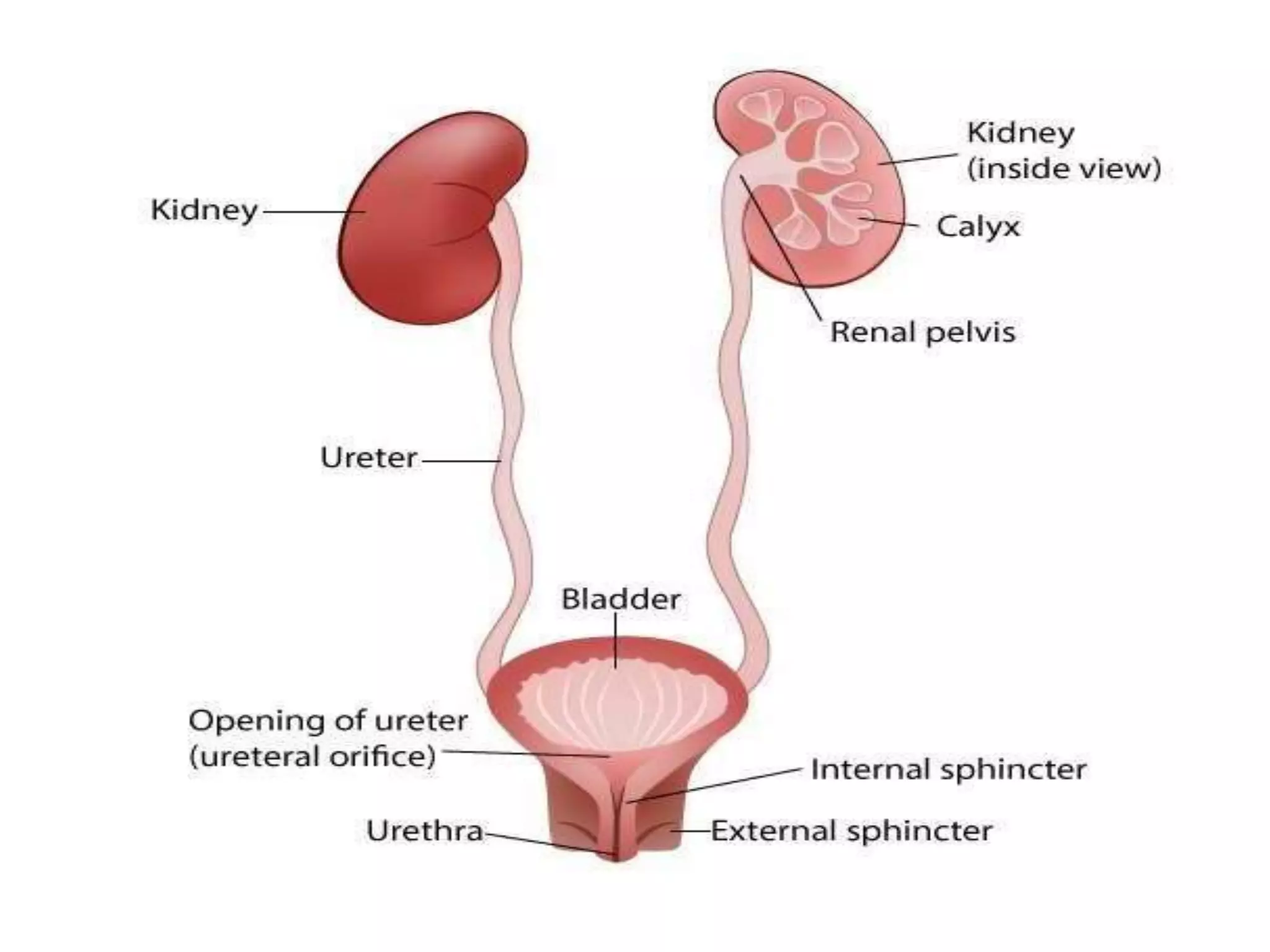
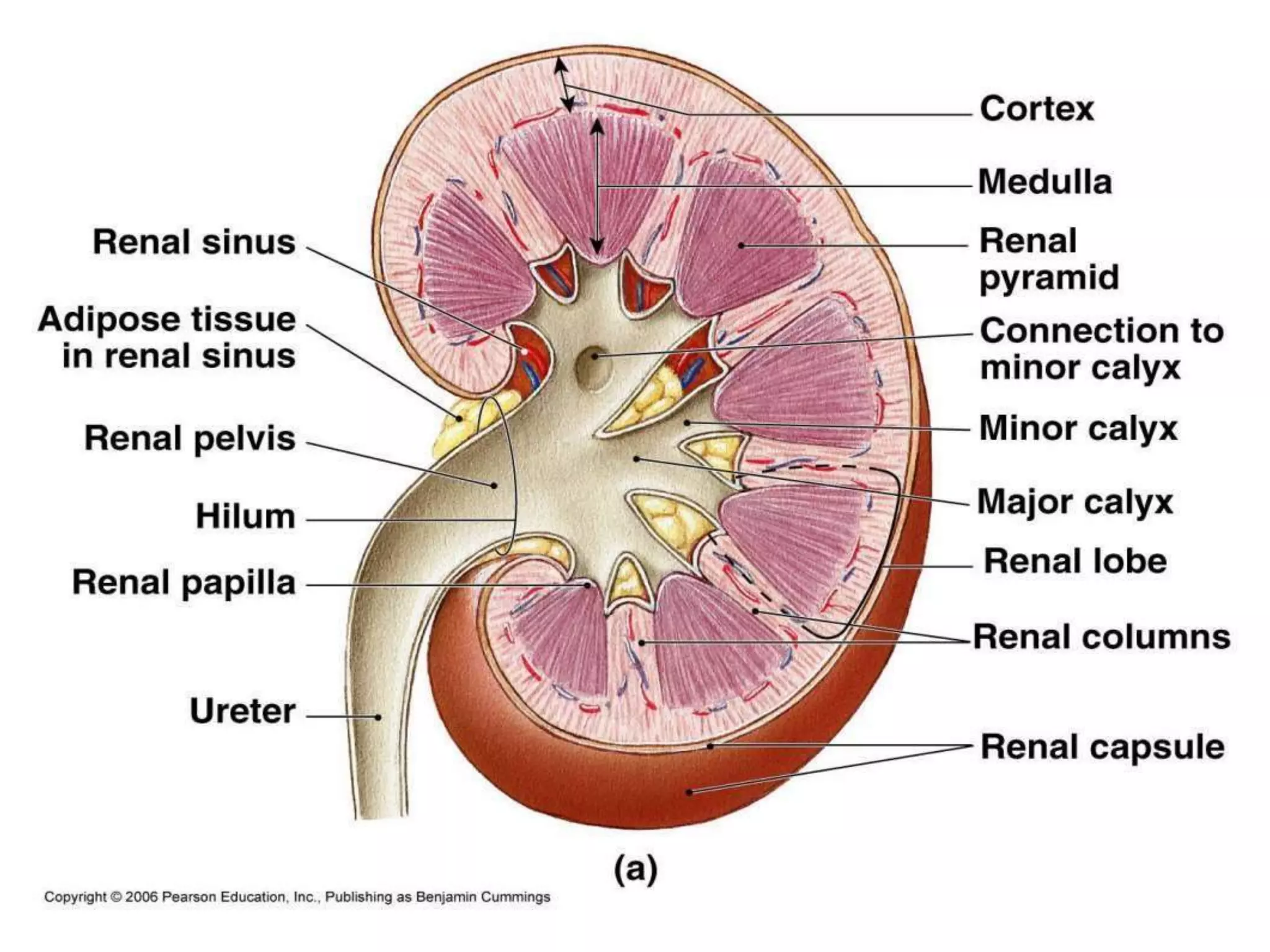
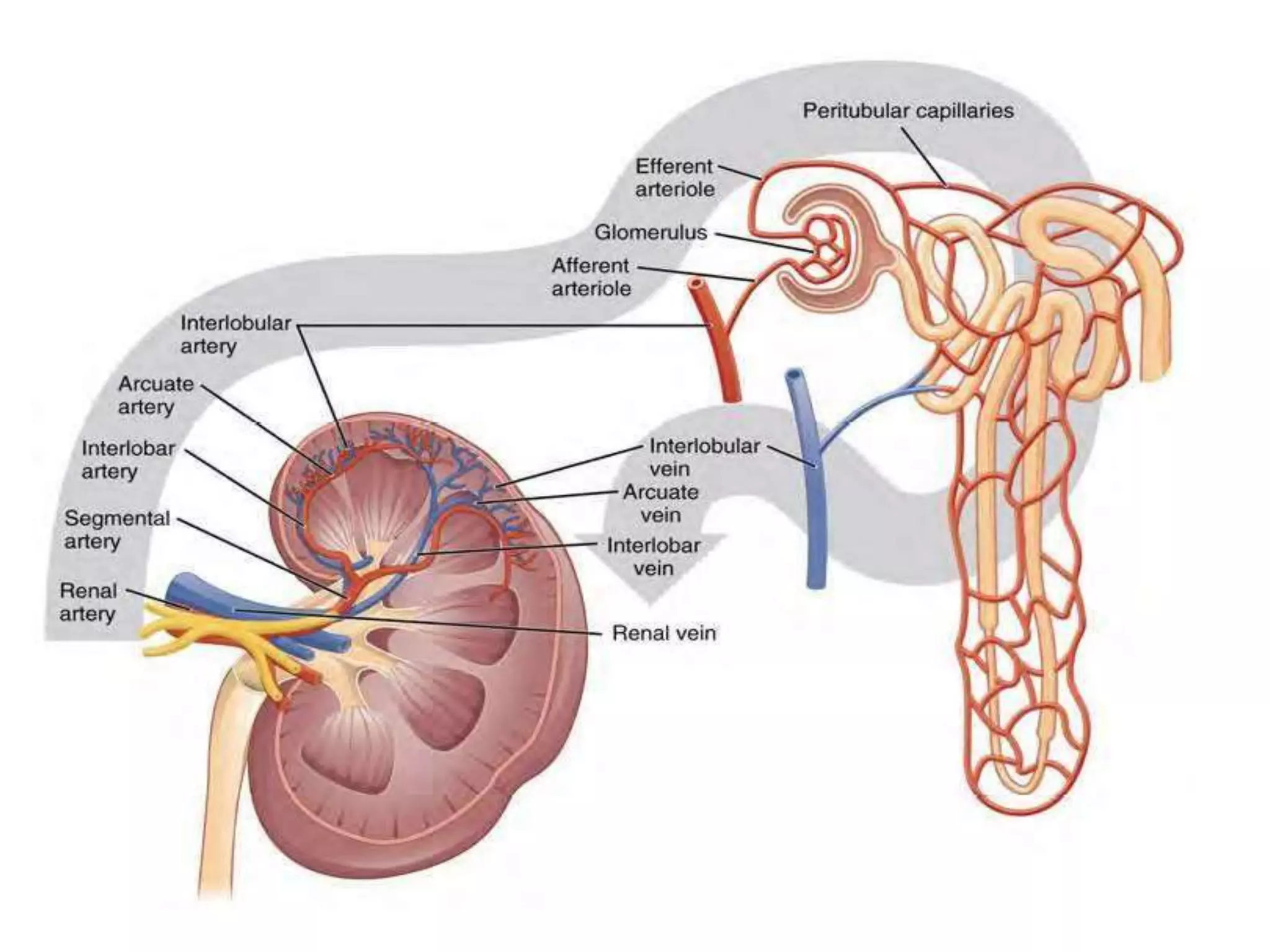
