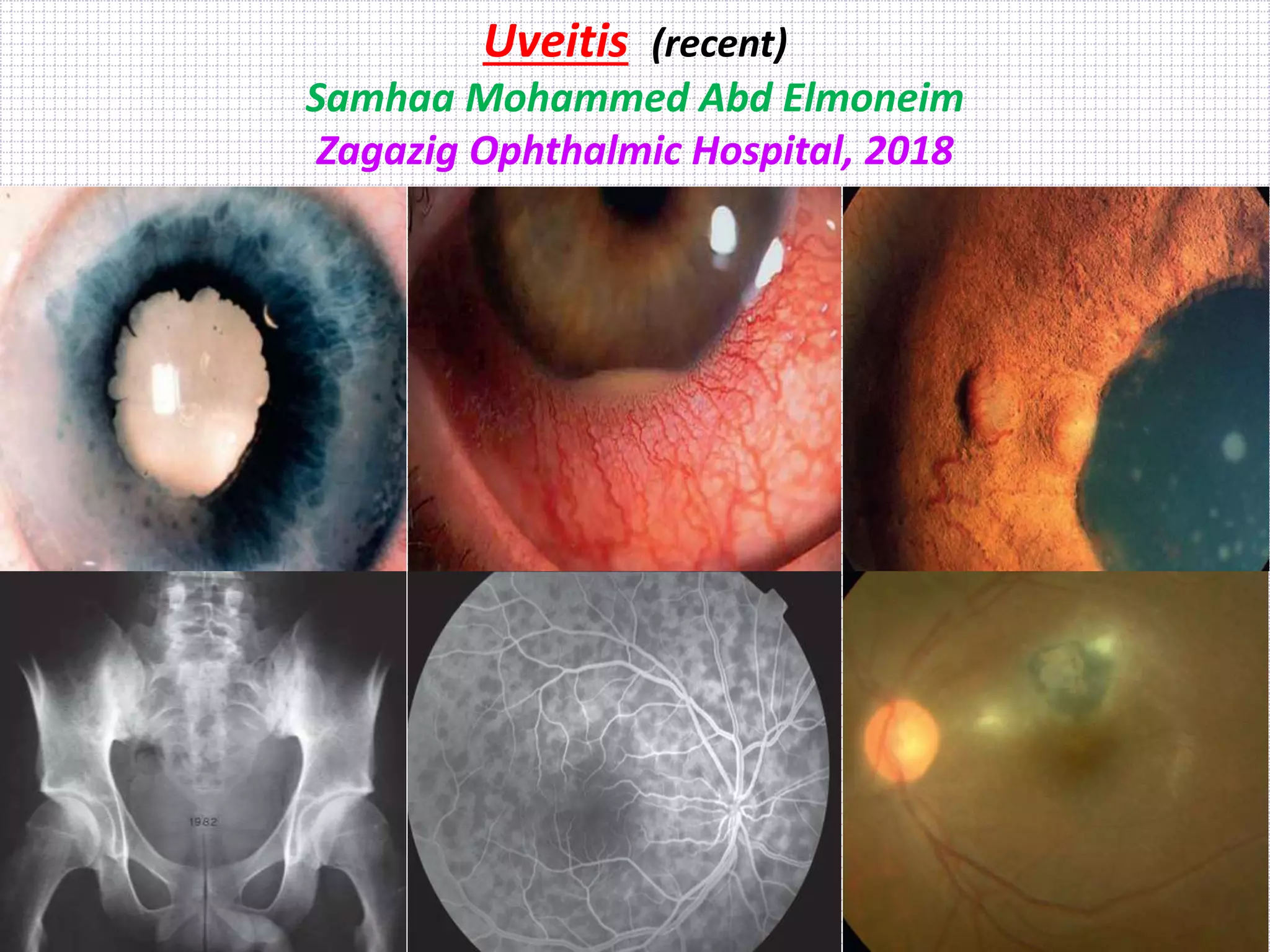
This document discusses uveitis, including its classification, description, causes, and clinical presentation. It provides details on:
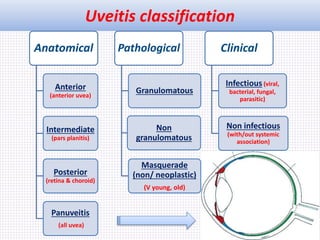
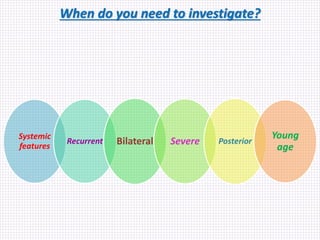
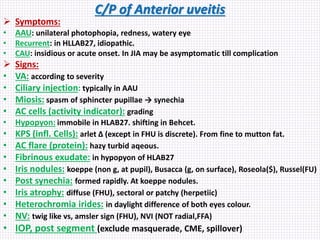
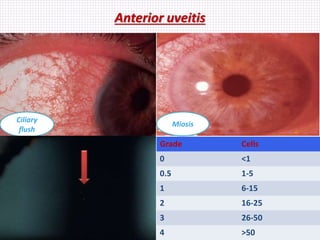
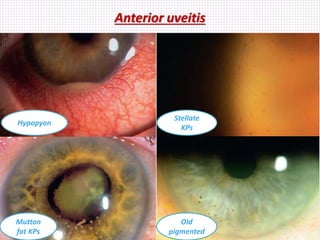
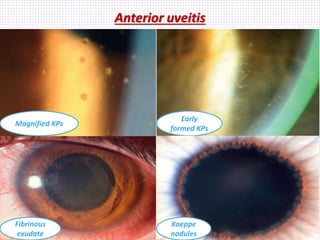
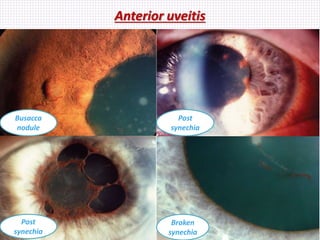
