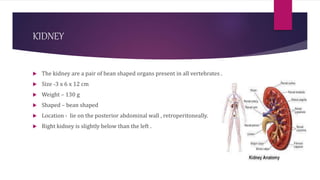
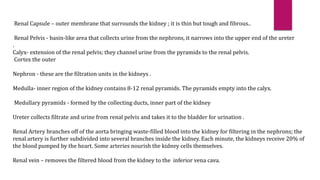
The urinary system consists of the kidneys, ureters, urinary bladder, and urethra. The kidneys filter waste from the blood to produce urine. Urine travels from the kidneys down the ureters into the urinary bladder, where it is stored until urination. The urethra then carries urine from the bladder out of the body. The kidneys contain nephrons, which filter the blood, reabsorb useful substances, and secrete waste products to form urine and maintain homeostasis.