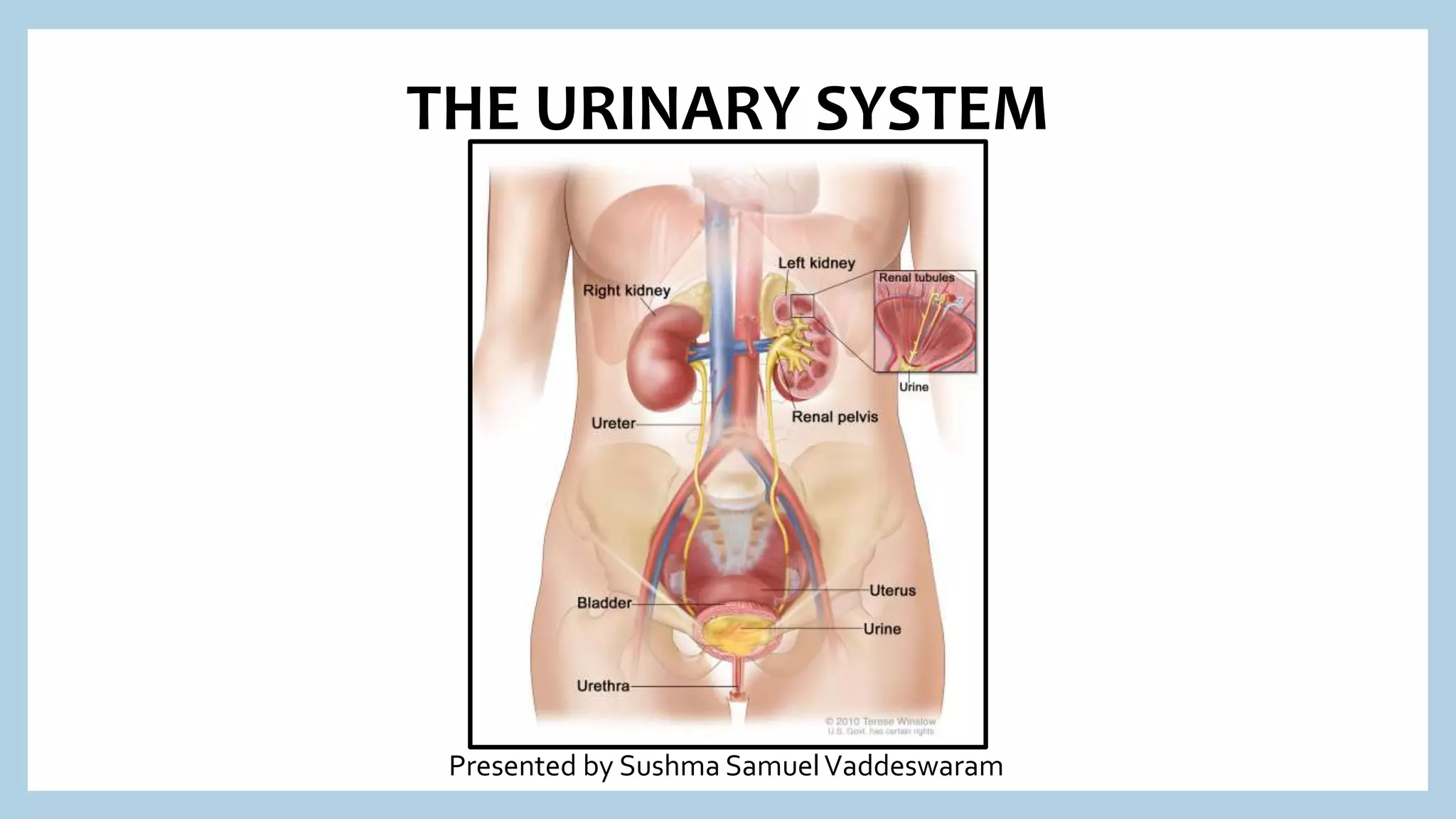
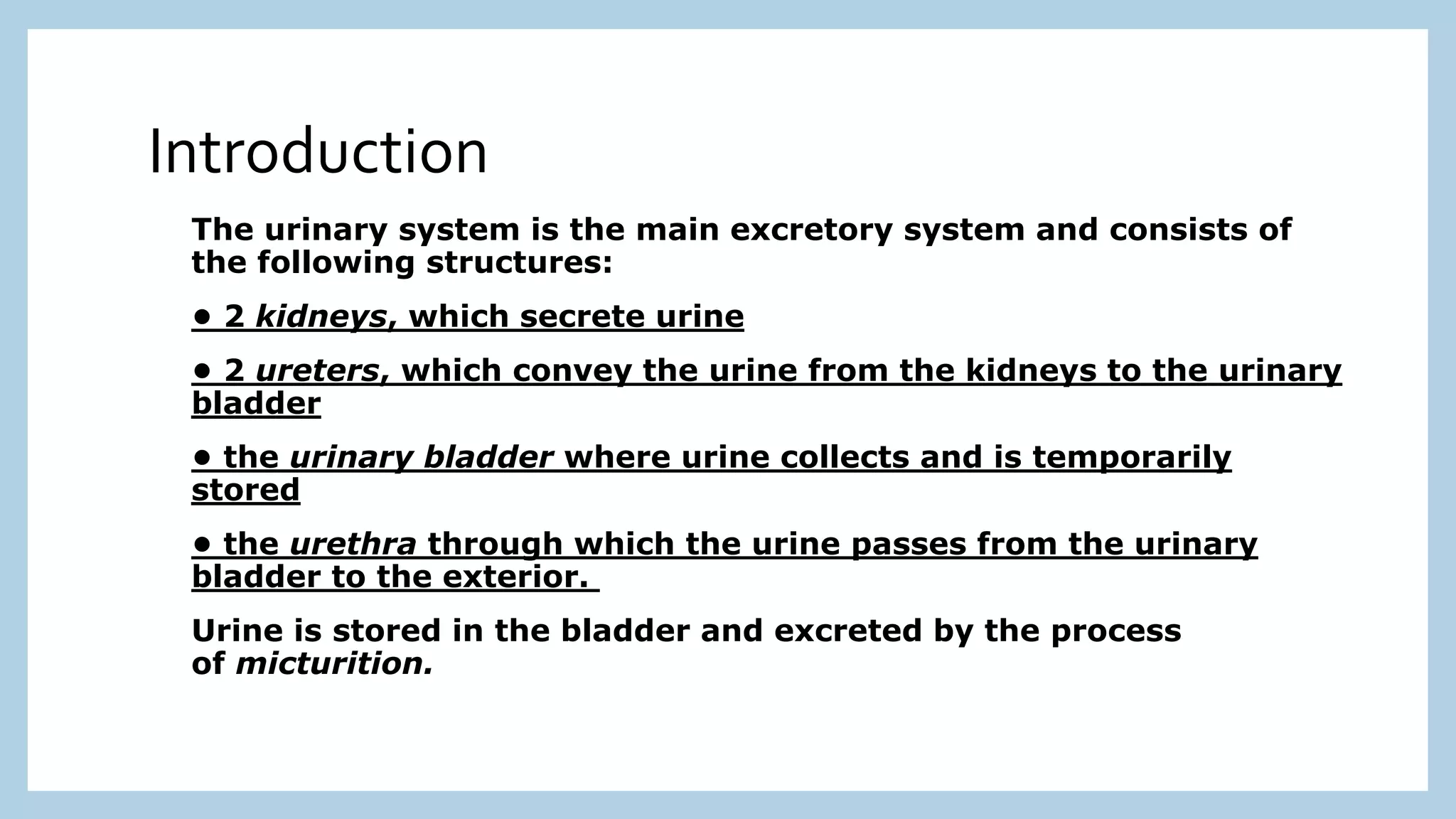
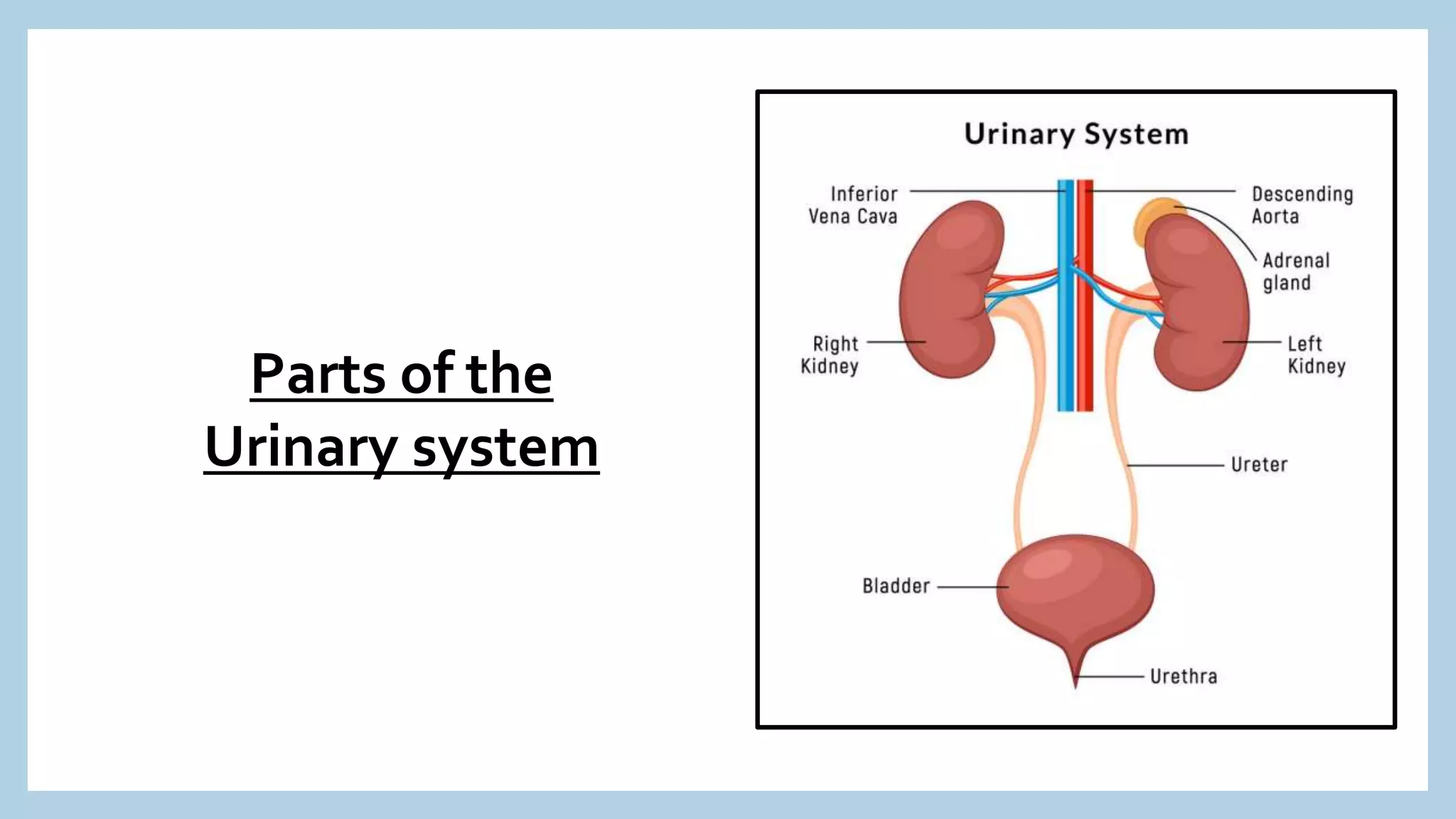
