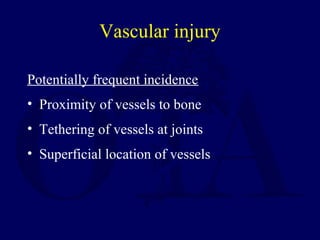
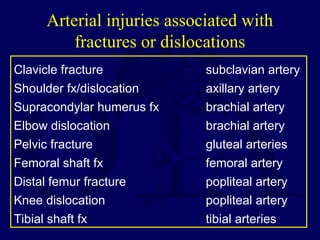
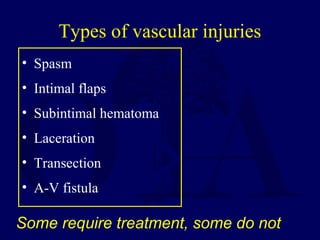
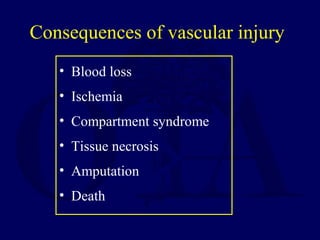
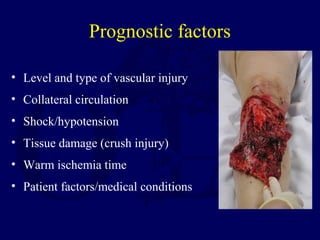
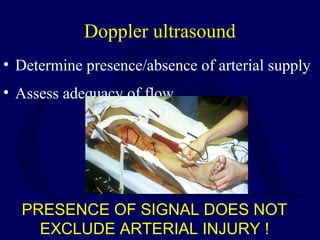
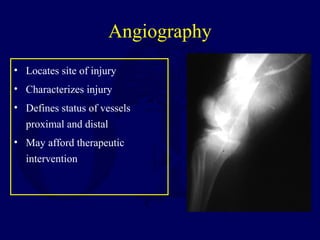
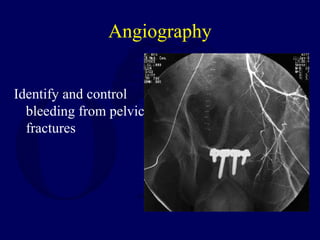
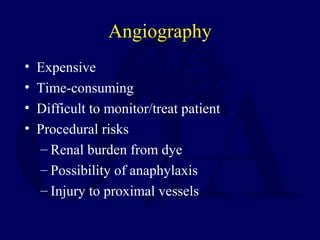
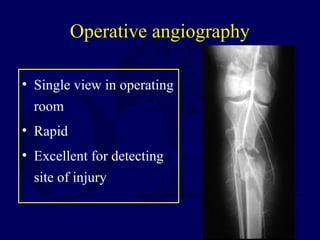
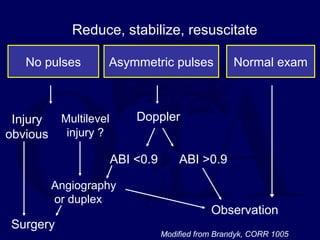
This document discusses the evaluation and treatment of vascular injuries associated with orthopedic trauma. Vascular injuries can cause irreversible tissue damage within 6 hours so rapid diagnosis and treatment is crucial. Physical exam, Doppler ultrasound, angiography, and surgical exploration are used to diagnose injuries. The type and level of injury, collateral circulation, ischemia time, and patient factors impact prognosis. Immediate treatment involves controlling bleeding, resuscitation, and splinting injuries. Urgent surgical treatment may be needed for arterial injuries or absent pulses. Ongoing monitoring of circulation and compartment pressures is important after initial treatment.