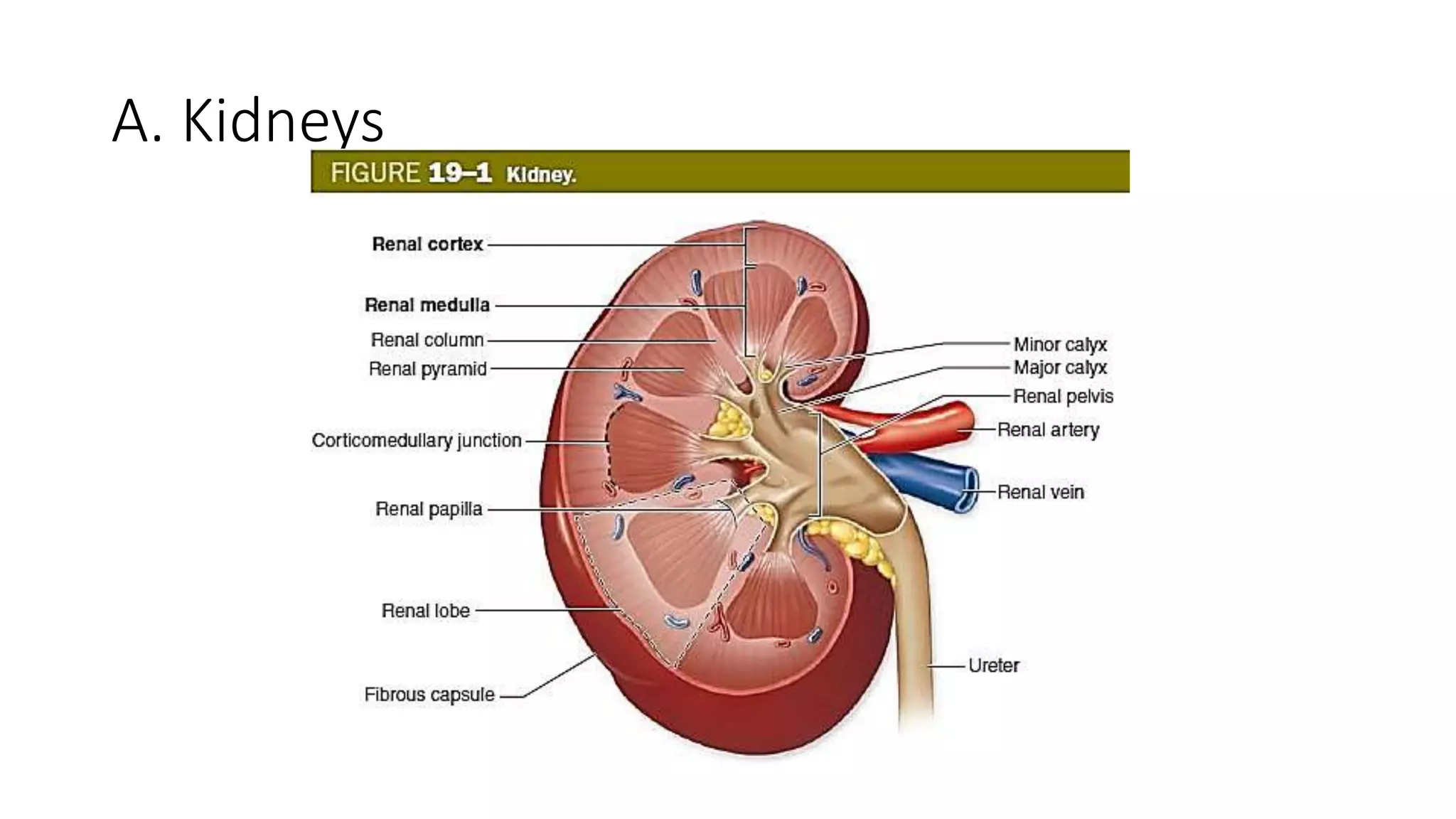
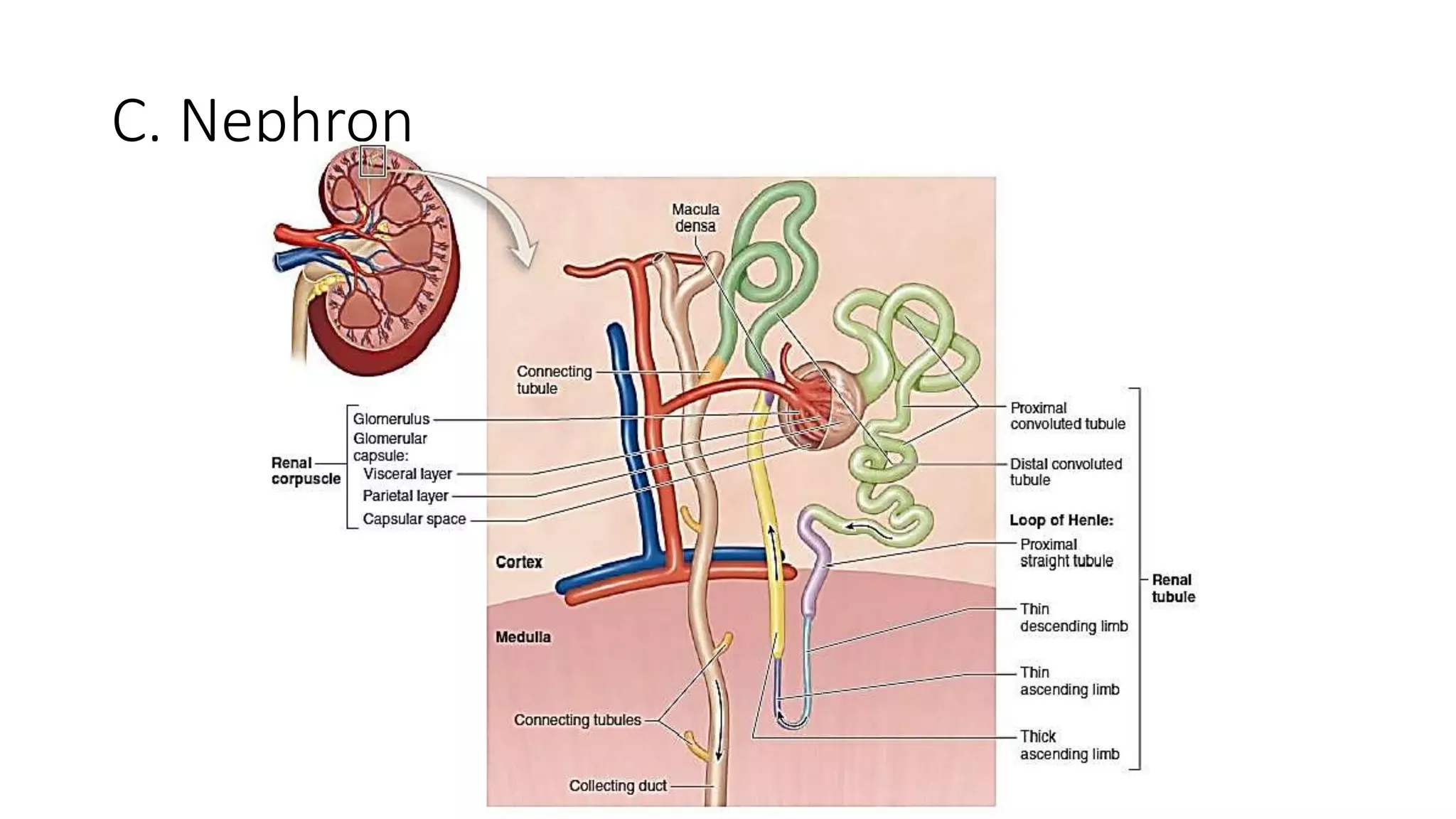
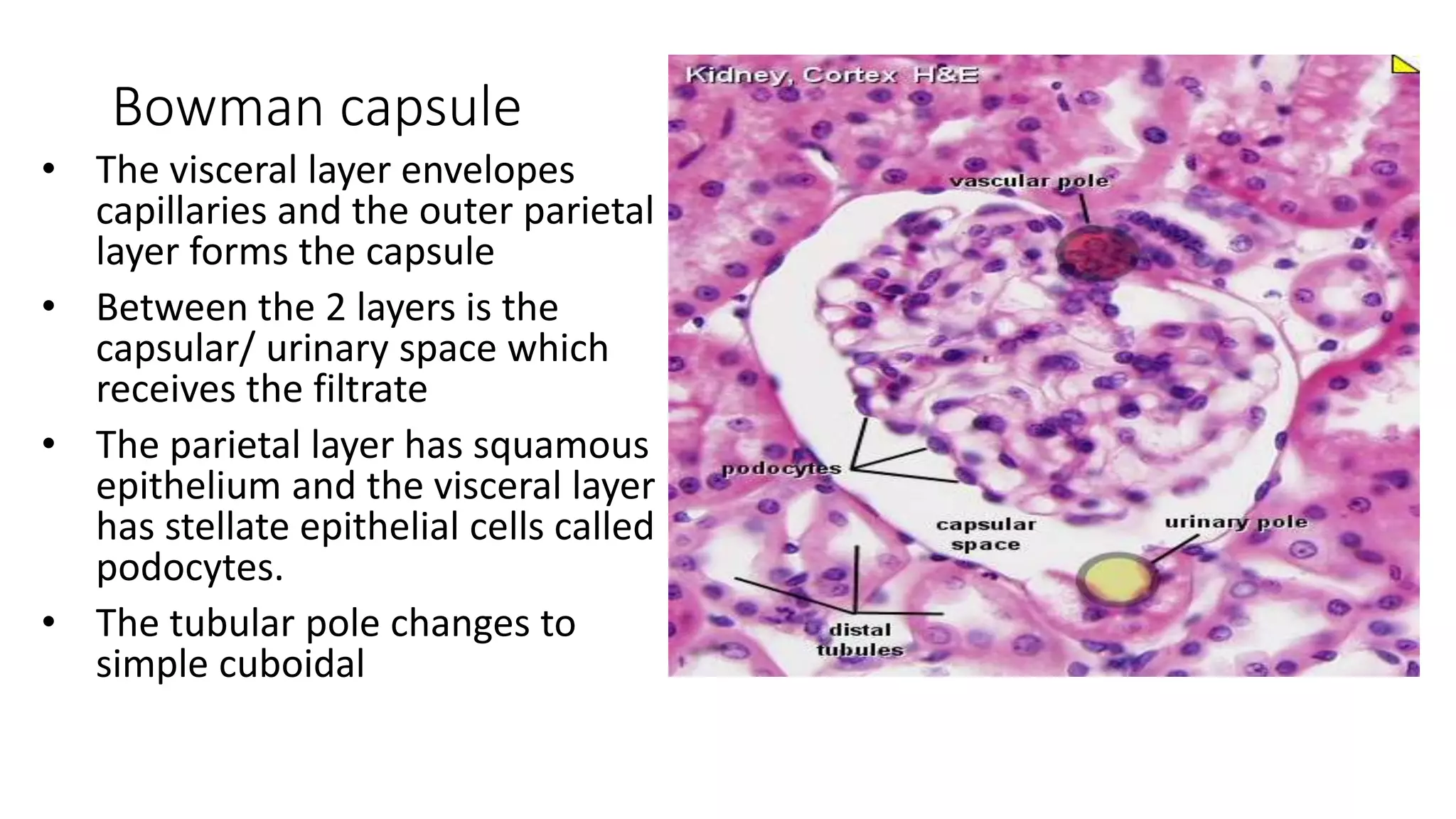
