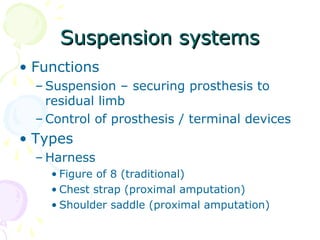
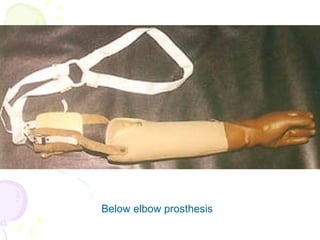
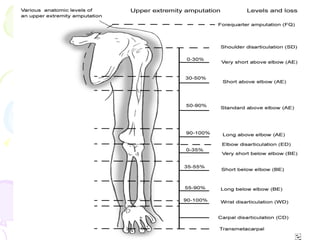
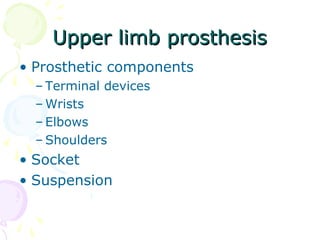
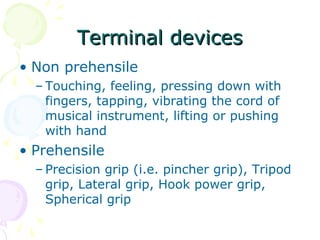
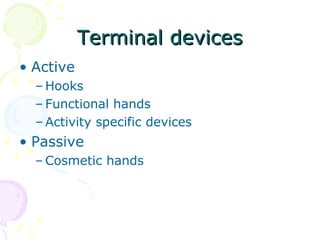
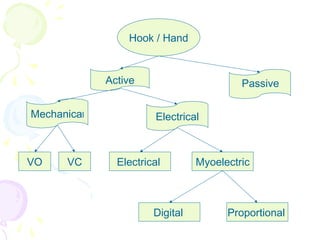
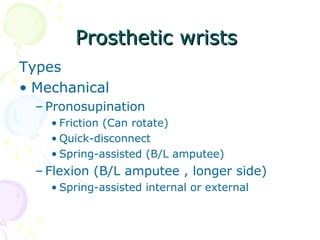
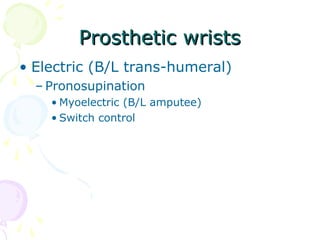
Upper limb prostheses are designed to replace missing limbs and restore function. A successful prosthesis is comfortable, easy to use, lightweight, durable, cosmetically pleasing, and mechanically sound. Prosthesis type depends on amputation level, expected use, patient factors, and resources. Terminal devices can be passive hooks/hands or myoelectric hands. Wrists, elbows, and shoulders provide anatomical movement. Suspension systems secure the prosthesis comfortably. Control mechanisms may be body-powered cables or electric switches/signals. Prosthesis components and design vary according to the amputation level and length of residual limb.









![Various socketsVarious sockets
• Wrist disarticulation socket
• long Below elbow socket
• Short below elbow socket
• Very short below elbow socket
[ Split sockets]
Muenster sockets](https://image.slidesharecdn.com/upperlimbprosthesisdraastha-160415102045/85/Upper-limb-prosthesis-pmr-55-320.jpg)