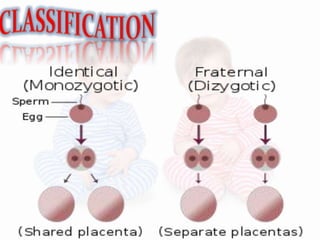
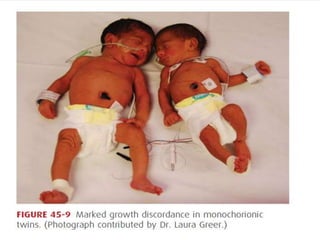
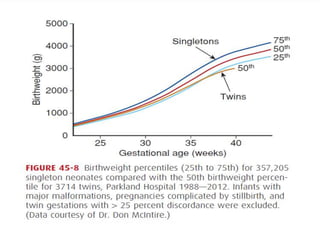
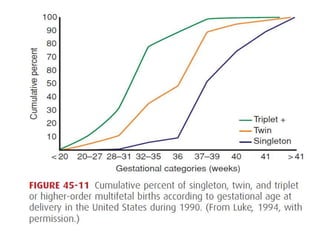
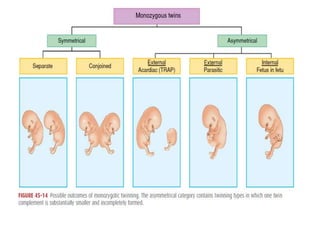
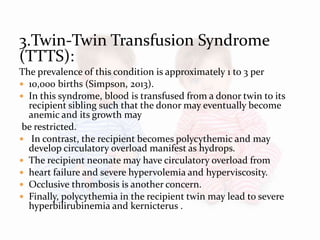
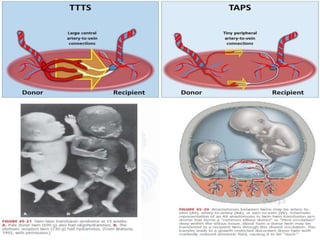
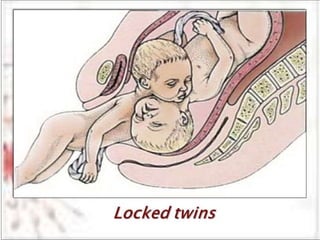
The document discusses various risks and complications associated with multifetal pregnancies, including higher rates of spontaneous abortion, congenital malformations, low birth weight, hypertensive disorders, and preterm births. It highlights that complications are more pronounced in twins, particularly monochorionic twins, leading to different risks in outcomes such as cognitive delays and twin-twin transfusion syndrome. The findings underscore the need for careful management and monitoring of multifetal gestations to minimize adverse outcomes.