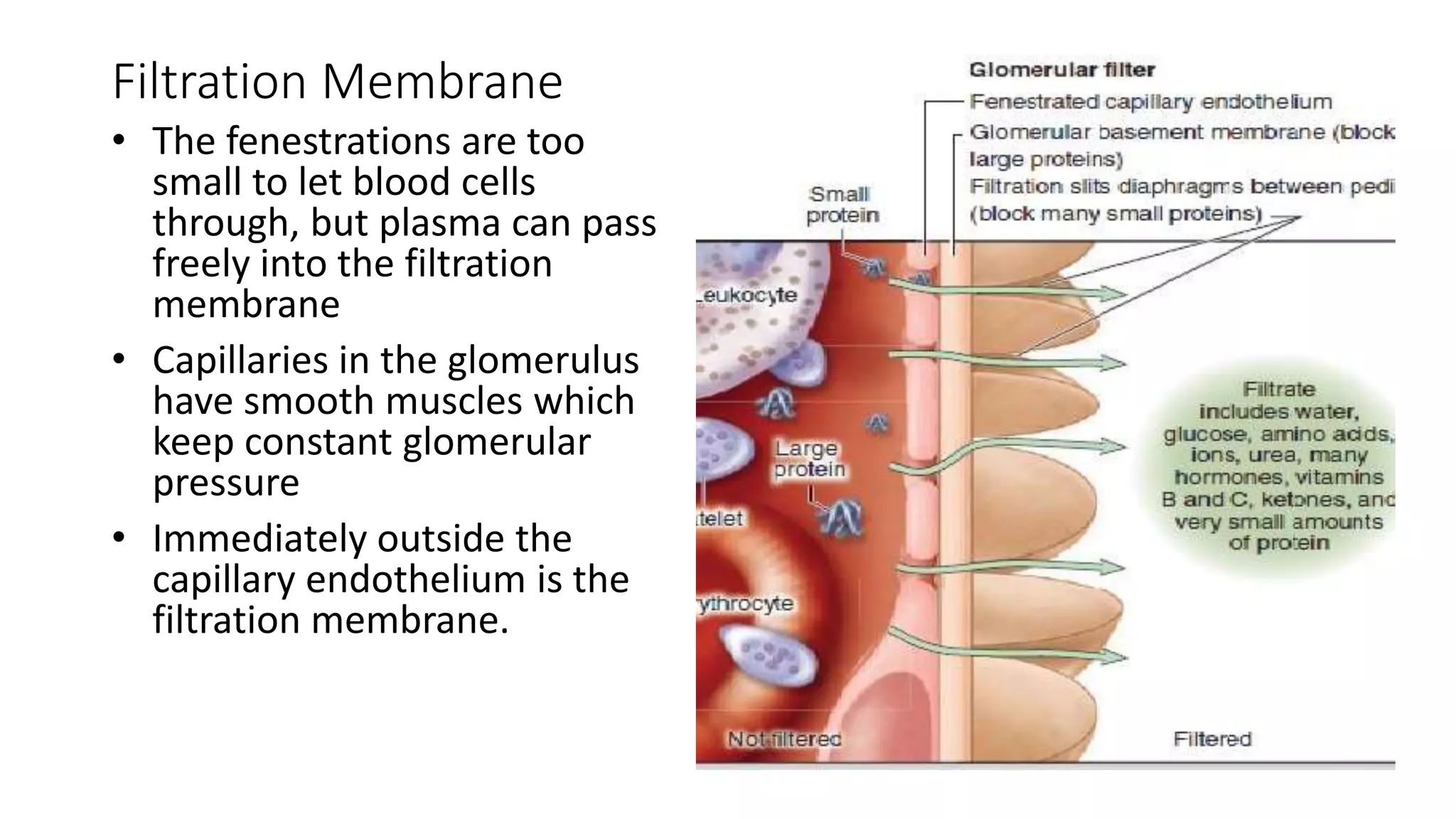
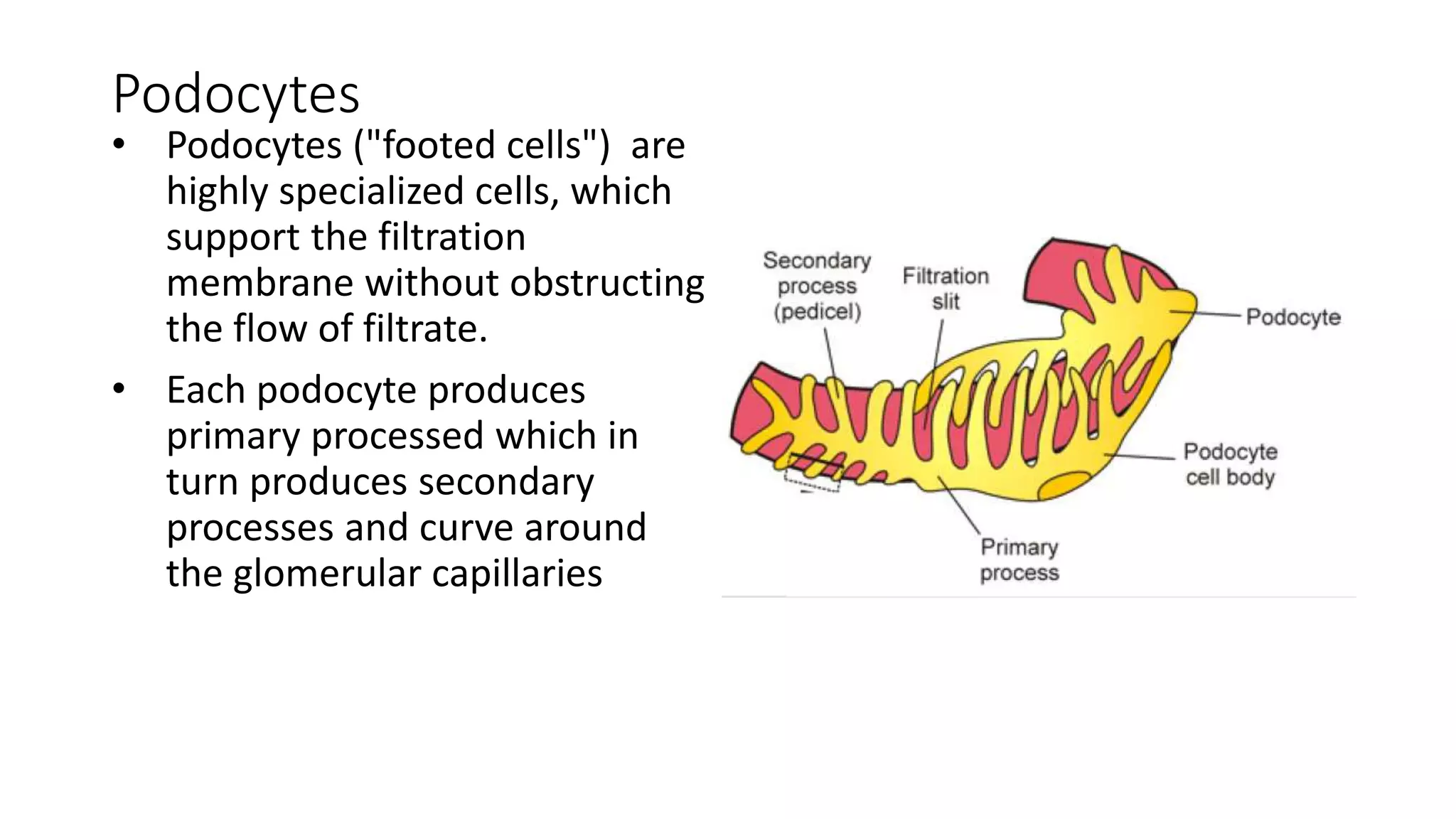
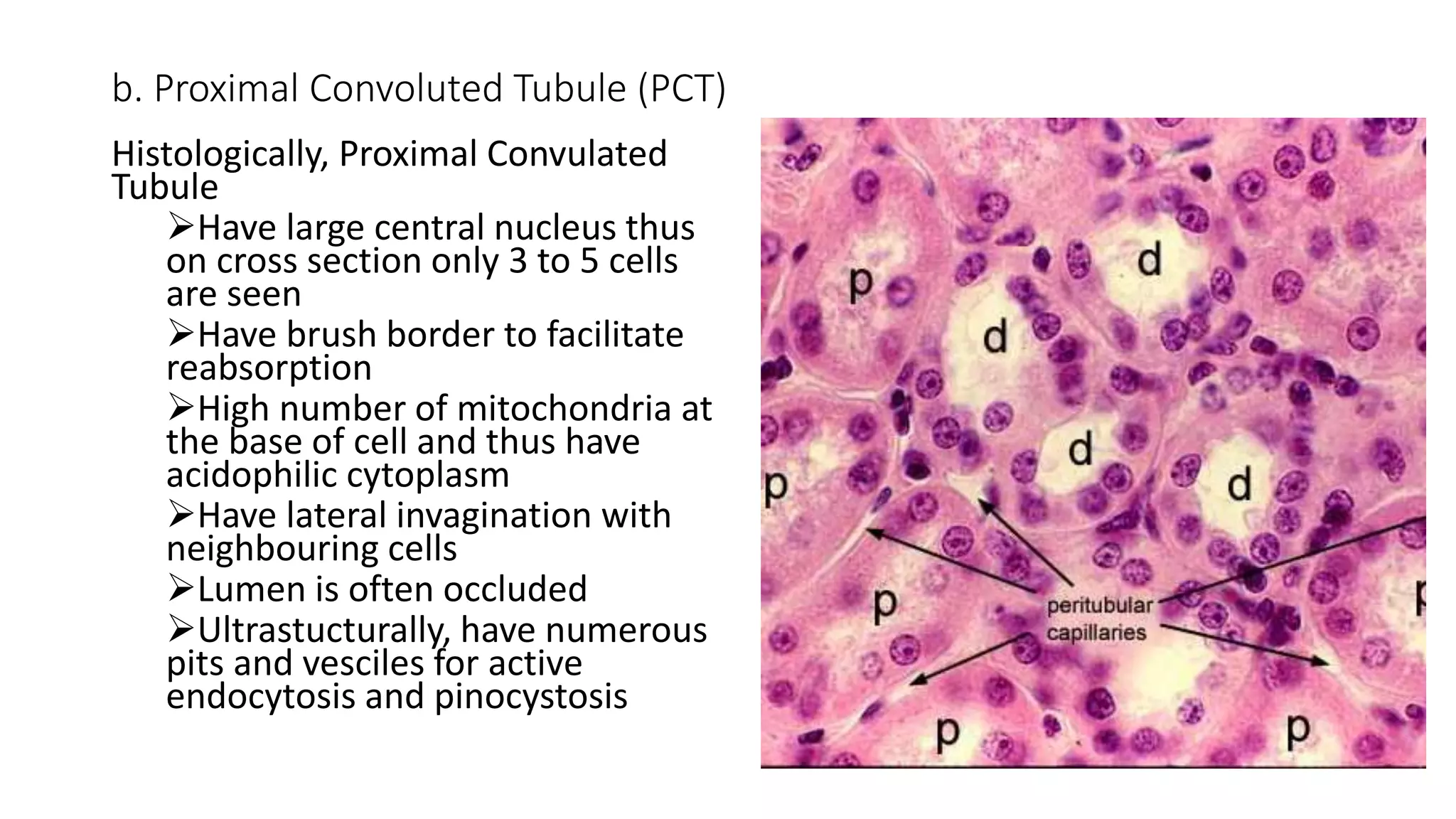
