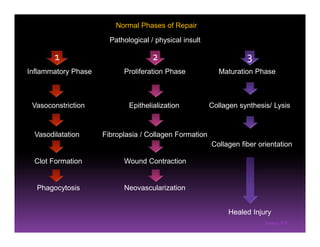
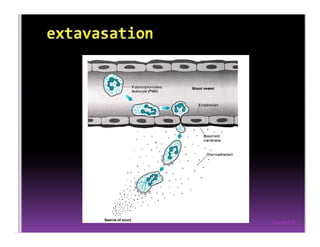
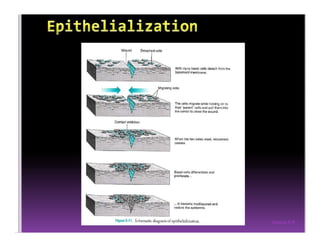
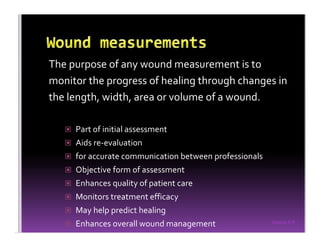
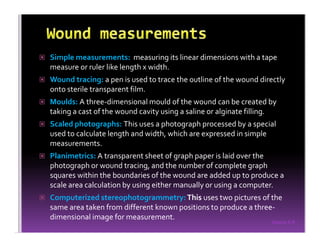
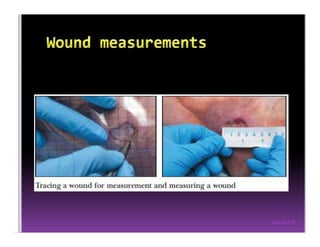
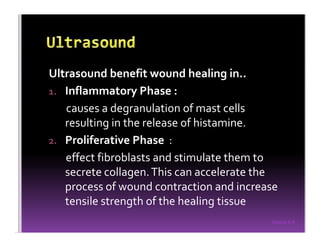
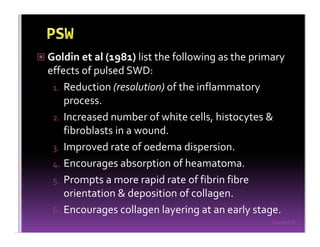
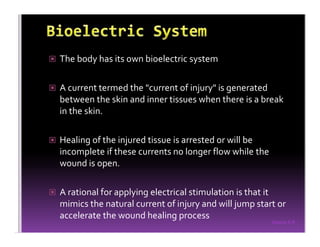
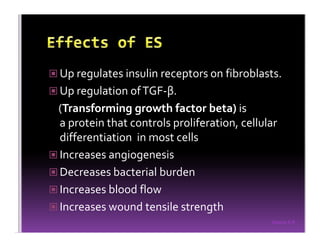
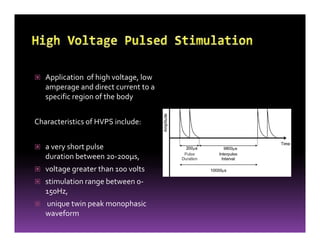
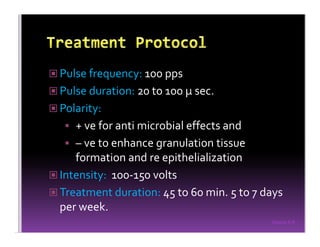
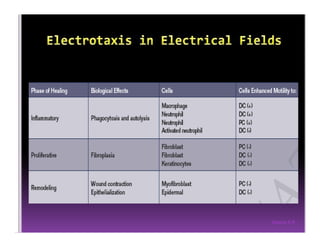
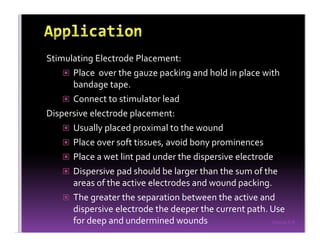
The document discusses wound healing and various modalities used to promote wound healing such as ultrasound, laser, ultraviolet light, and pulsed shortwave diathermy. It covers the normal phases of wound healing including inflammatory, proliferation and maturation phases. Factors that can inhibit wound healing and importance of wound measurement are summarized. Electrical stimulation modalities like high voltage pulsed current and low voltage pulsed current are described along with their proposed mechanisms of action in accelerating wound healing. Placement and treatment procedures for electrical stimulation are also outlined.