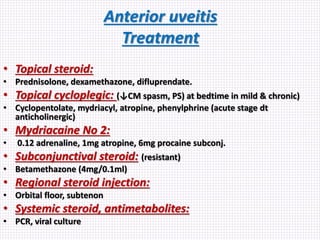
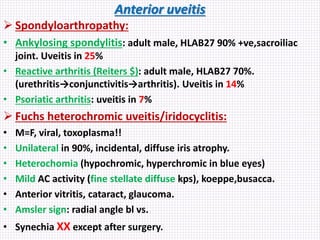
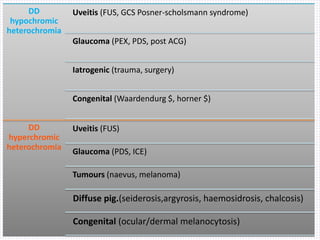
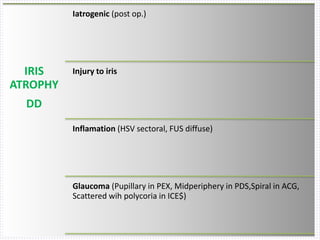
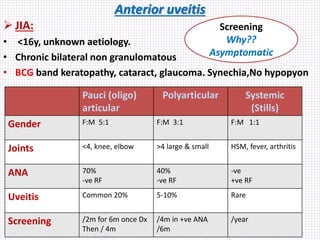
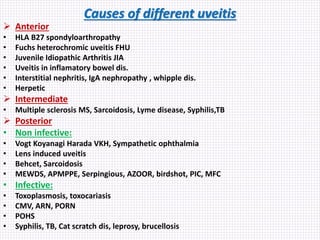
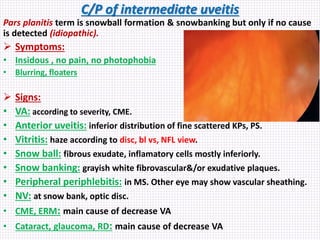
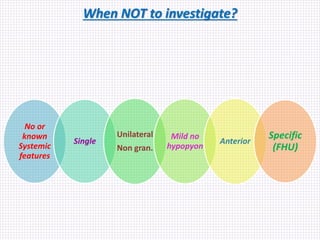
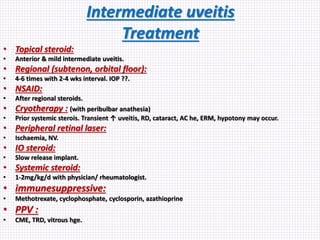
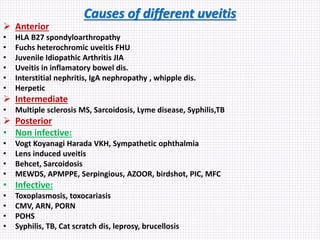
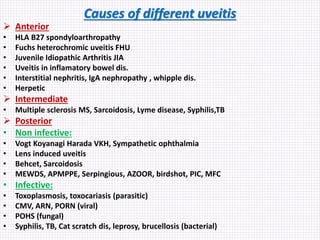
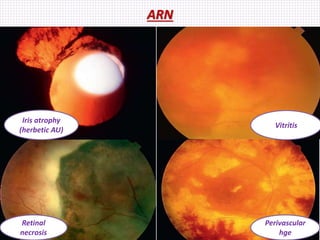