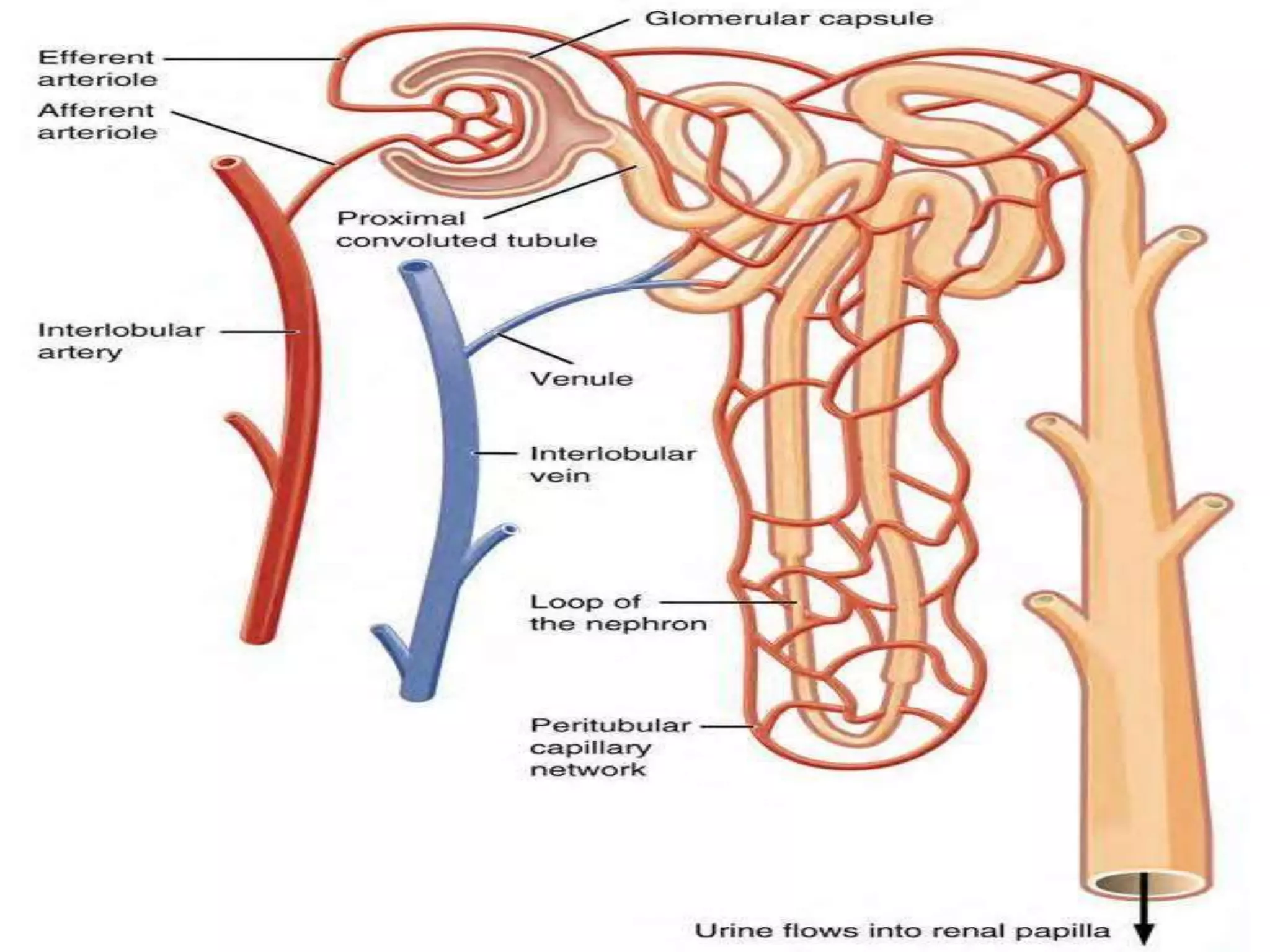
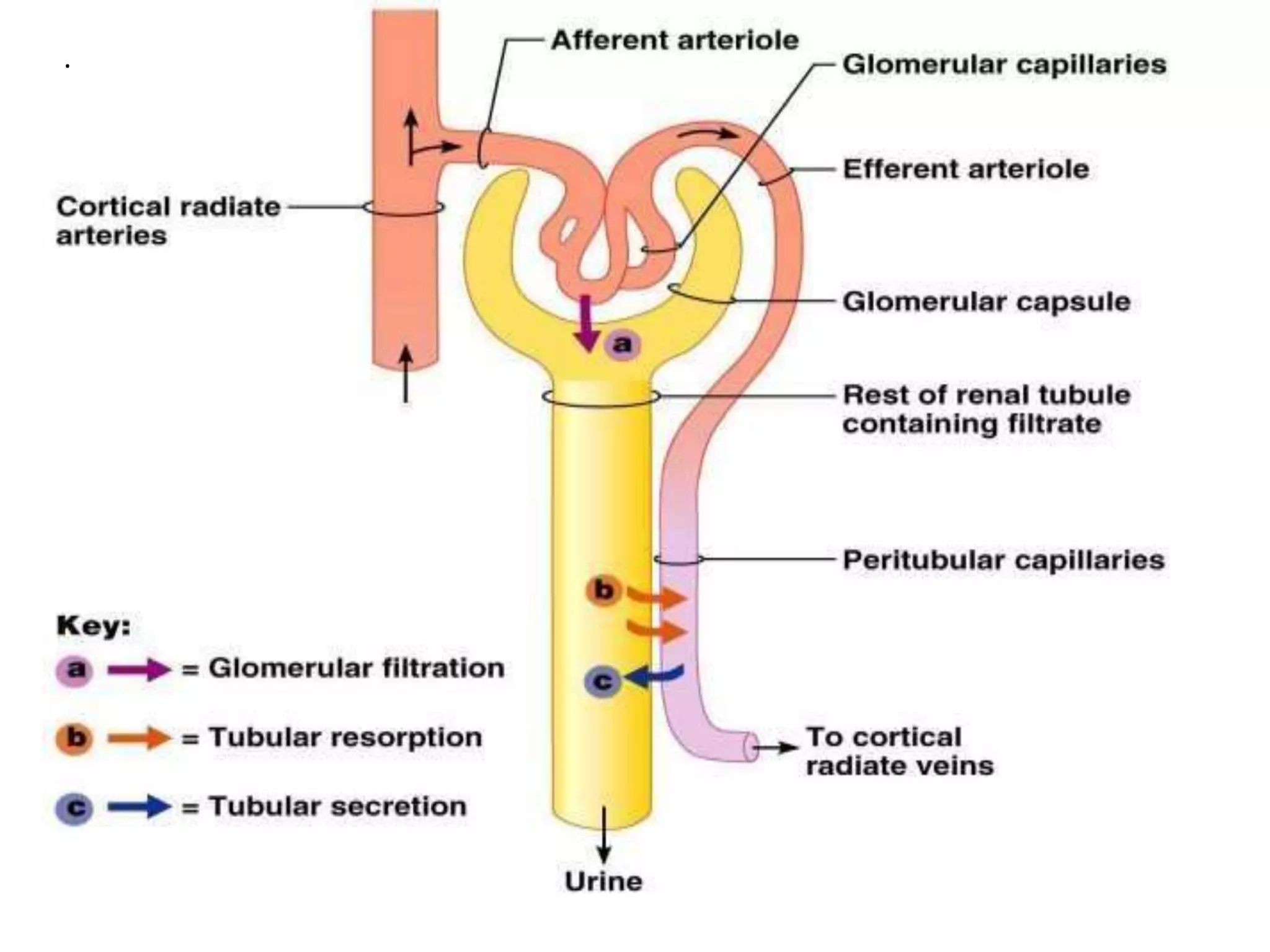
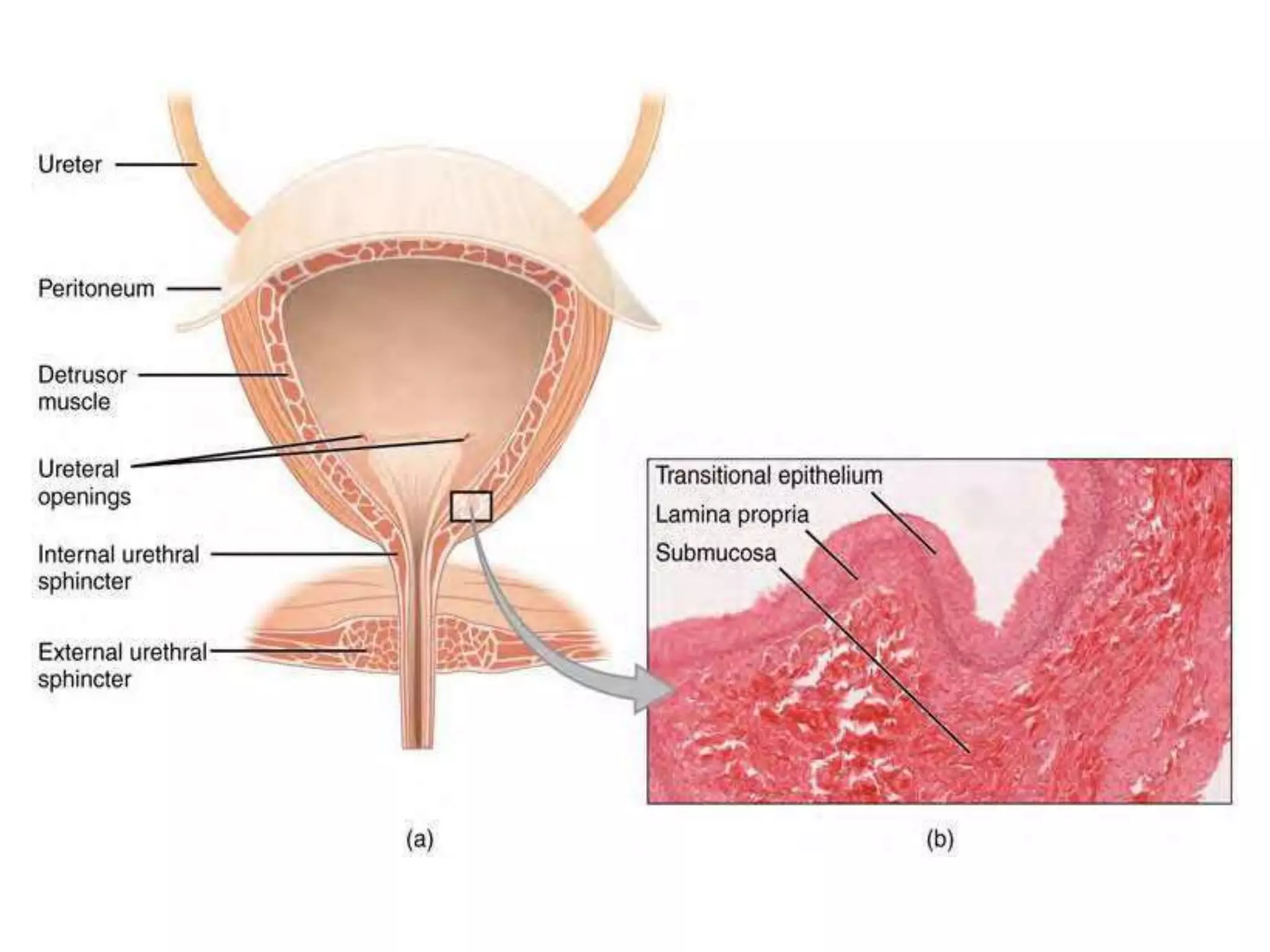