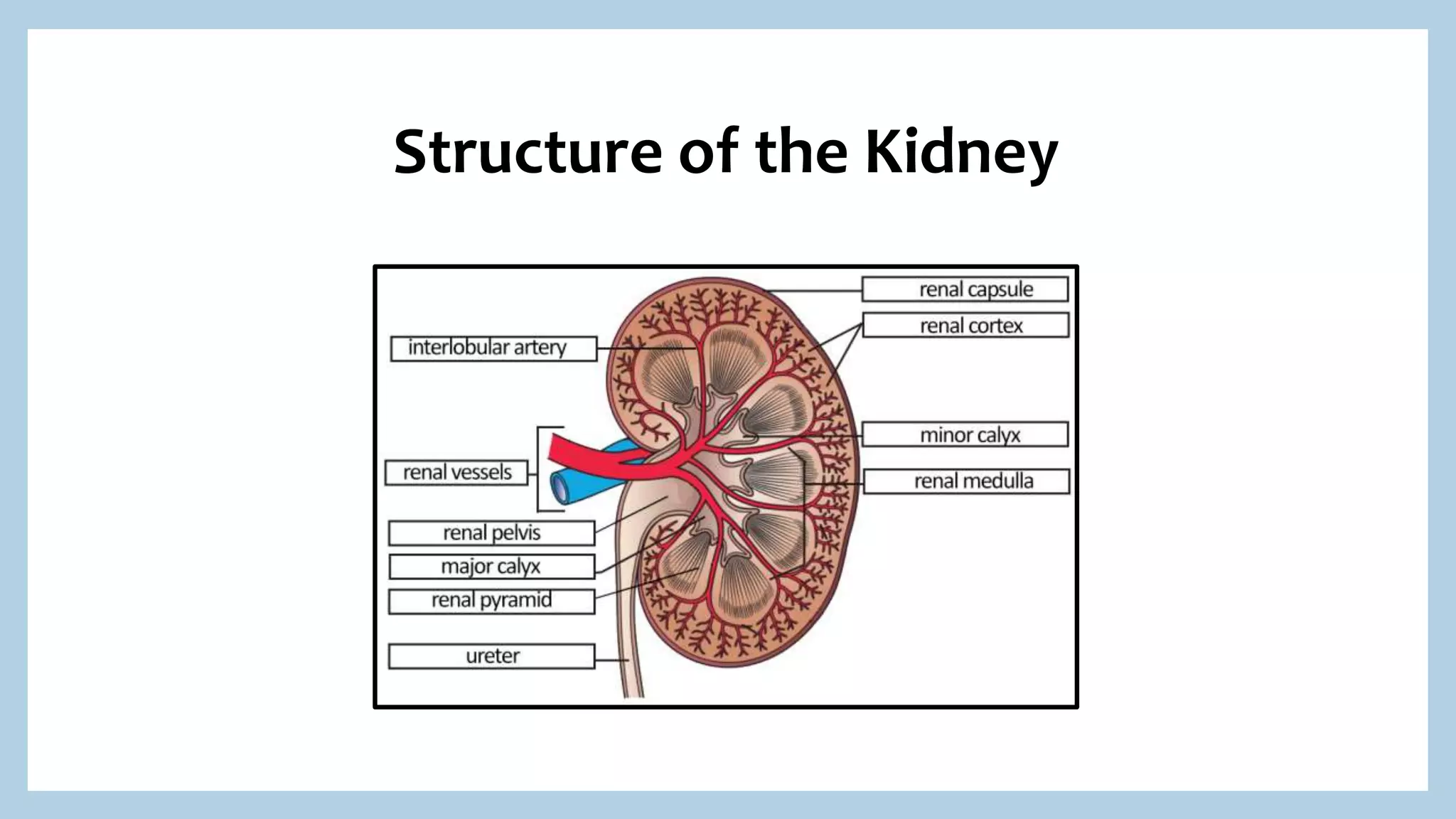
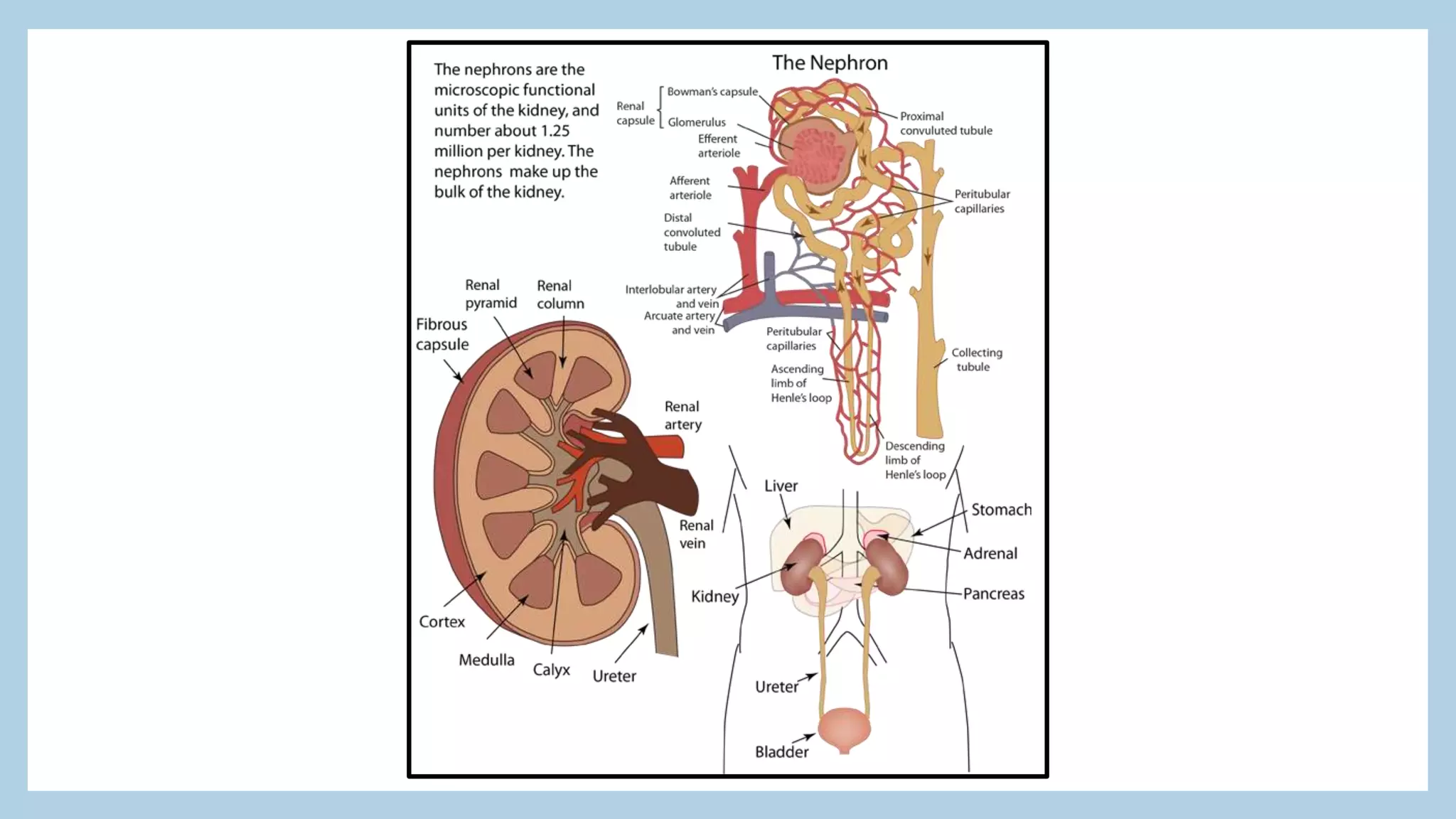