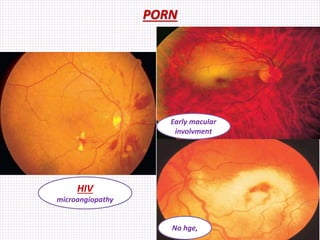
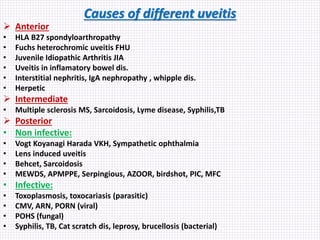
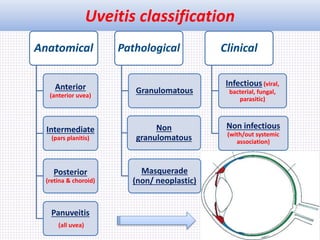
1) The anatomical, pathological, and clinical classifications of uveitis including anterior, intermediate, posterior, and panuveitis.
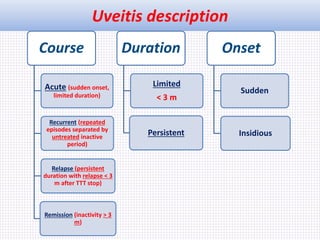
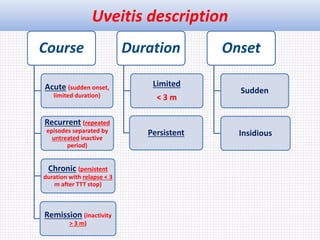
2) The description of uveitis including its course (acute, recurrent, relapse, remission), duration (limited, persistent), and onset (sudden, insidious).