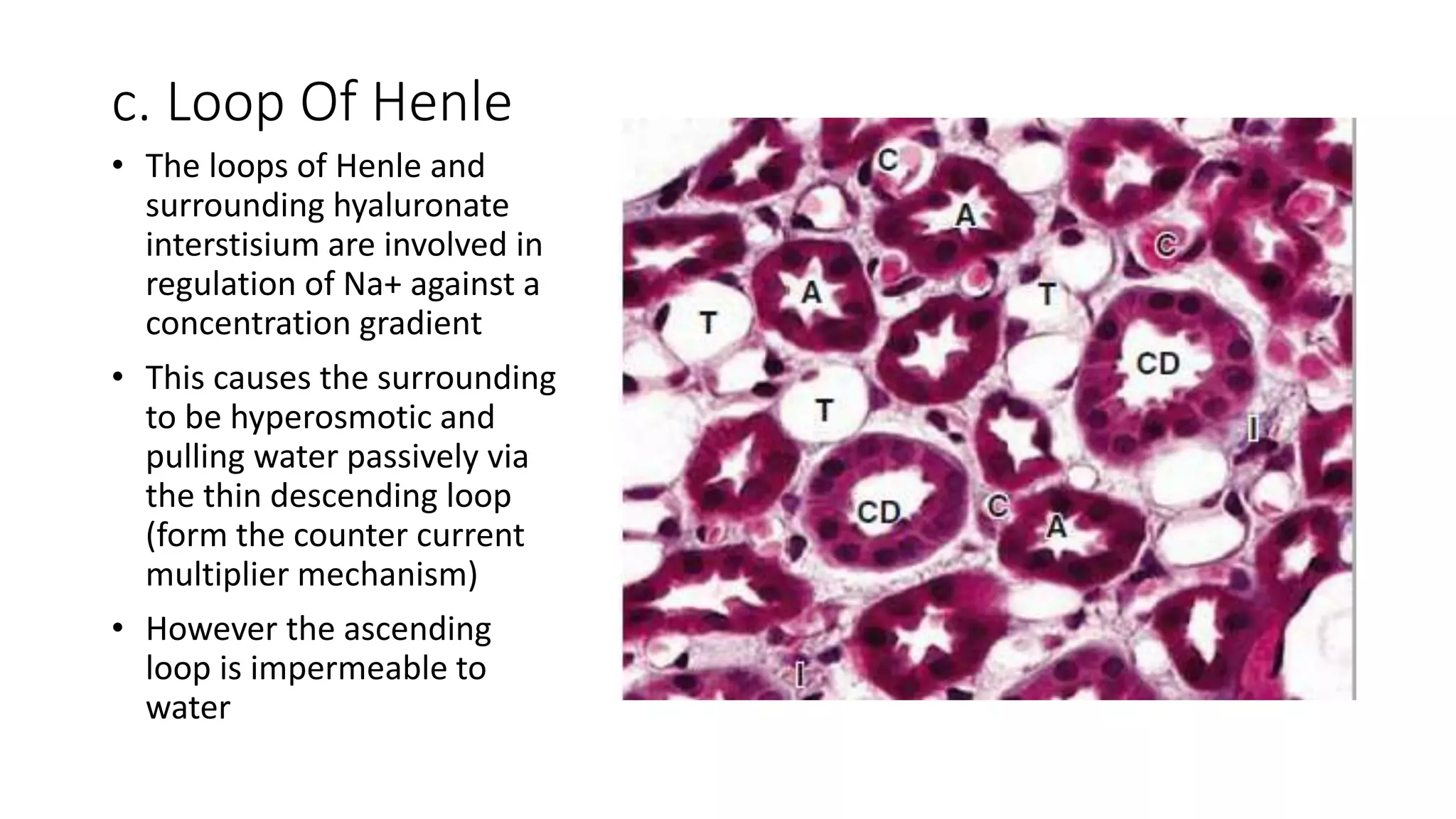
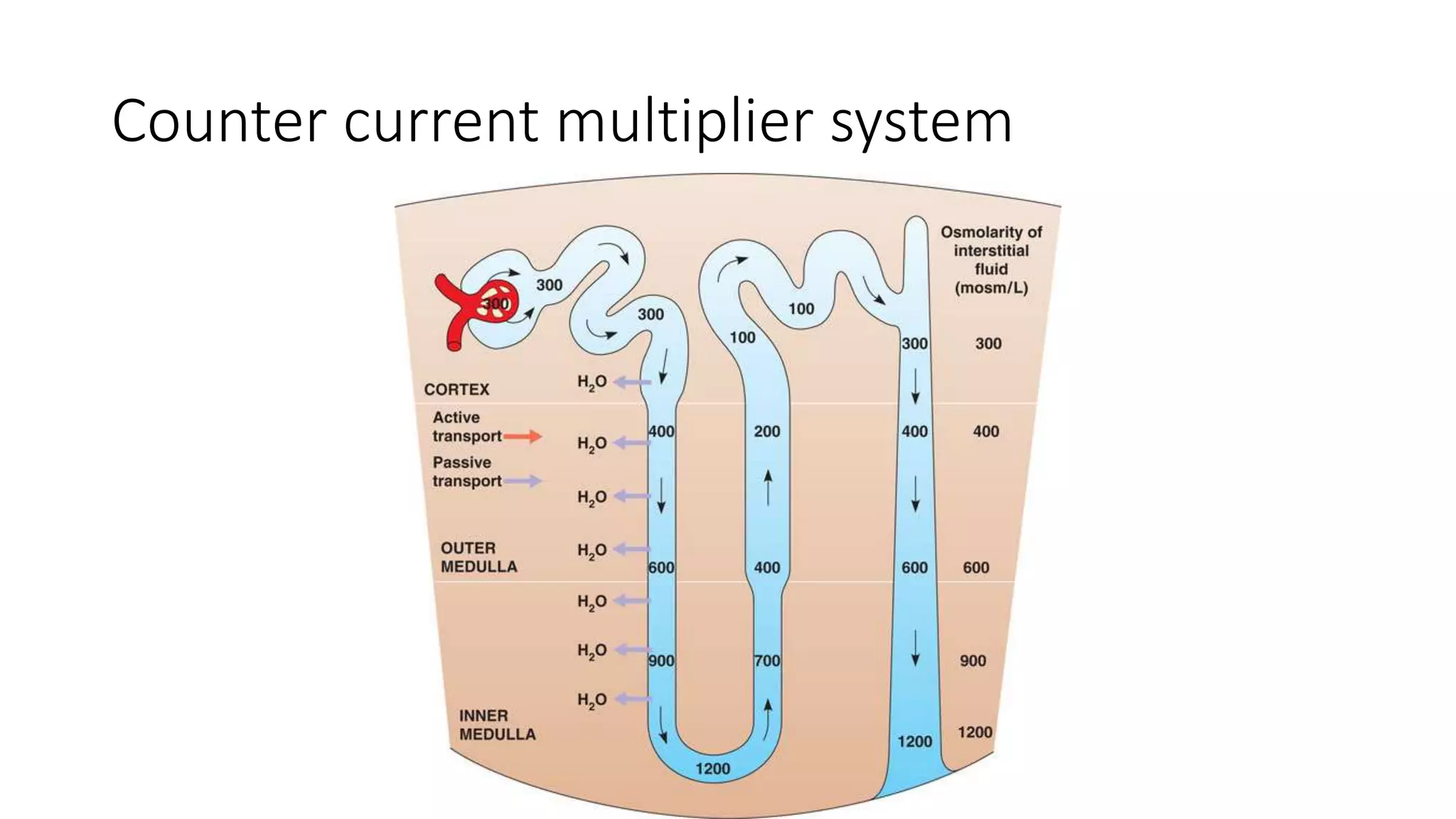
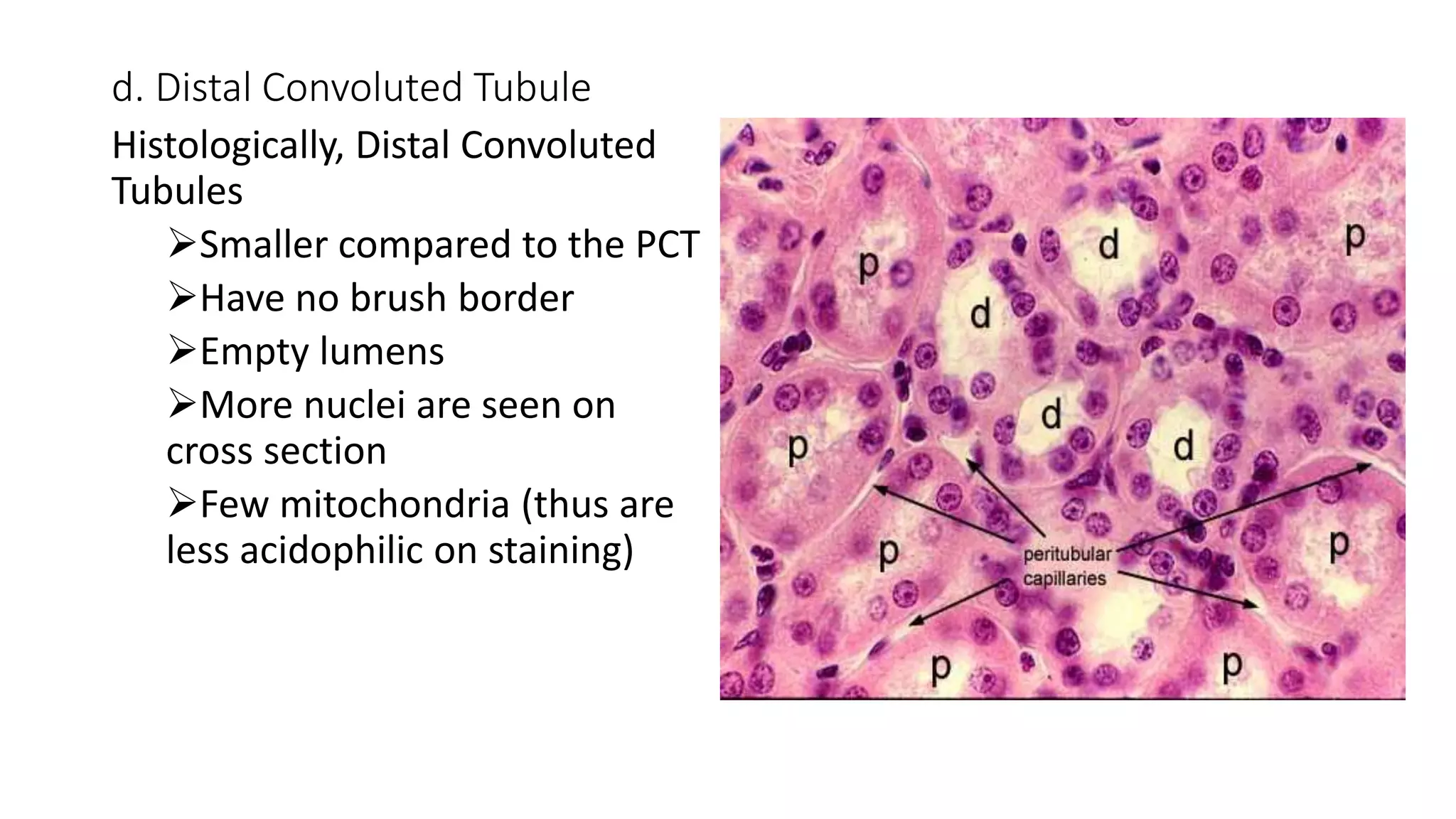
