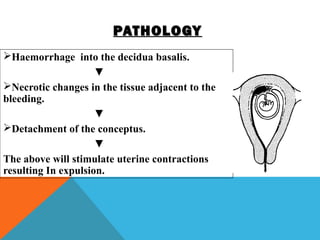
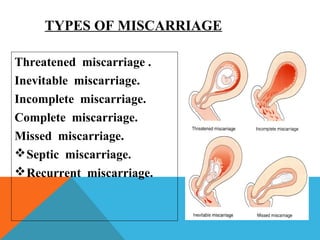
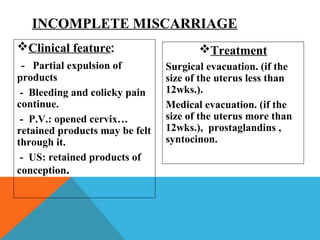
Dr. Tarig Mahmoud discusses various causes and types of early pregnancy bleeding and miscarriage. There are several potential causes of miscarriage, including fetal chromosomal abnormalities, maternal medical conditions, infections, and uterine/cervical issues. The main types of miscarriage are threatened, inevitable, incomplete, complete, and missed. Recurrent miscarriage is defined as three or more consecutive losses. Septic miscarriage can occur if an incomplete miscarriage leads to an ascending infection. Counseling is important to reassure patients and provide psychological support after a miscarriage.