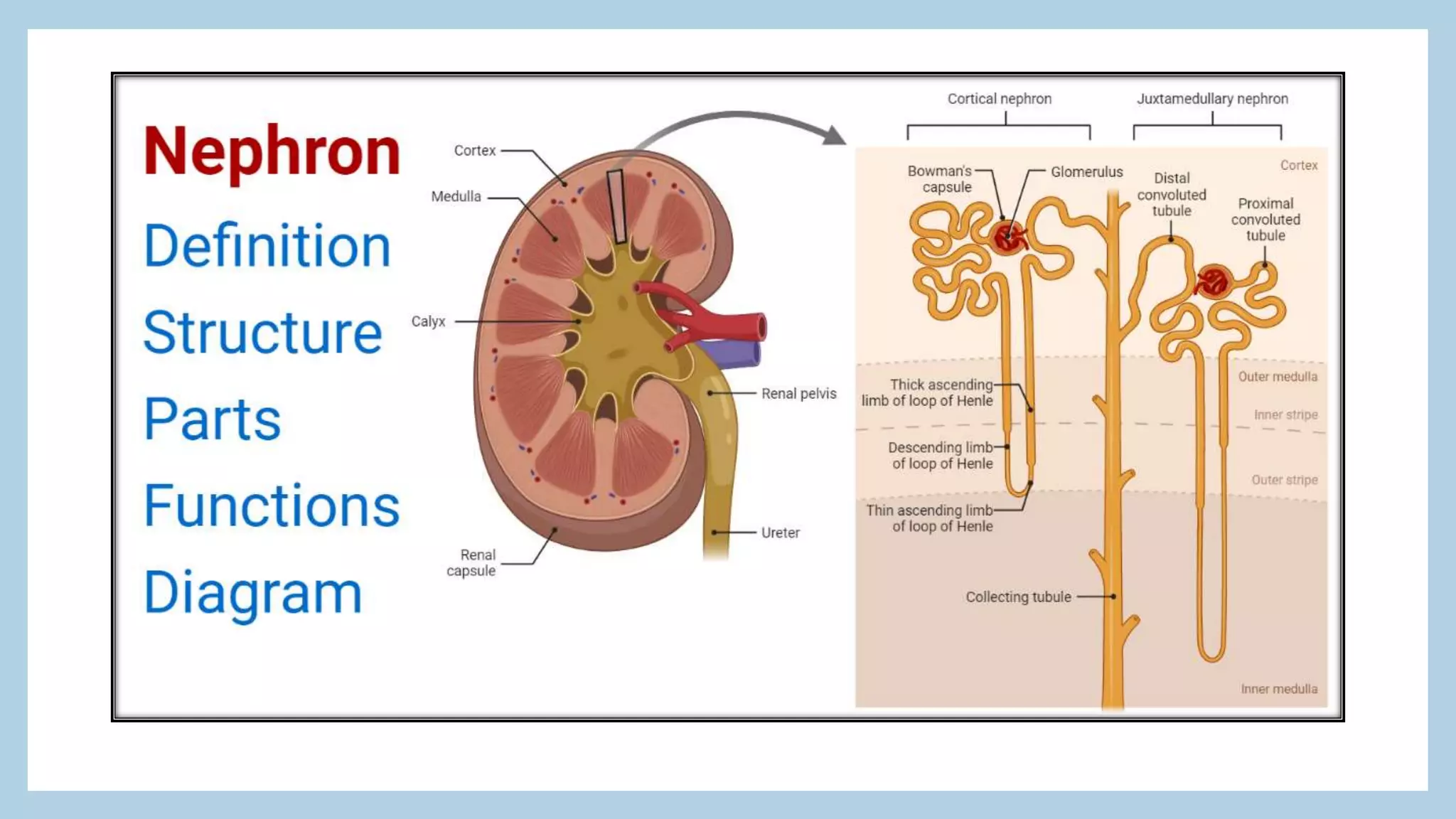
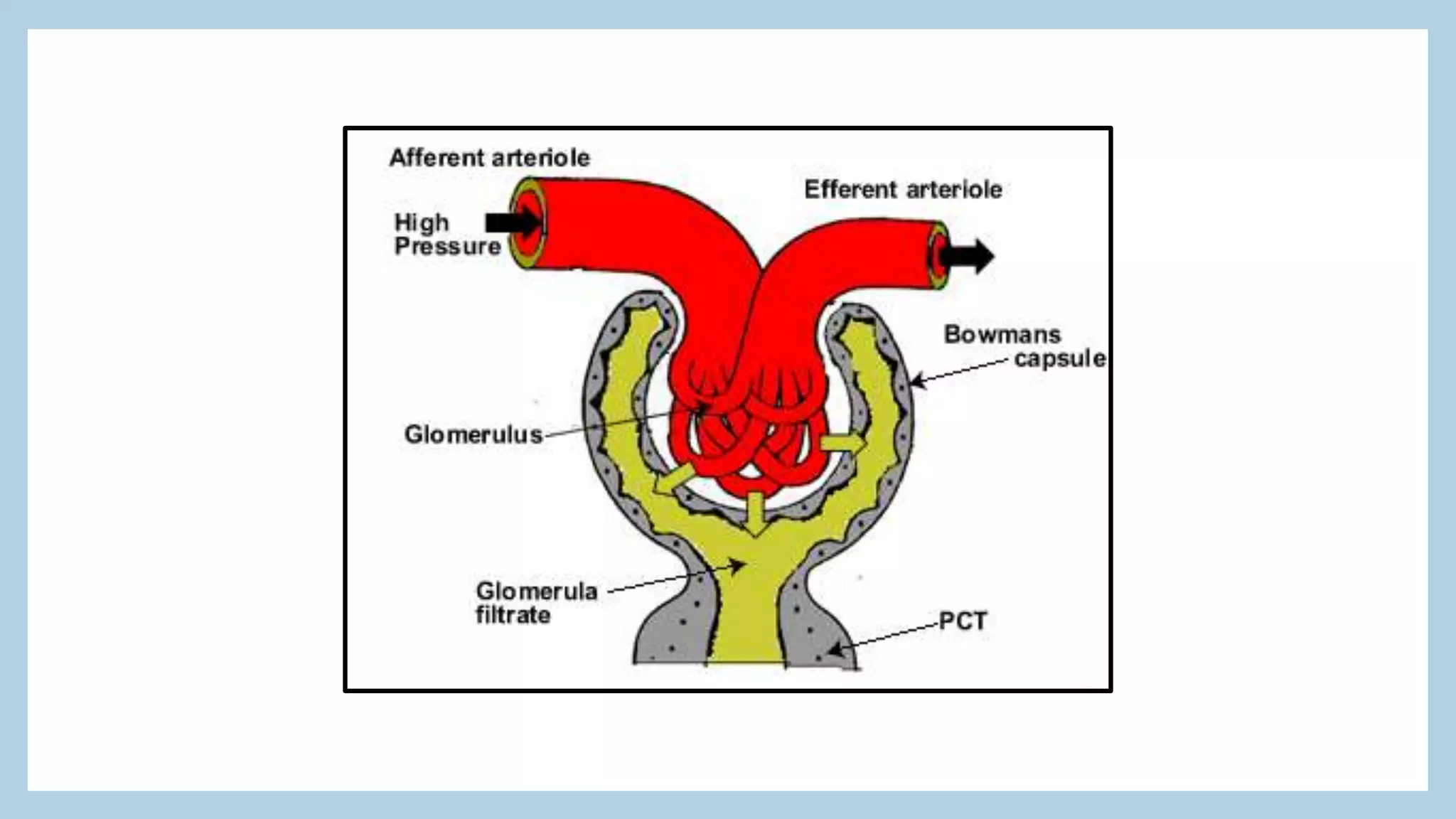
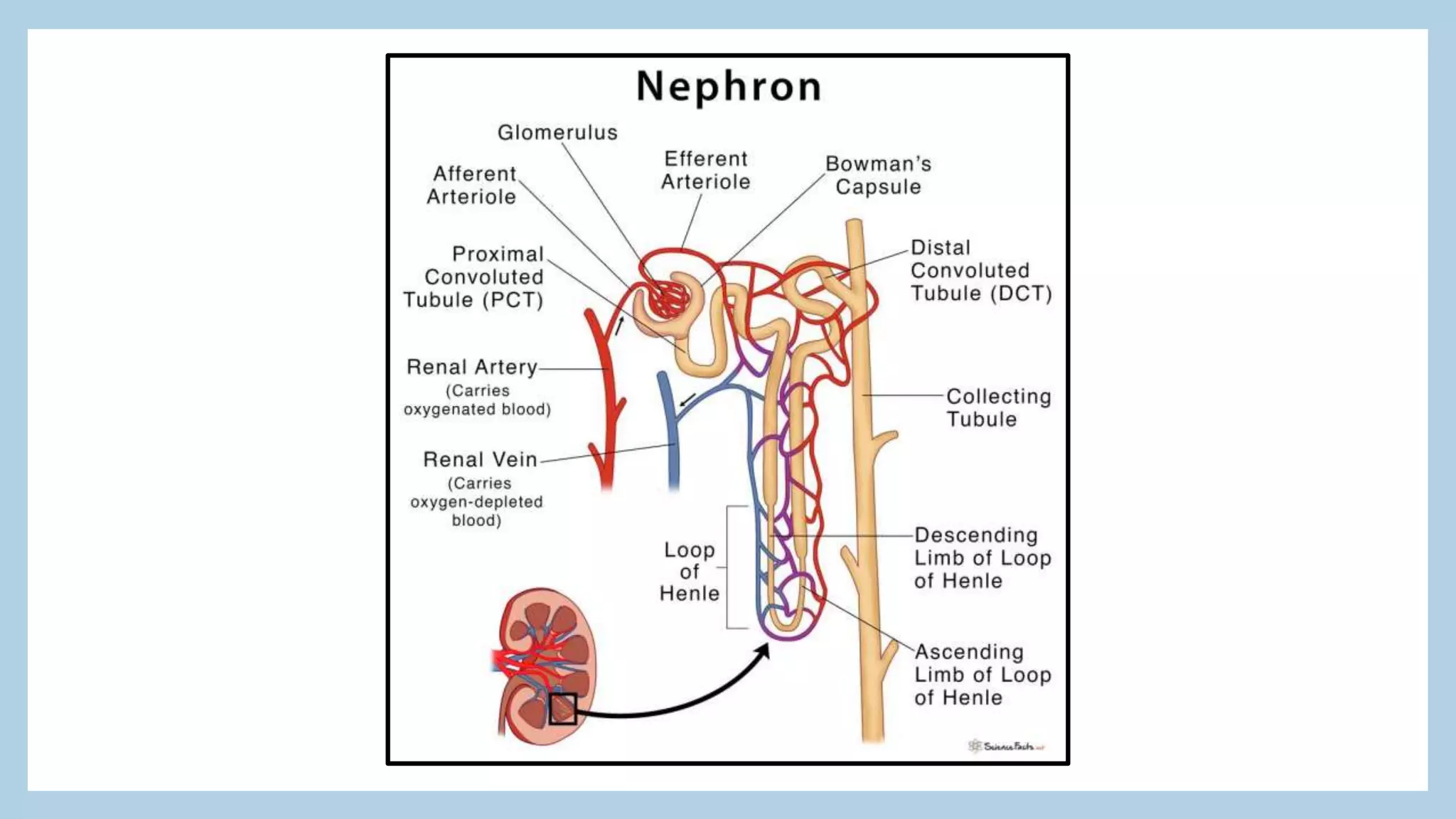