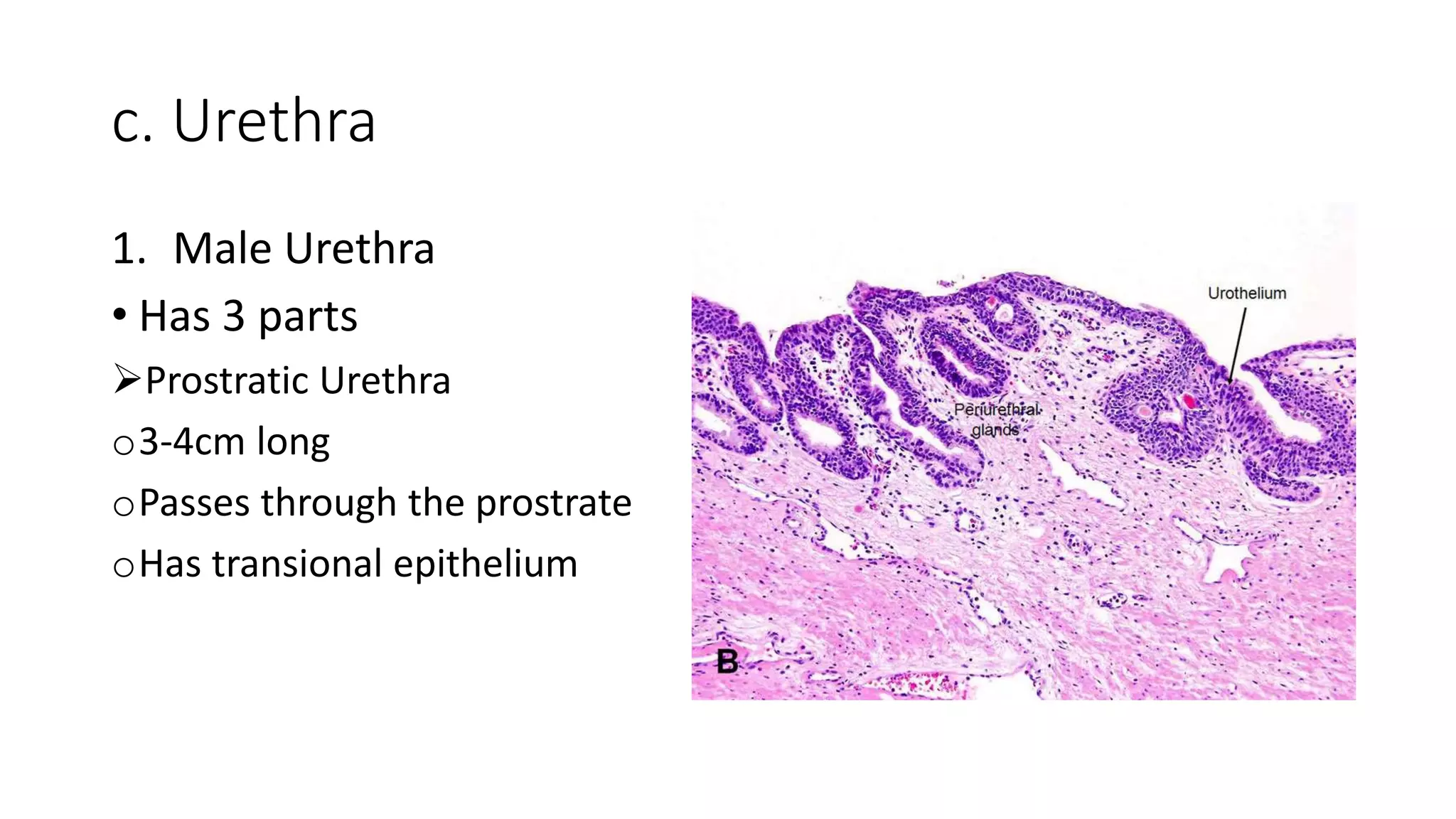
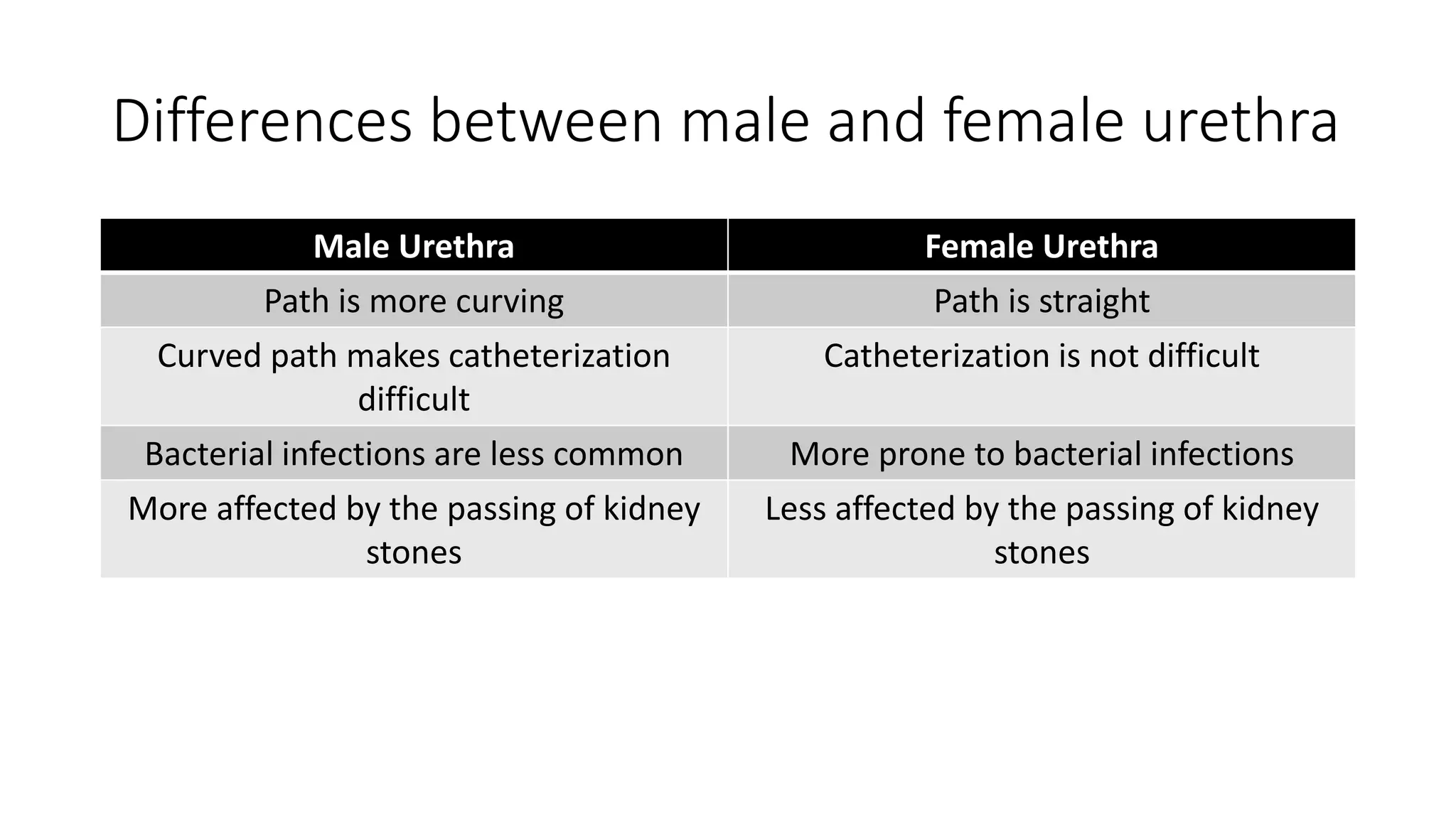
This document provides an overview of the histology of the urinary system. It describes the key components and functions of the kidneys, nephrons, ureters, bladder, and urethra. The kidneys filter blood to form urine and regulate fluid and electrolyte balance. The nephron is the functional unit of the kidney and includes the glomerulus, Bowman's capsule, proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct. Urine passes from the kidneys through the ureters to the bladder for temporary storage before being released through the urethra.