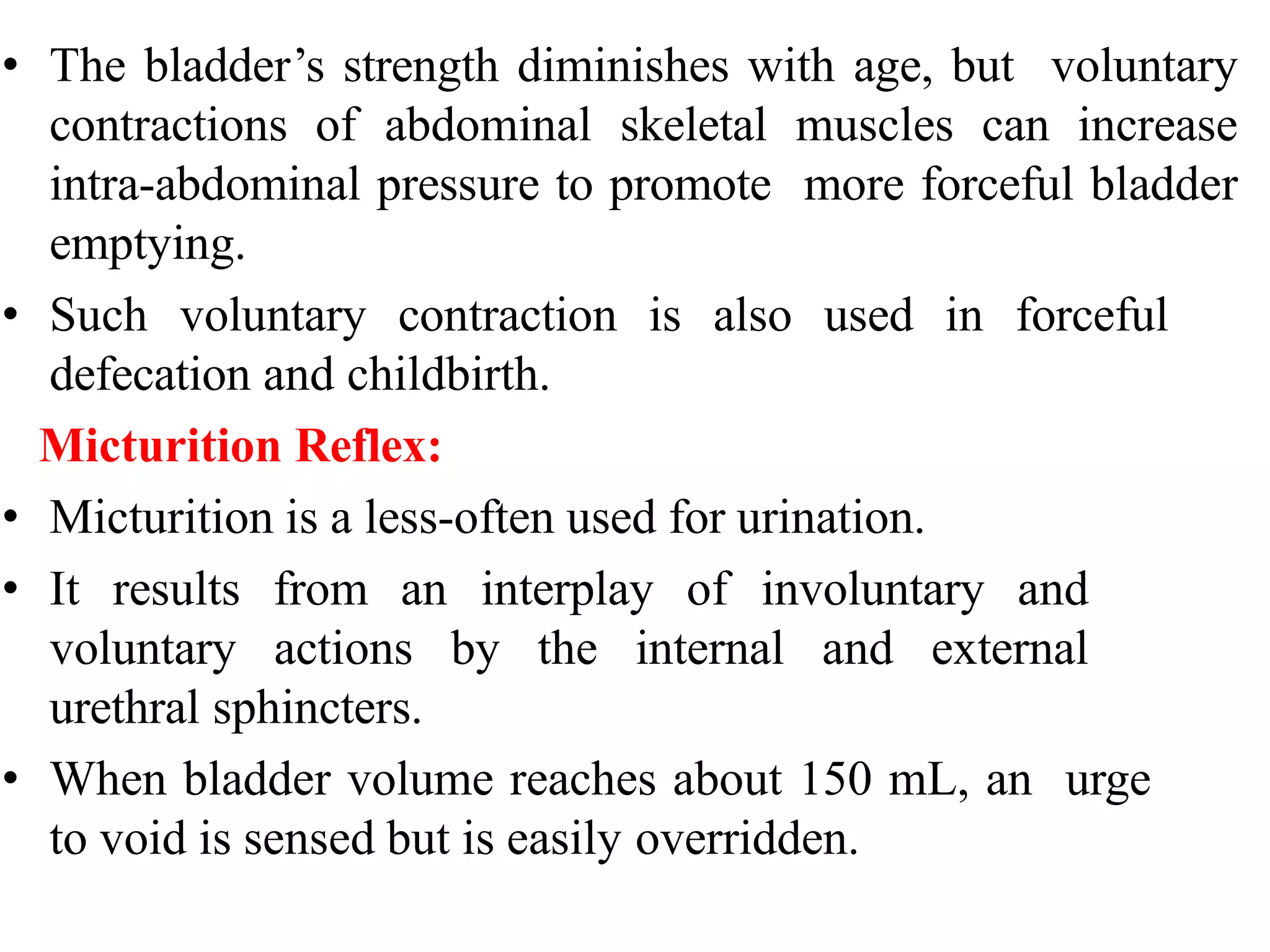
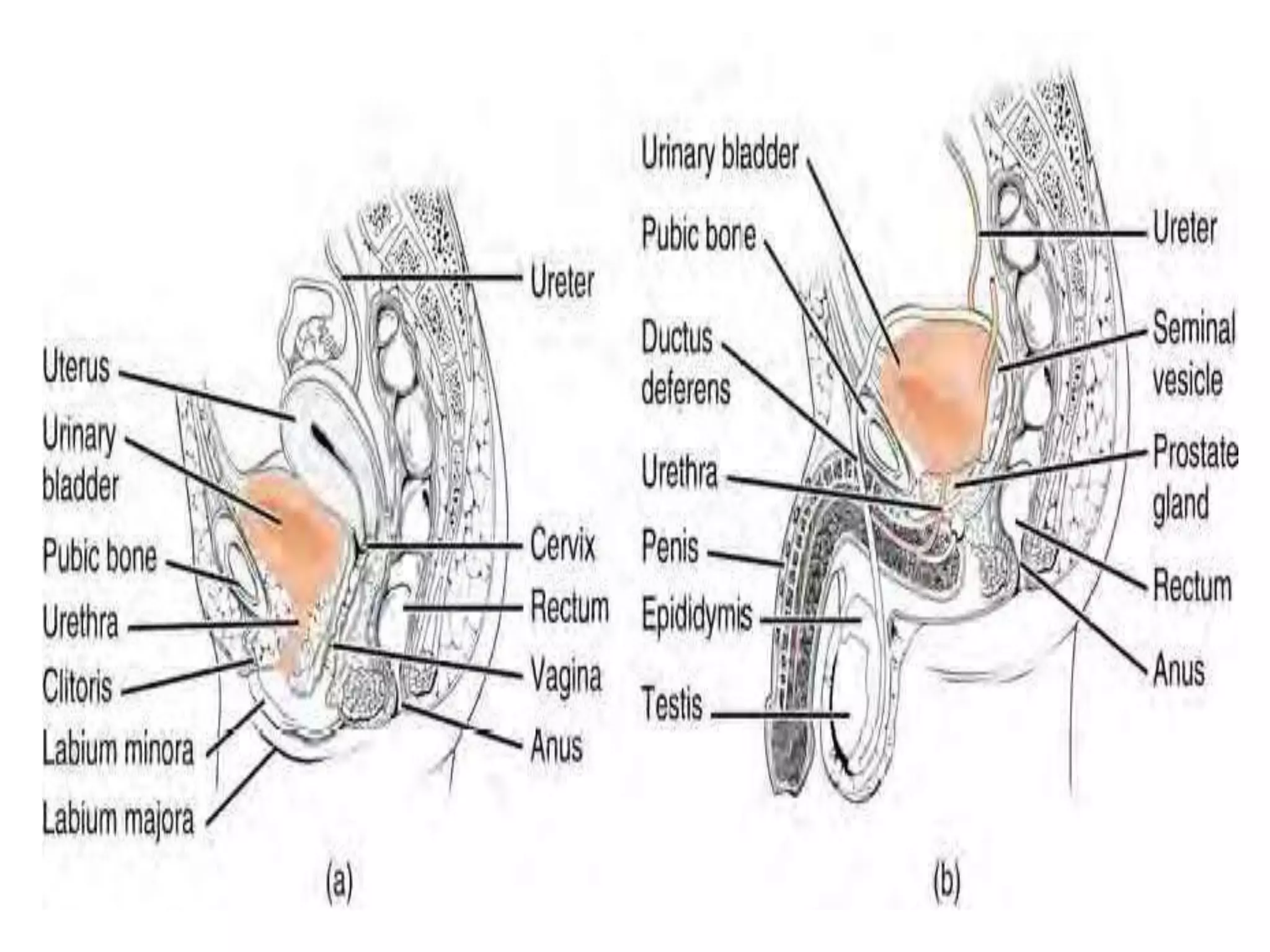
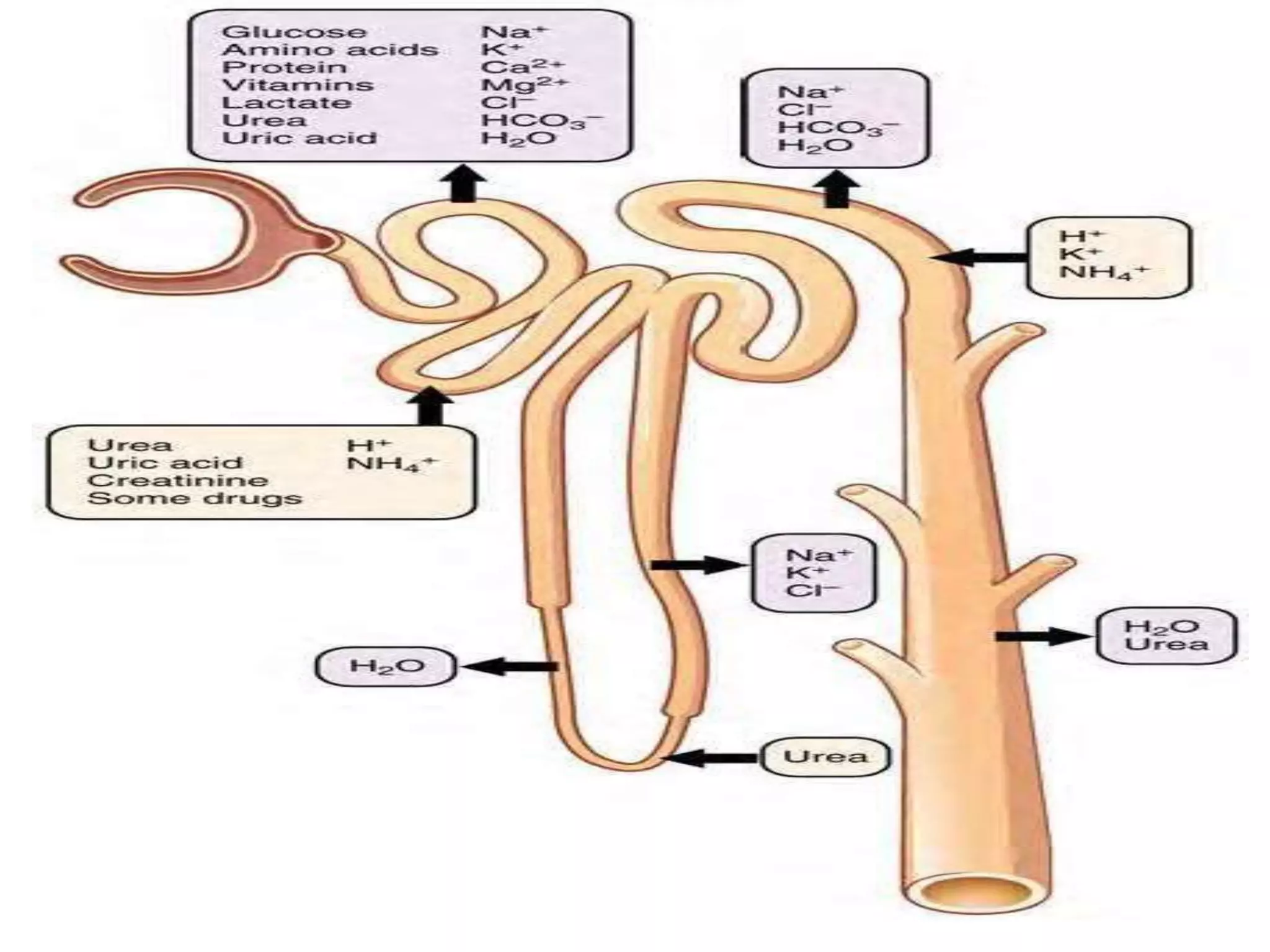
