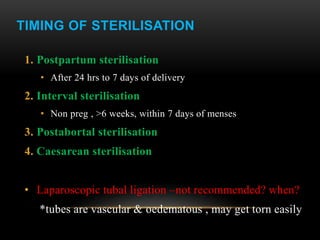
This document discusses female sterilization procedures including timing, guidelines, surgical approaches, counseling requirements, and complications. It describes minilaparotomy, laparoscopic sterilization, and vaginal tubal ligation methods. Timing options include postpartum, interval, or postabortal sterilization. Counseling must cover permanence, risks, and potential for failure or reversal. Surgical risks include infection, bleeding, and injury to nearby organs. Laparoscopy is preferred for interval sterilization due to lower risk of complications compared to minilaparotomy.