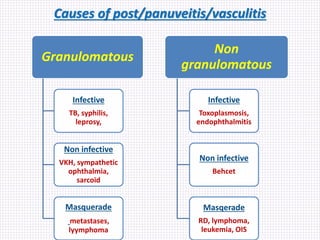
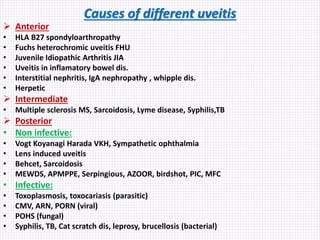
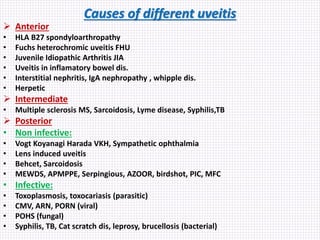
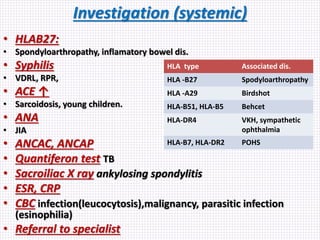
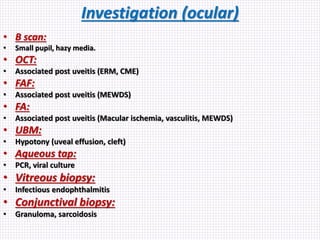
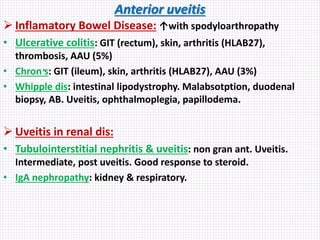
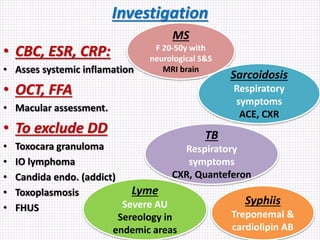
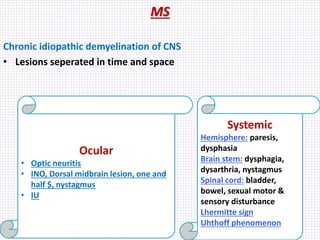
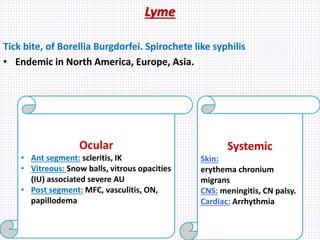
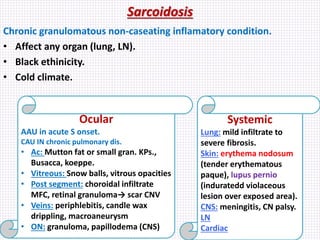
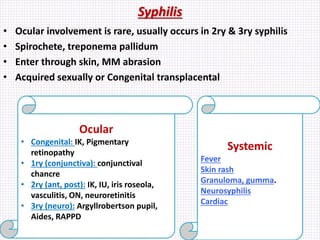
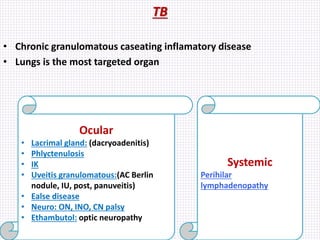
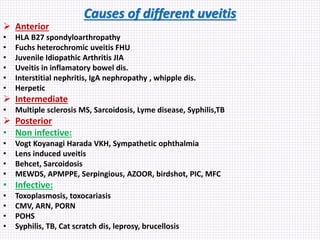
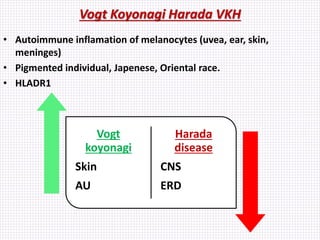
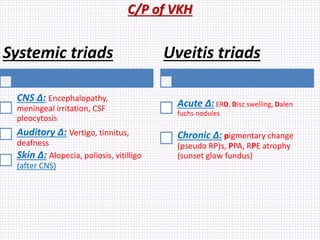
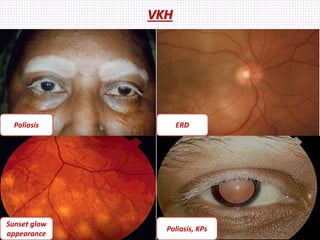
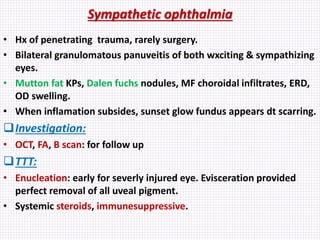
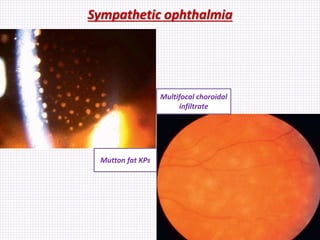