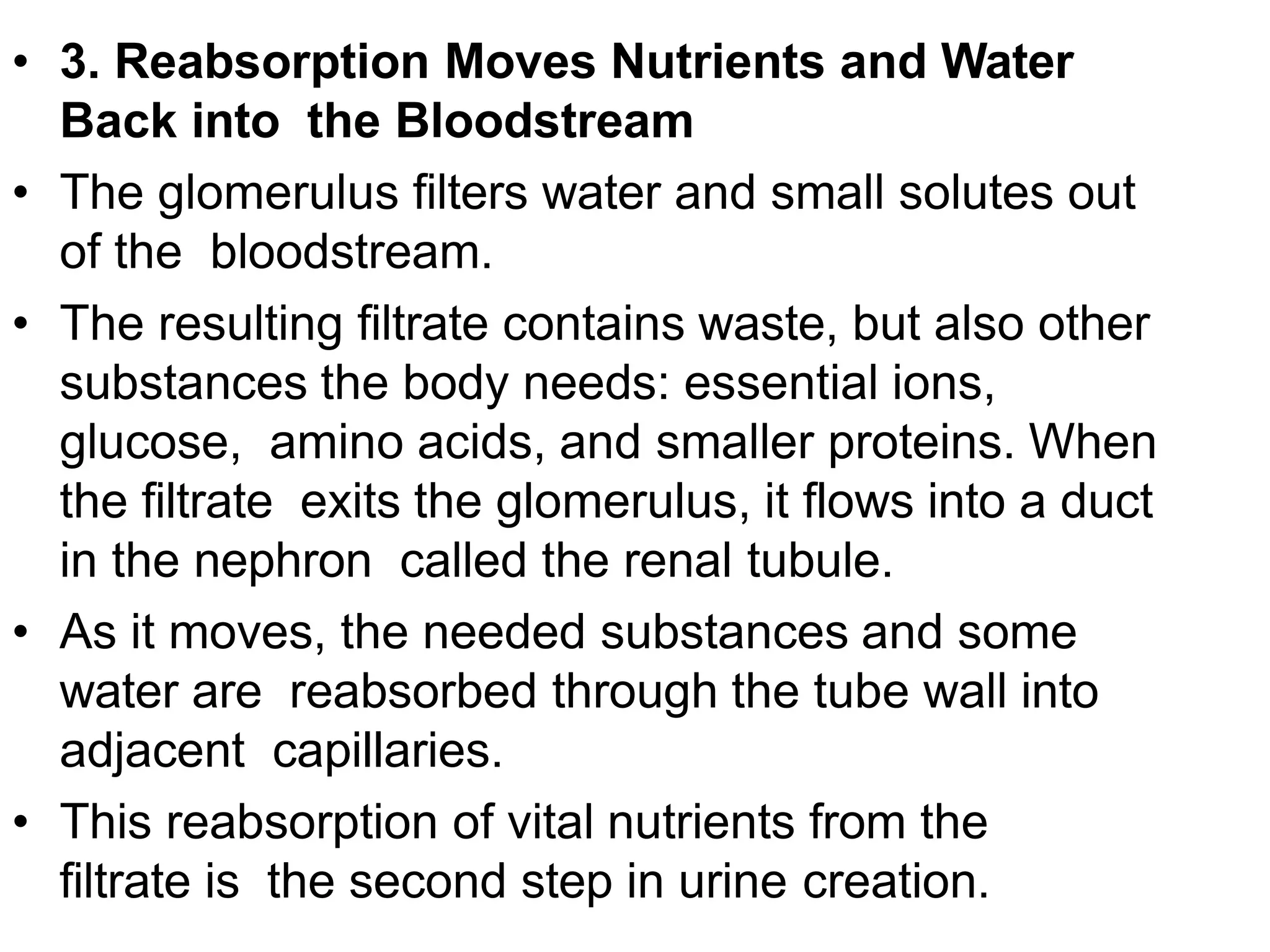
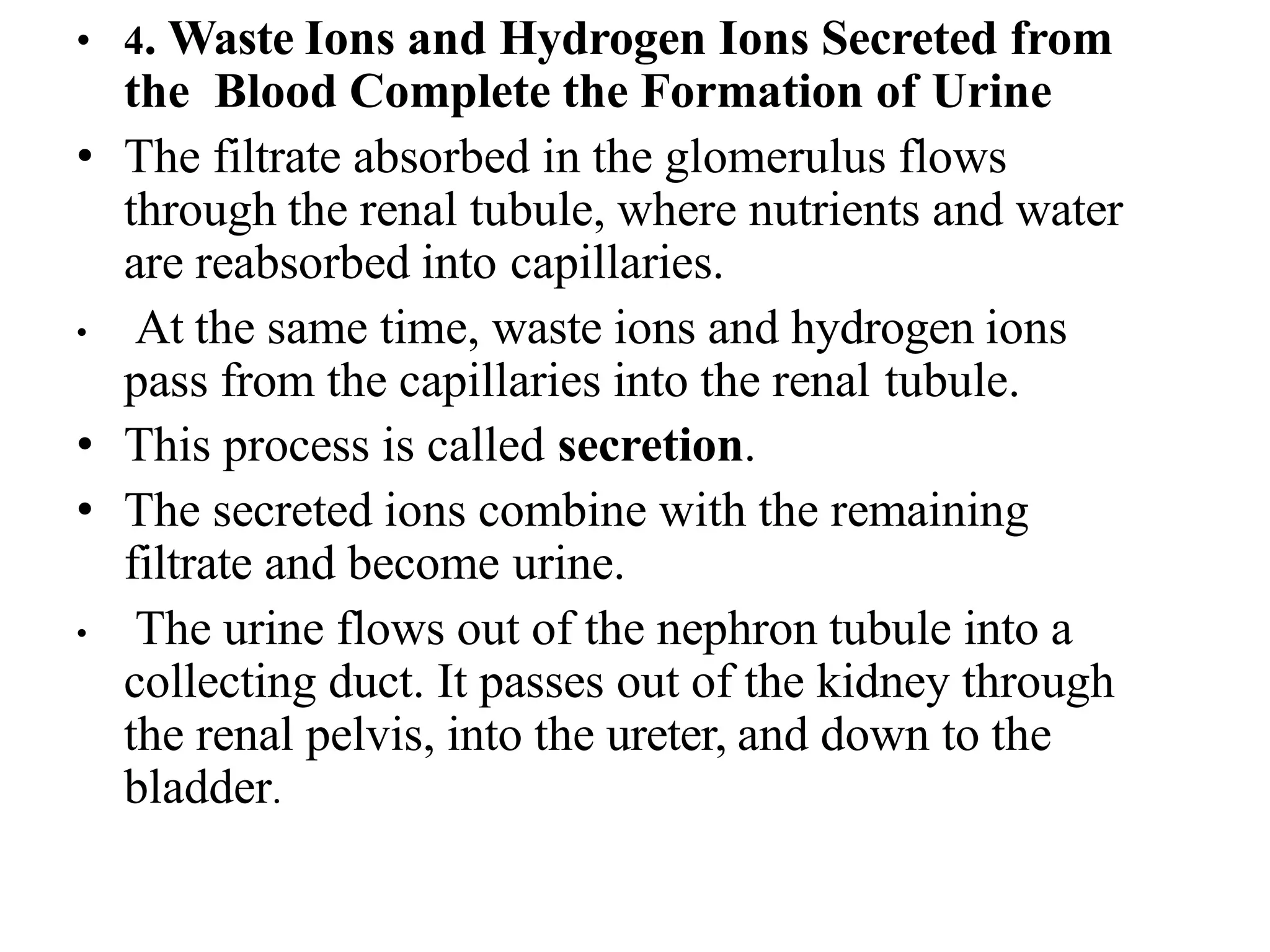
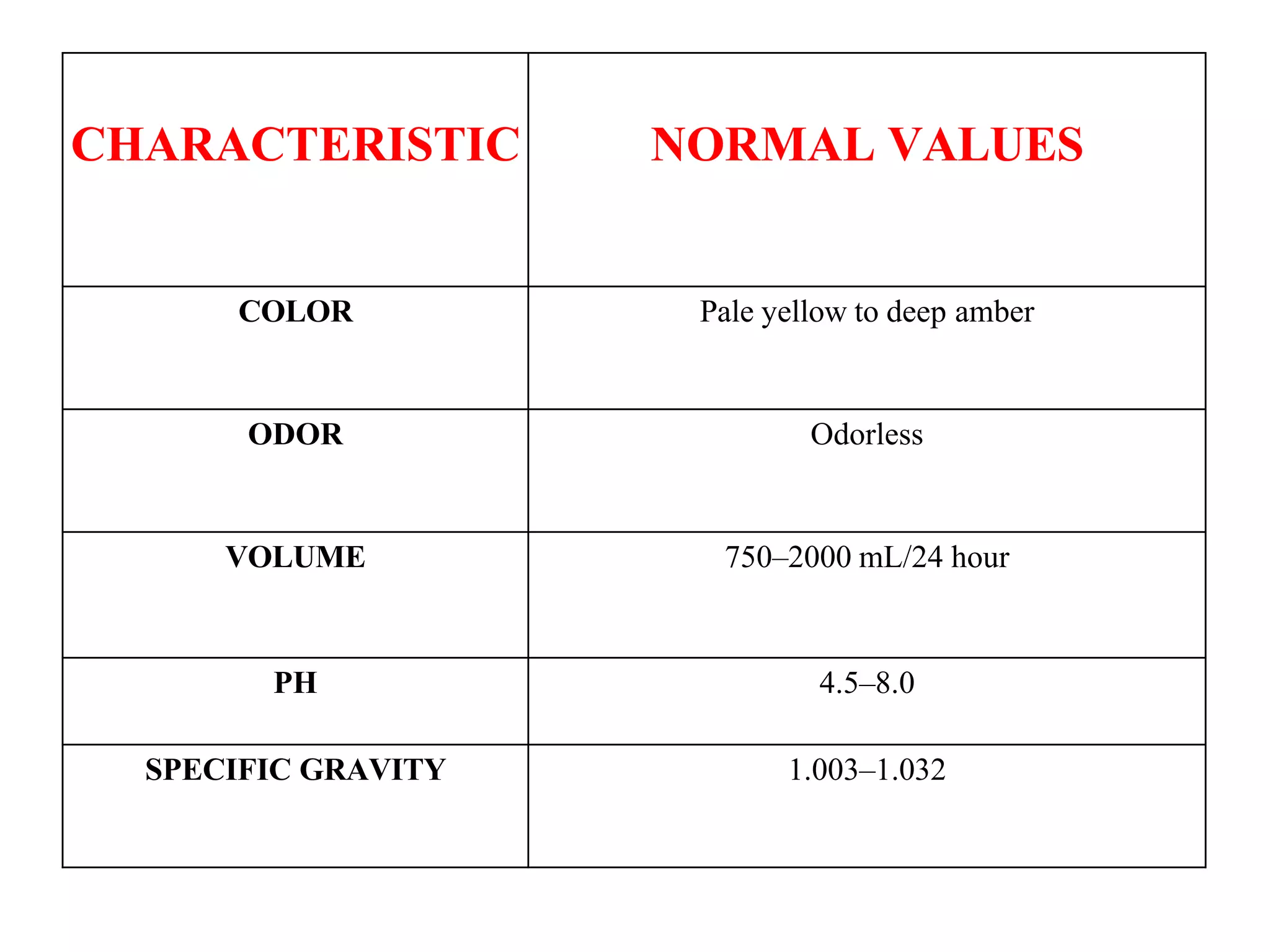
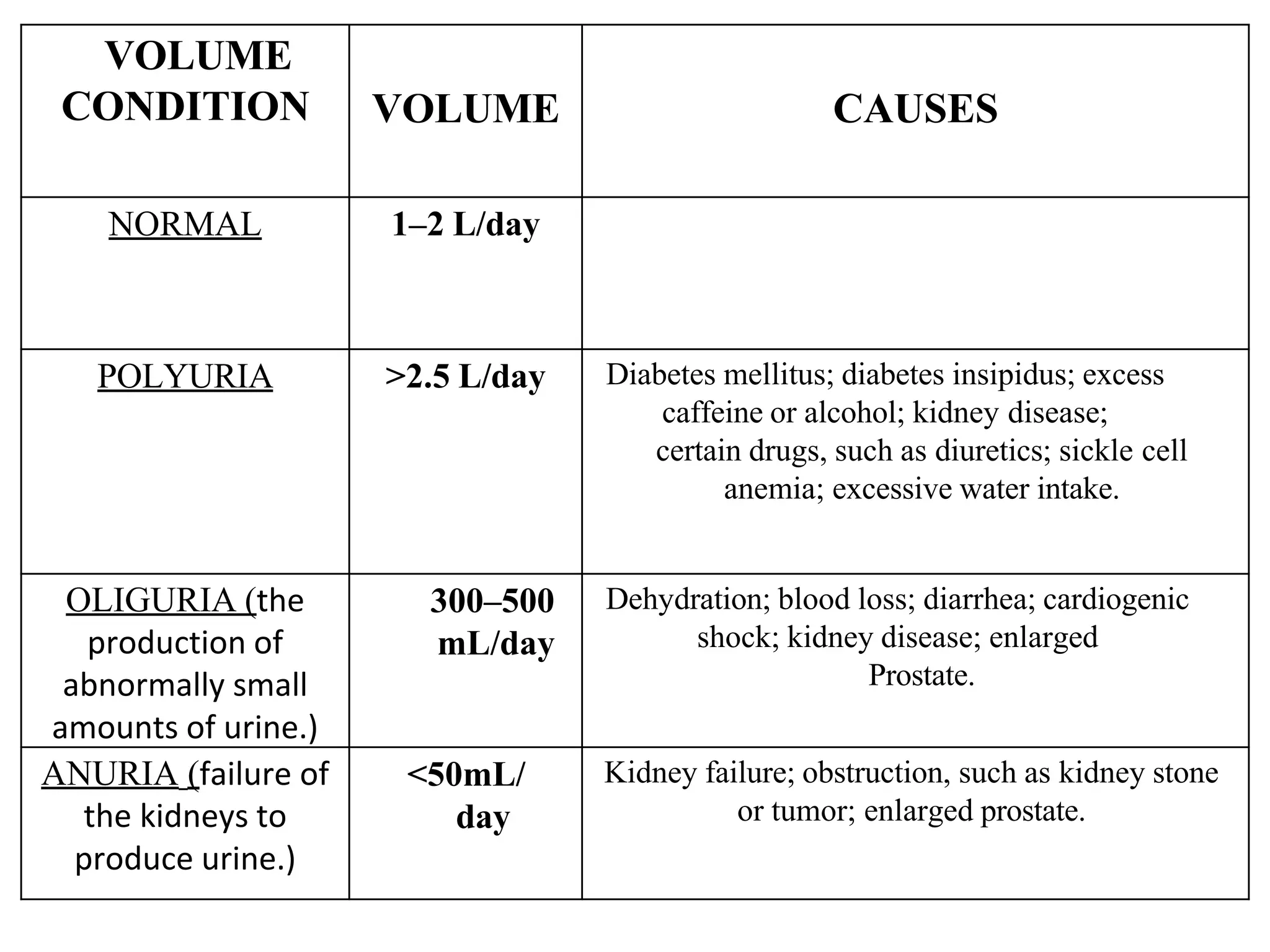
The document provides a comprehensive overview of the urinary system, outlining its components, functions, and structure, including the kidneys, ureters, bladder, and urethra. It details the role of the kidneys in waste removal, electrolyte regulation, blood volume, and blood pressure, as well as the nephron's function in urine formation through filtration, reabsorption, and secretion. Additionally, it discusses the physical characteristics of urine and the hormonal regulation of kidney function.