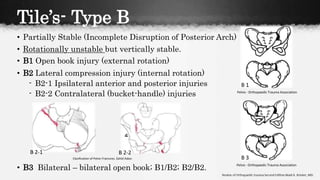
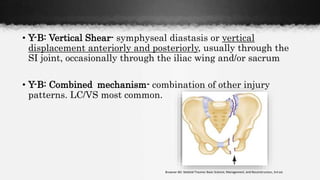
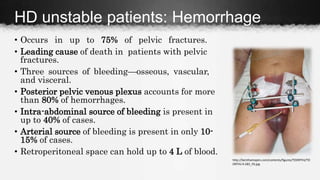
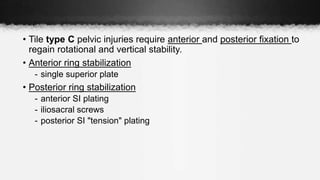
Pelvic fractures can be life-threatening injuries that require prompt treatment. They account for 3% of all fractures and mortality is as high as 22% depending on the severity of the injury. The pelvis forms a ring structure connecting the sacrum to the two innominate bones. High-energy impacts from motor vehicle accidents are the most common causes of pelvic fractures. Tile and Young-Burgess classifications are used to characterize the fractures and guide treatment. Unstable fractures with hemorrhage require emergency stabilization, usually with an external fixator or pelvic binder, and fluid resuscitation to prevent hypovolemic shock.