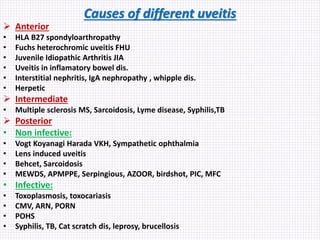
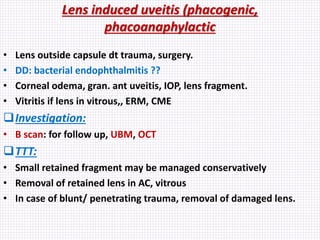
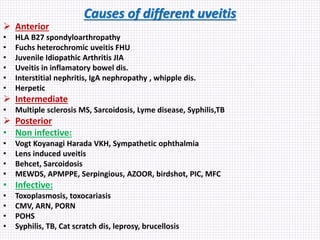
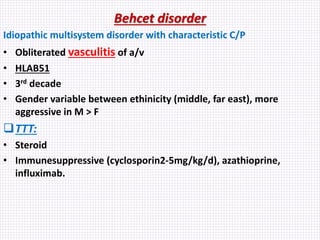
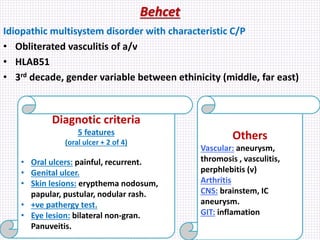
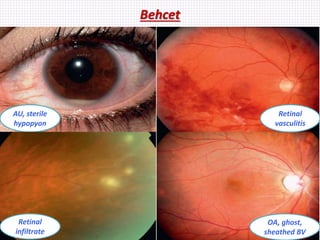
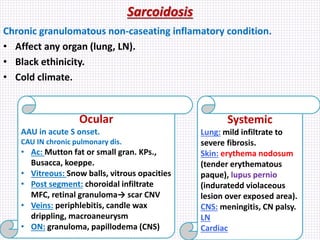
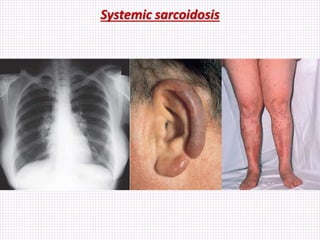
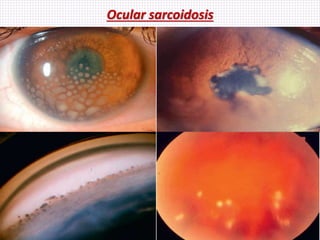
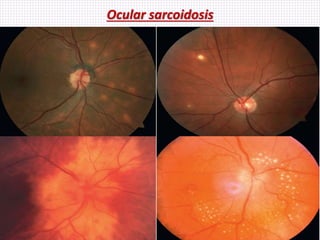
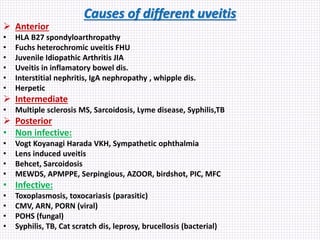
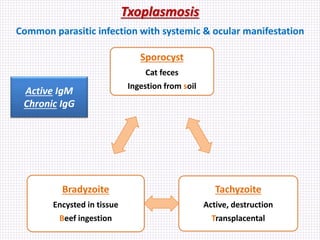
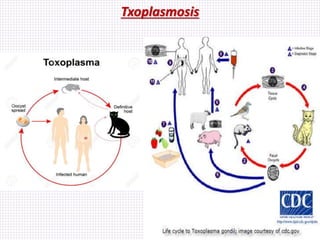
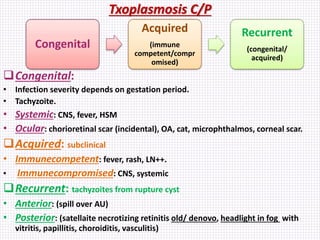
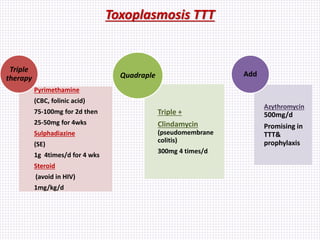
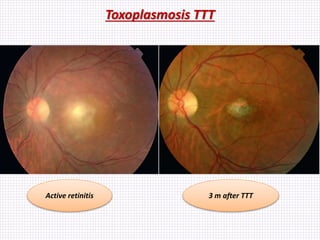
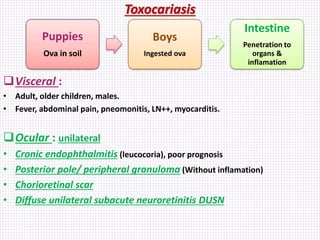
