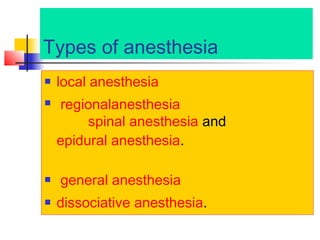
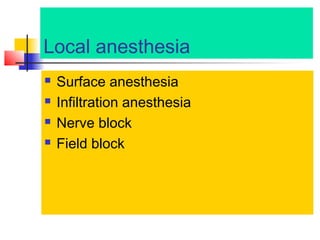
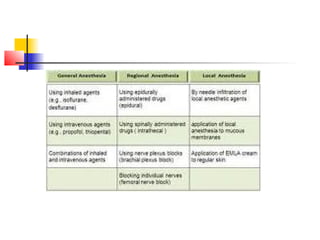
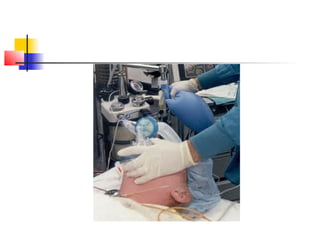
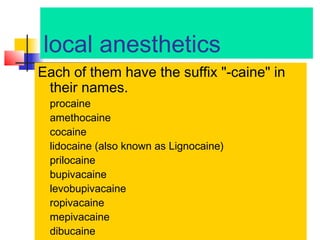
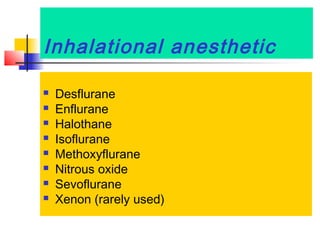
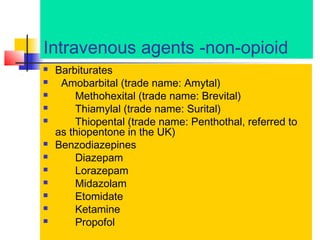
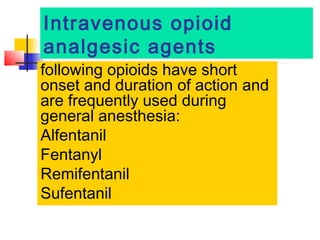
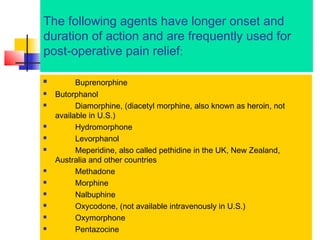
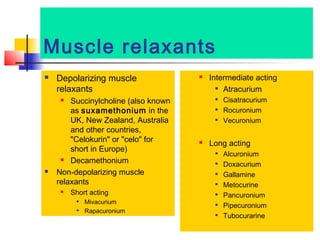
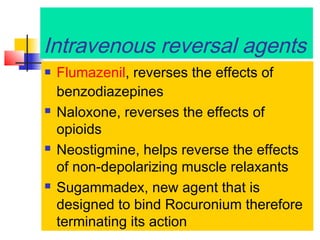
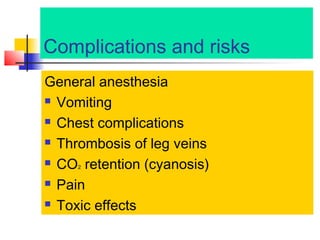
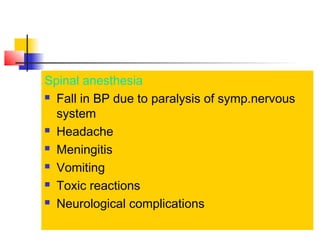
Anesthesia is a medical process where sensation and awareness are temporarily reduced or lost. There are several types including local, regional, spinal/epidural, general, and dissociative anesthesia. Local anesthesia blocks sensation in a specific area while general anesthesia induces a state of unconsciousness. Common agents for general anesthesia include inhalational gases, intravenous medications like propofol and opioids, and muscle relaxants. Proper administration and monitoring during anesthesia aims to balance pain relief with safety.