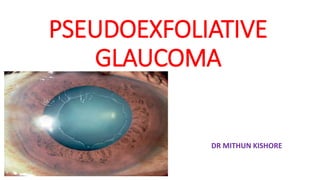
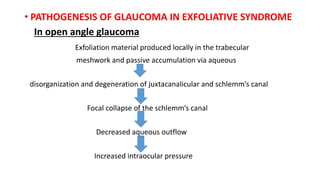
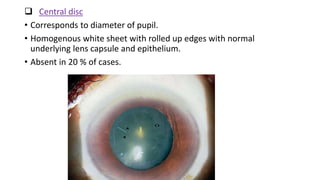
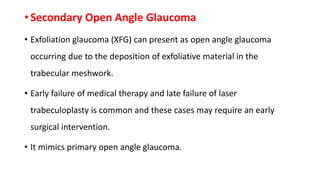
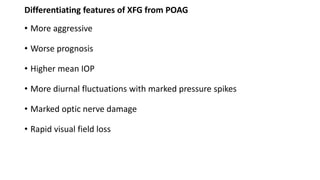
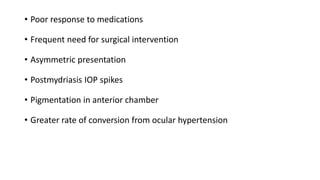
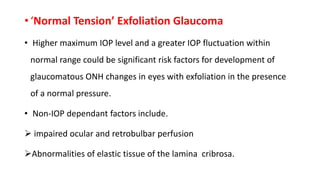
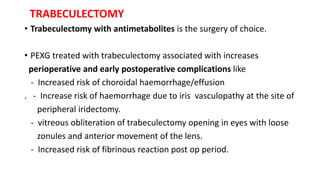
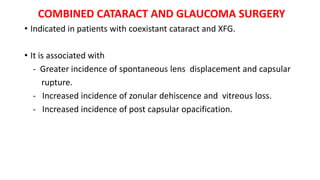
Exfoliative glaucoma is a type of open-angle glaucoma caused by the buildup of exfoliative material in the eye. It develops as a complication of exfoliative syndrome, which is characterized by the progressive production and deposition of abnormal fibrillar material in ocular tissues. Exfoliative glaucoma presents with higher intraocular pressures that are difficult to control and a worse prognosis compared to primary open-angle glaucoma. Treatment involves medications, laser trabeculoplasty, and early surgical intervention such as trabeculectomy, as exfoliative glaucoma often responds poorly to medical and laser therapies.