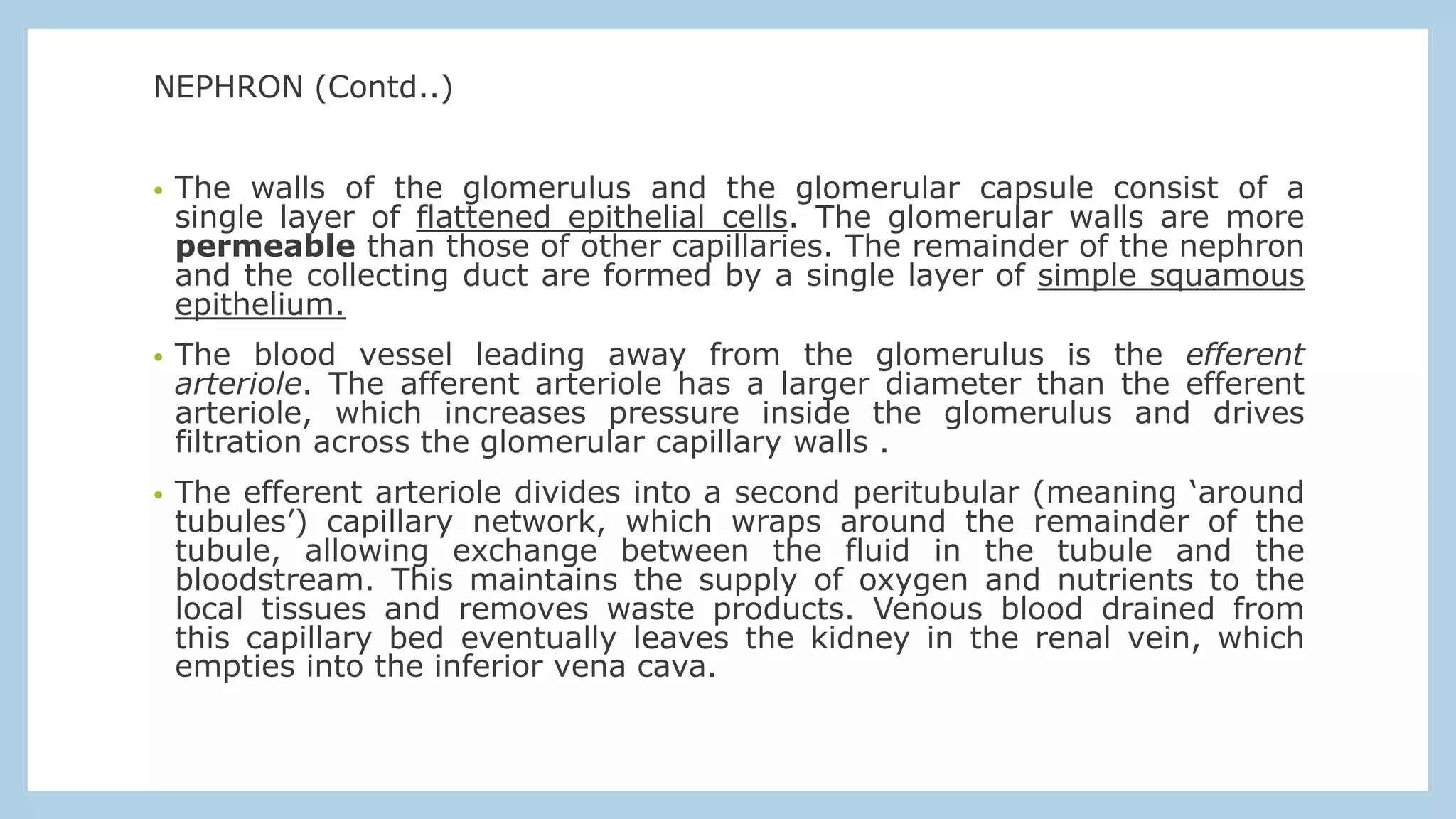
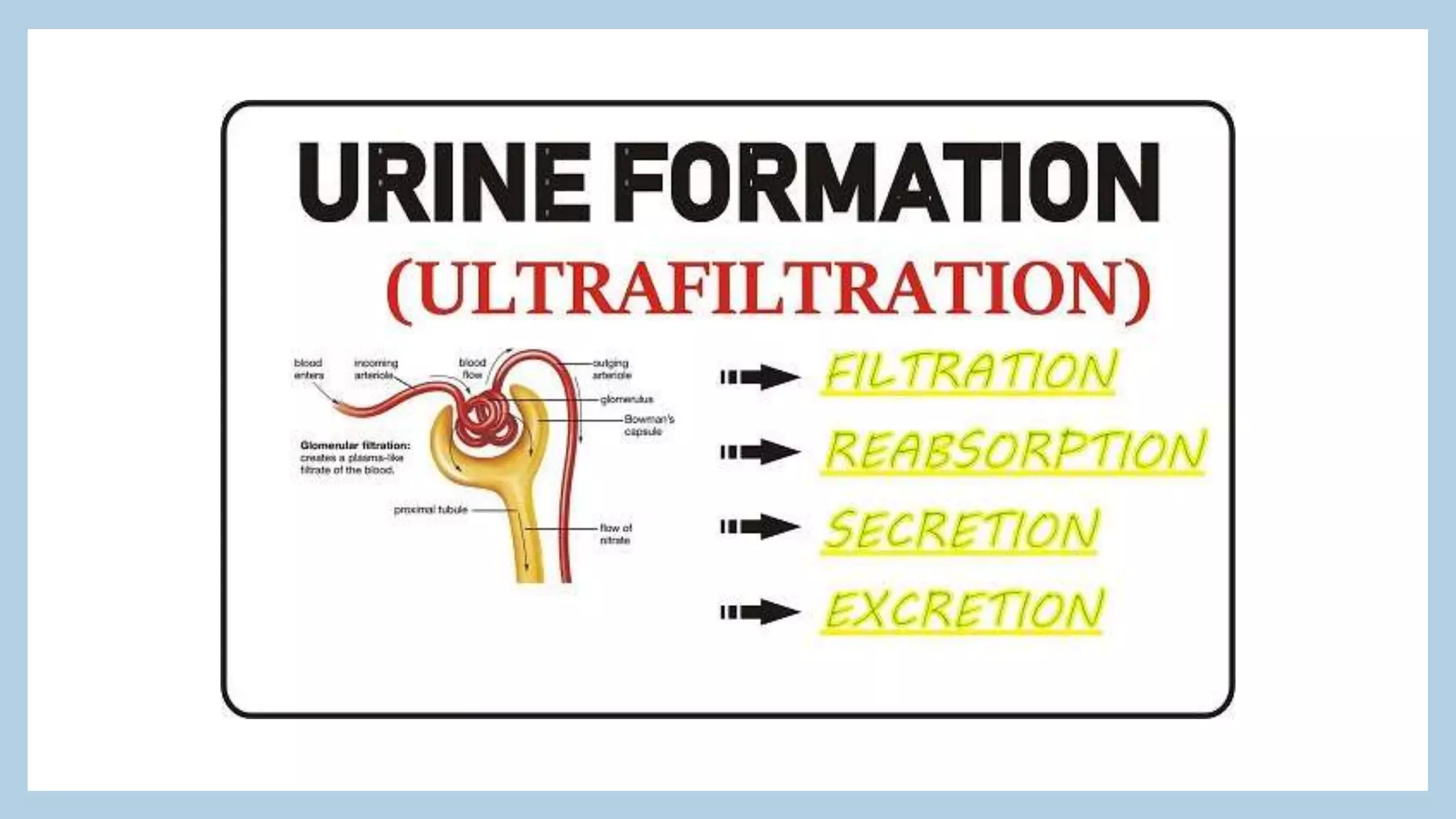
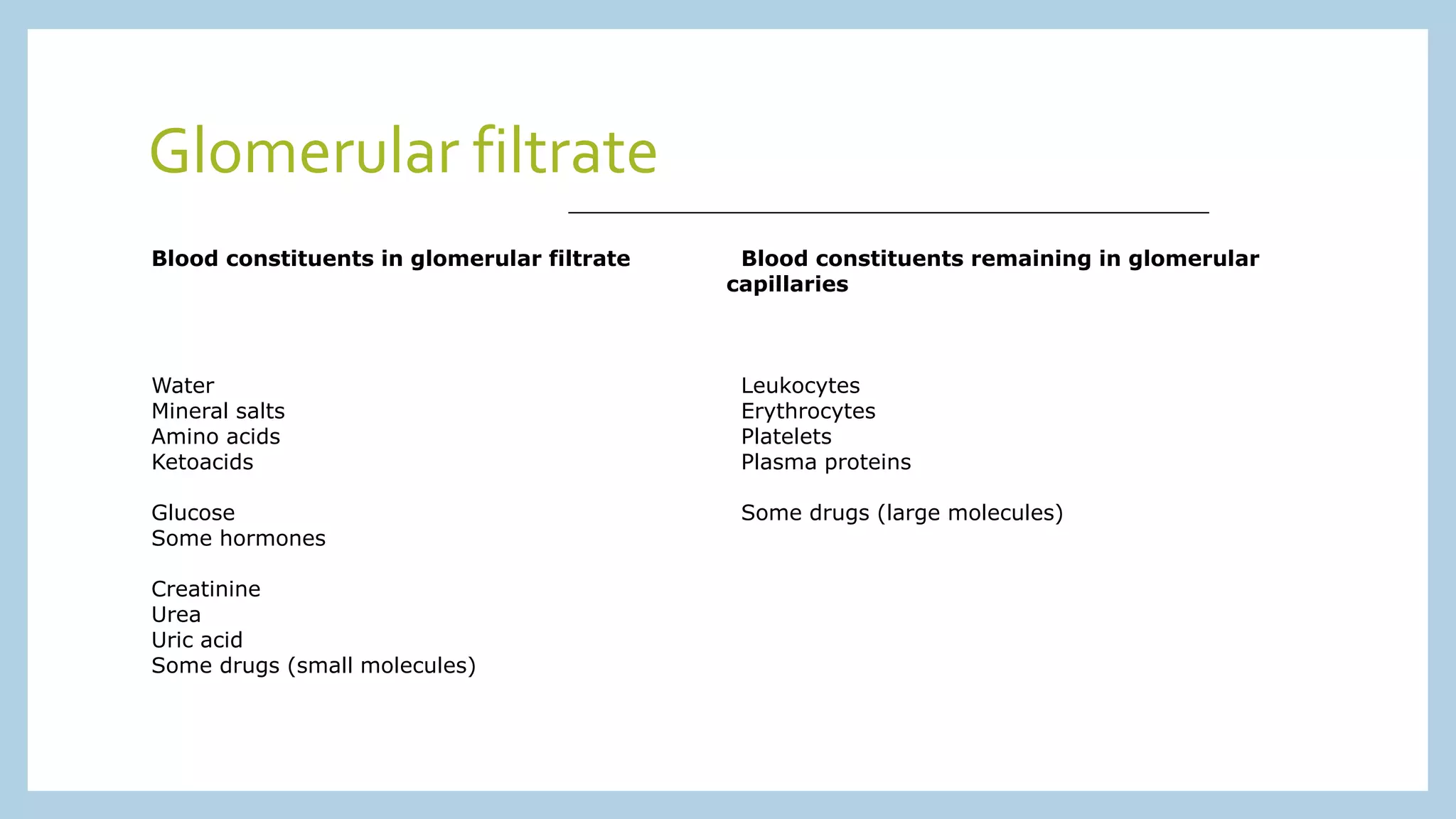
