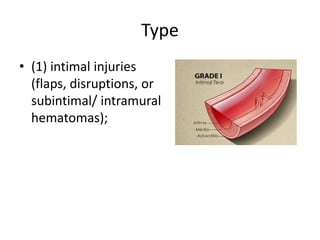
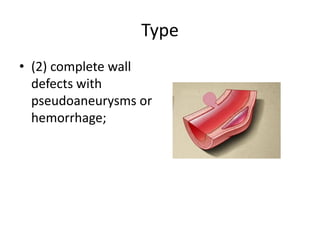
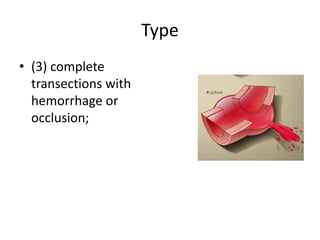
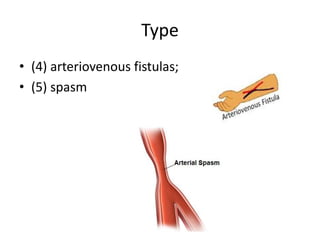
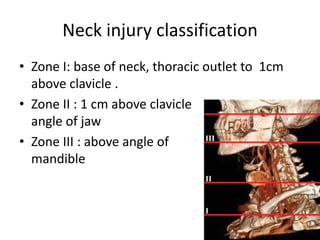
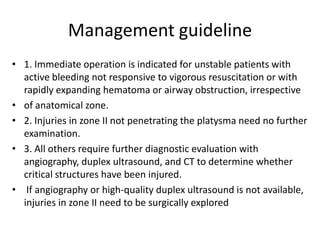
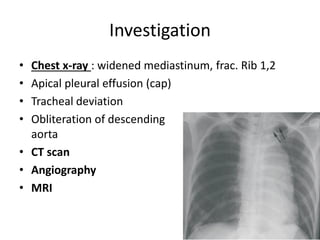
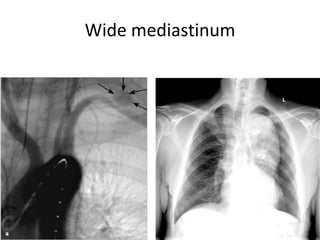
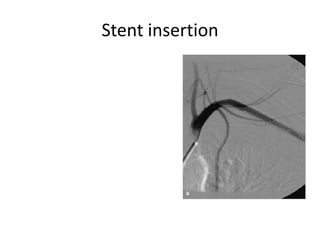
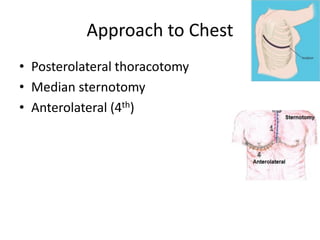
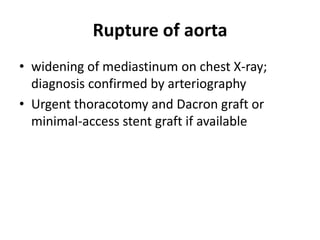
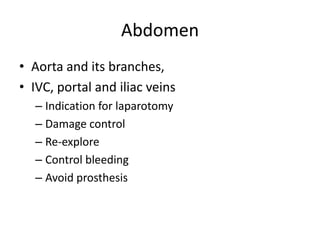
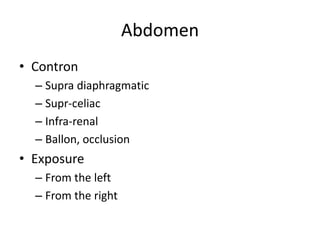
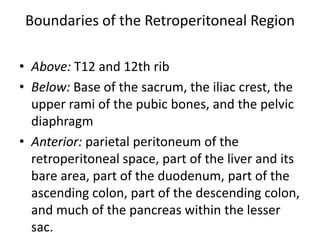
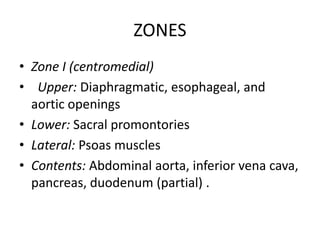
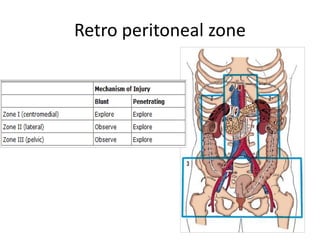
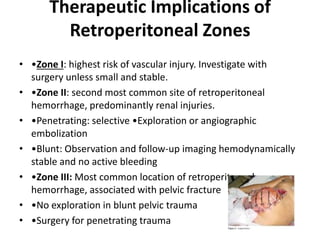
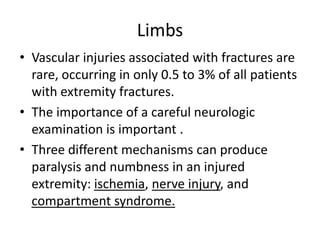
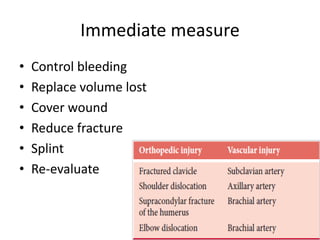
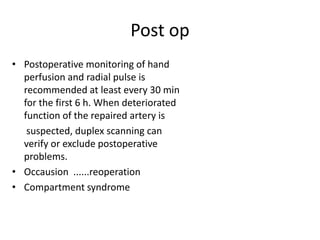
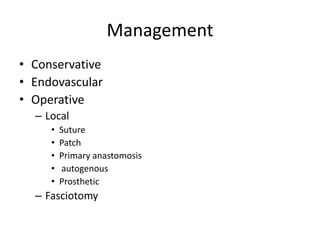
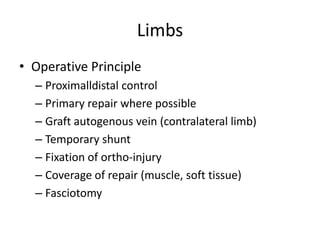
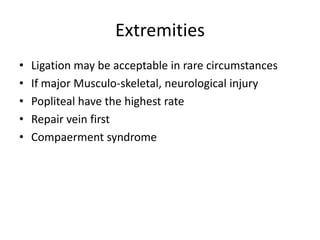
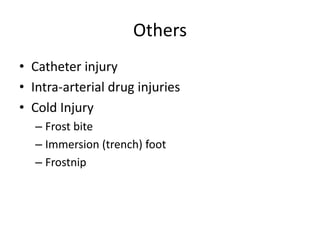
This document discusses various types of vascular injuries. It covers the basic principles of vascular injury including anatomy, type of injury, mechanisms, clinical manifestations, investigations and management. It describes different types of vascular injuries like laceration, transection, dissection, crush and thrombosis. It discusses evaluation and investigations like Doppler, duplex ultrasound, angiography, CT angiography and MRI. It covers management of vascular injuries in different body regions like neck, chest, abdomen and extremities. It provides guidelines on treatment approaches including operative versus endovascular management.