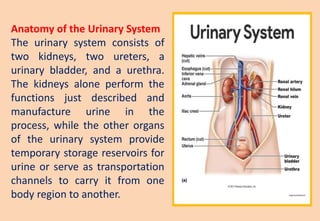
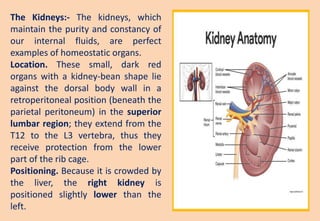
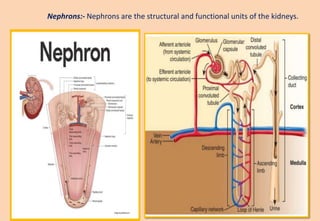
The urinary system consists of two kidneys, two ureters, a urinary bladder, and a urethra. The kidneys filter waste from the blood to produce urine. Each kidney contains over a million nephrons, the functional units that filter blood and form urine. Urine is stored in the bladder and exits the body through the urethra. The kidneys also regulate fluid and electrolyte balance and blood pressure.