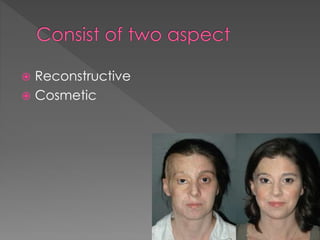
The document discusses physiotherapy management for plastic surgery. It begins by defining plastic surgery as procedures that mould or sculpt tissues to achieve reconstruction or cosmetic effects. It then distinguishes between reconstructive surgery, which improves function or appearance of abnormal structures, and cosmetic surgery, which is optional and performed on normal structures to improve appearance. The document provides examples of different types of reconstructive and cosmetic procedures and outlines factors for physiotherapists to consider in pre-operative assessment and rehabilitation protocols, including surgical details, immobilization needs, exercise prescription, patient education and goals.


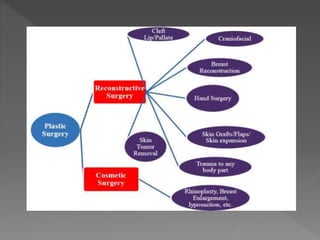

![ Abdominoplasty ("tummy tuck"): reshaping and firming of
the abdomen
Blepharoplasty ("eyelid surgery"): reshaping of the eyelids or the
application of permanent eyeliner, including Asian blepharoplasty
Mammoplasty: Breast augmentations ("breast implant" )
Labiaplasty: surgical reduction and reshaping of the labia
Lip enhancement: surgical improvement of lips' fullness through
enlargement
Rhinoplasty ("nose job"): reshaping of the nose
Otoplasty ("ear surgery"/"ear pinning"): reshaping of the ear
Cheek augmentation ("cheek implant"): implants to the cheek
Orthognathic Surgery: manipulation of the facial bones through
controlled fracturing
Fillers injections: collagen, fat, and other tissue filler injections, such
as hyaluronic acid
Brachioplasty ("Arm lift"): reducing excess skin and fat between the
underarm and the elbow[23]
Laser Skin Rejuvenation or Resurfacing: The lessening of depth in
pores of the face
Liposuction ("suction lipectomy"): removal of fat deposits by
traditional suction technique or ultrasonic energy to aid fat removal
Keloid removal - The keloid forms when the body fails to stop
producing new tissue during healing.](https://image.slidesharecdn.com/ptmanagmentofplasticsurgery12-140911050857-phpapp02/85/PHYSIOTHERAPY-MANAGEMENT-FOR-PLASTIC-SURGERY-11-320.jpg)