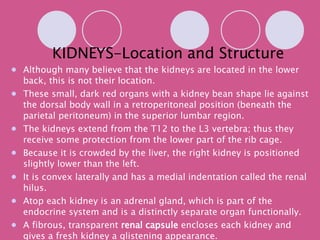
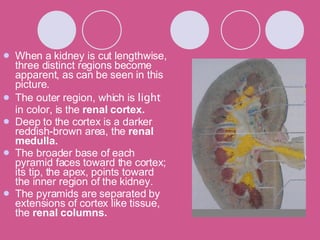
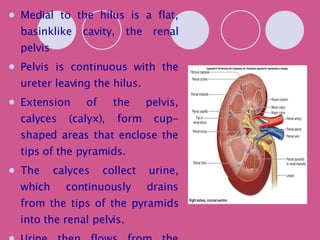
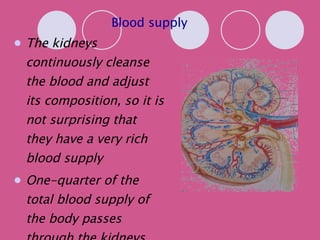
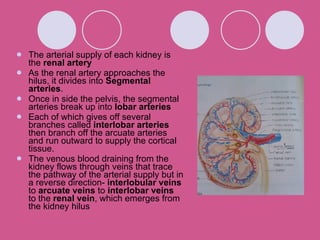
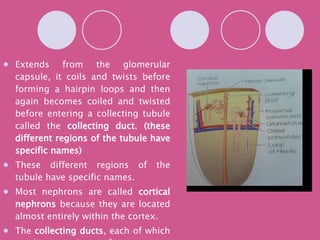
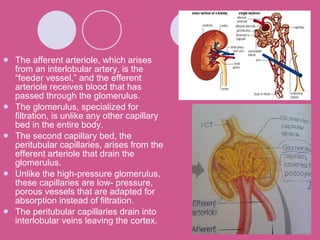
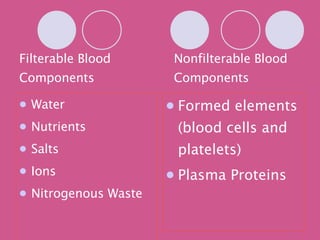
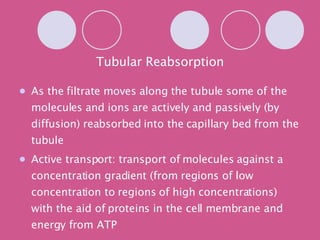
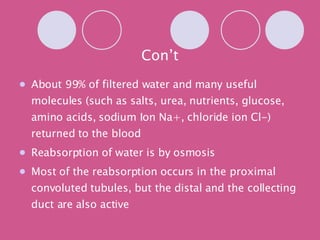
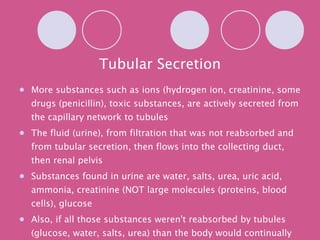
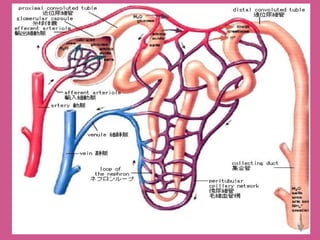
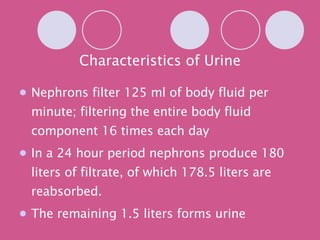
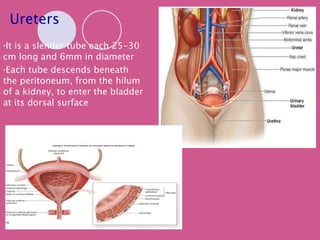
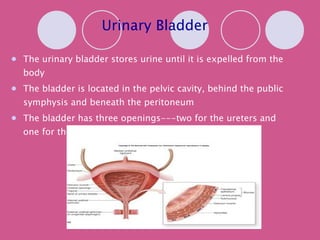
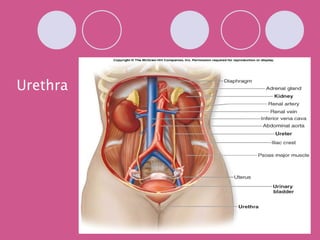
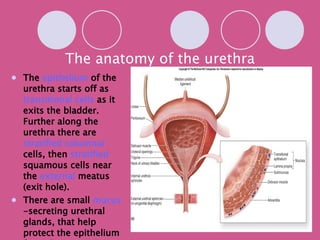
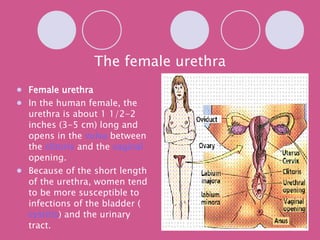
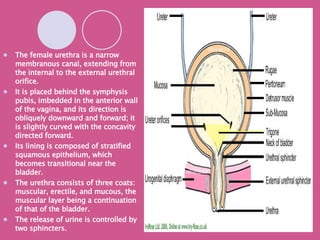
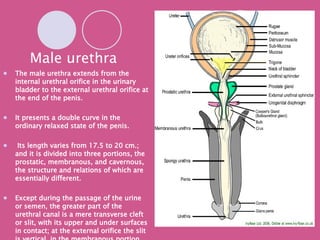
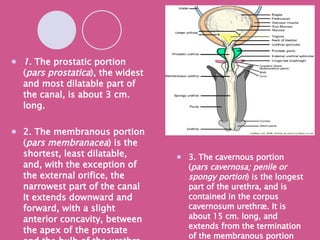
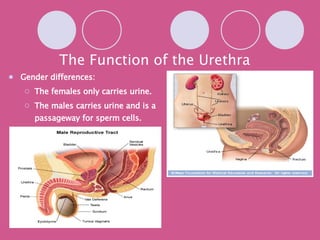
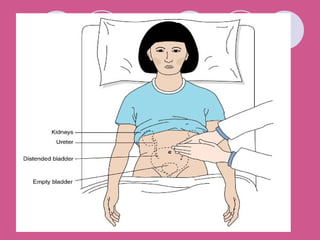