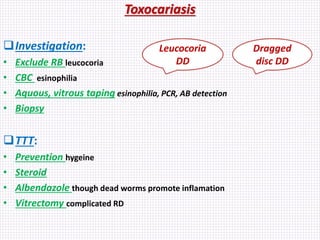
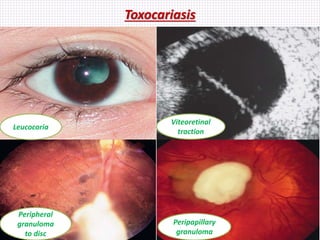
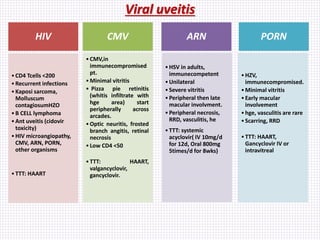
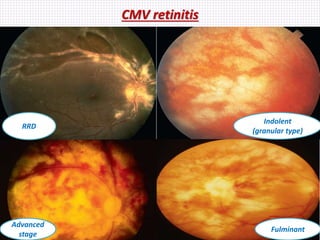
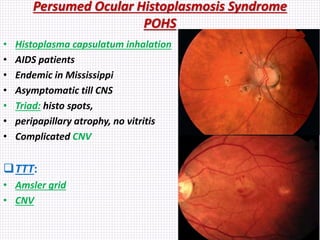
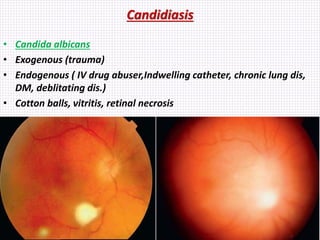
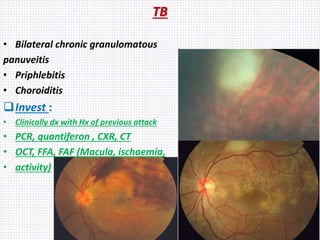
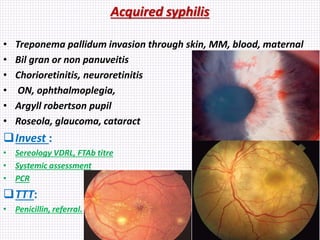
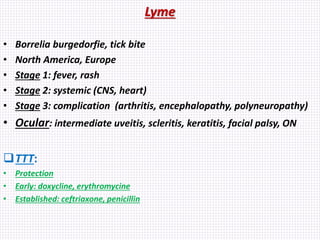
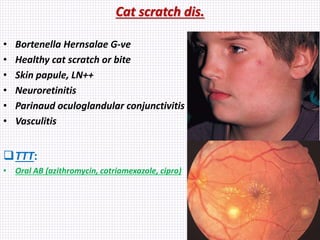
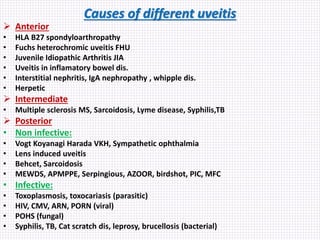
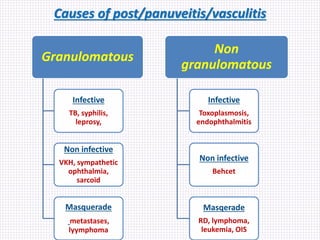
3) The common causes of different types of uveitis including infectious (viral, bacterial, fungal, parasitic) and non-infectious etiologies with and without systemic associations. Specific causes of anterior, intermediate, and posterior uveitis are