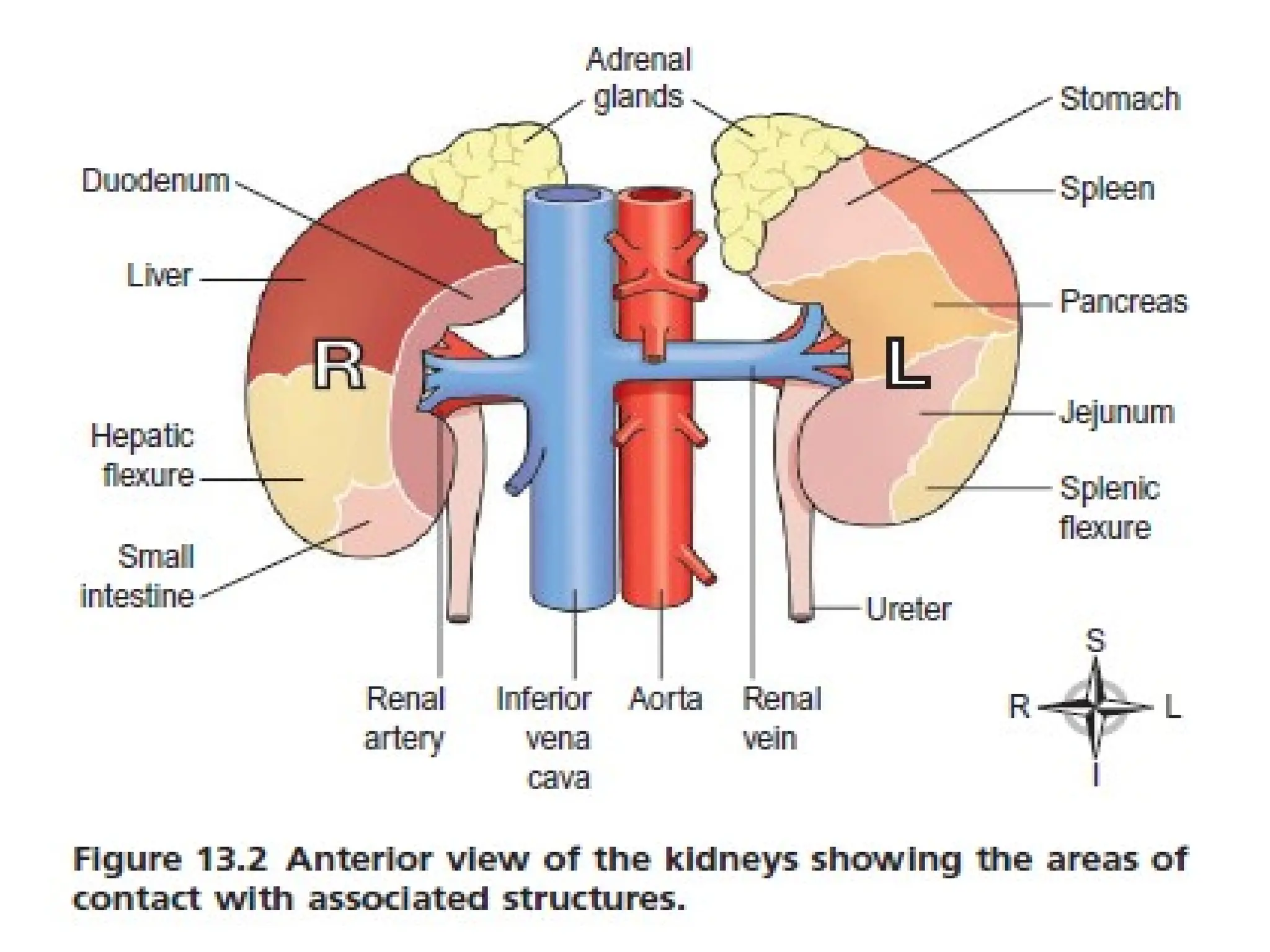
The urinary system consists of the kidneys, ureters, bladder, and urethra, responsible for urine formation and excretion, and maintaining body homeostasis. The kidneys filter blood to produce urine, which involves processes such as filtration, selective reabsorption, and secretion, while also playing crucial roles in regulating blood pressure and blood cell production. Urine is composed of metabolic waste and is stored in the bladder until excretion.