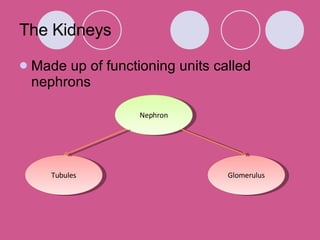
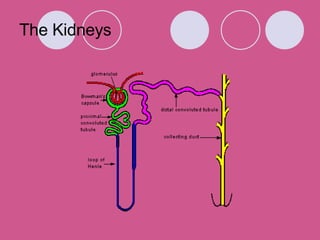
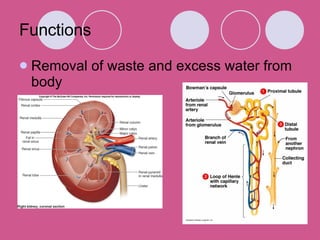
The document provides detailed information about the structure and function of the urinary system. It describes the location and structure of the kidneys and discusses nephrons, filtration, reabsorption, and secretion in urine formation. It also outlines the pathways of urine from the kidneys through the ureters to the bladder and urethra, and describes how urine is stored and expelled from the body.









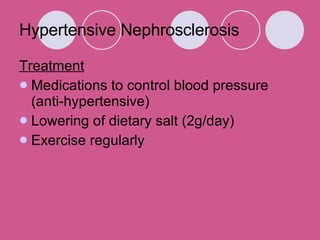


![References Kidney Dialysis Foundation (2007). Normal Kidney Functions. Health Guide [Online]. Available: http://www.kdf.org.sg/health.php (2008, June 01). National Kidney Foundation (2007). Common Kidney Diseases. Education [Online]. Available: http://www.nkfs.org/index.php (2008, June 01).](https://image.slidesharecdn.com/uria-1225008695285067-8/85/Uri-A-119-320.jpg)