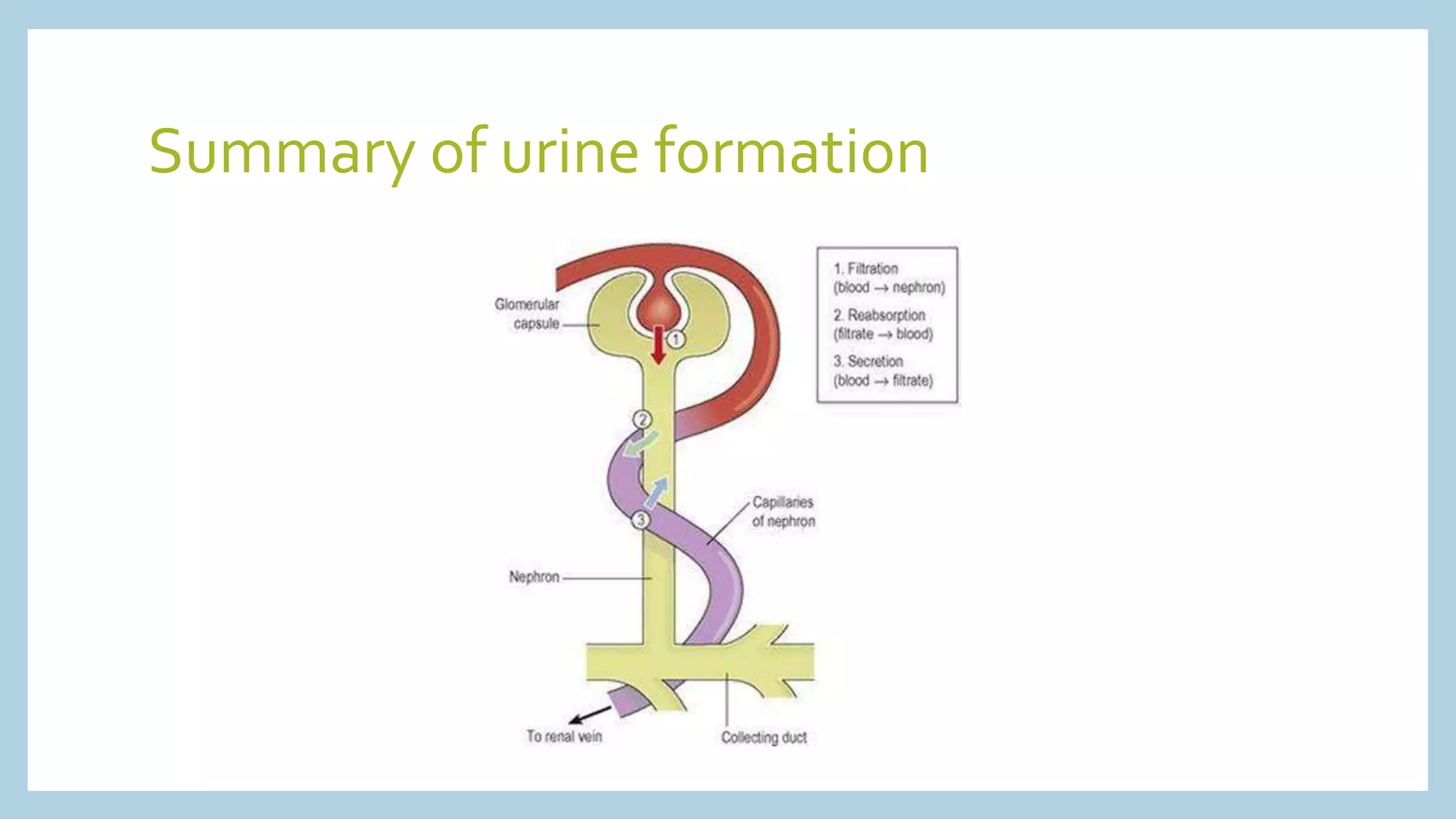
The urinary system consists of the kidneys, ureters, bladder, and urethra. The kidneys filter waste from the blood to form urine. Most of the filtered water and nutrients are reabsorbed, while waste products like urea remain. Hormones like ADH and aldosterone regulate water and electrolyte reabsorption. The urine is stored in the bladder and expelled through the urethra, removing waste from the body.