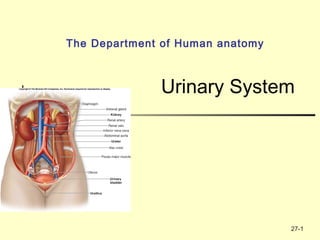
The urinary system develops through three successive phases - the pronephros, mesonephros, and metanephros. The pronephros is nonfunctional in mammals. The mesonephros allows for filtration of blood into mesonephric tubules. During the fifth week of gestation, the ureteric bud induces nearby mesoderm to form the metanephros, or permanent kidneys. The kidneys filter waste from the blood to form urine, which drains via the ureters into the bladder and is then excreted through the urethra. The basic functional unit of the kidneys is the nephron, which filters the blood and reabsorbs necessary molecules