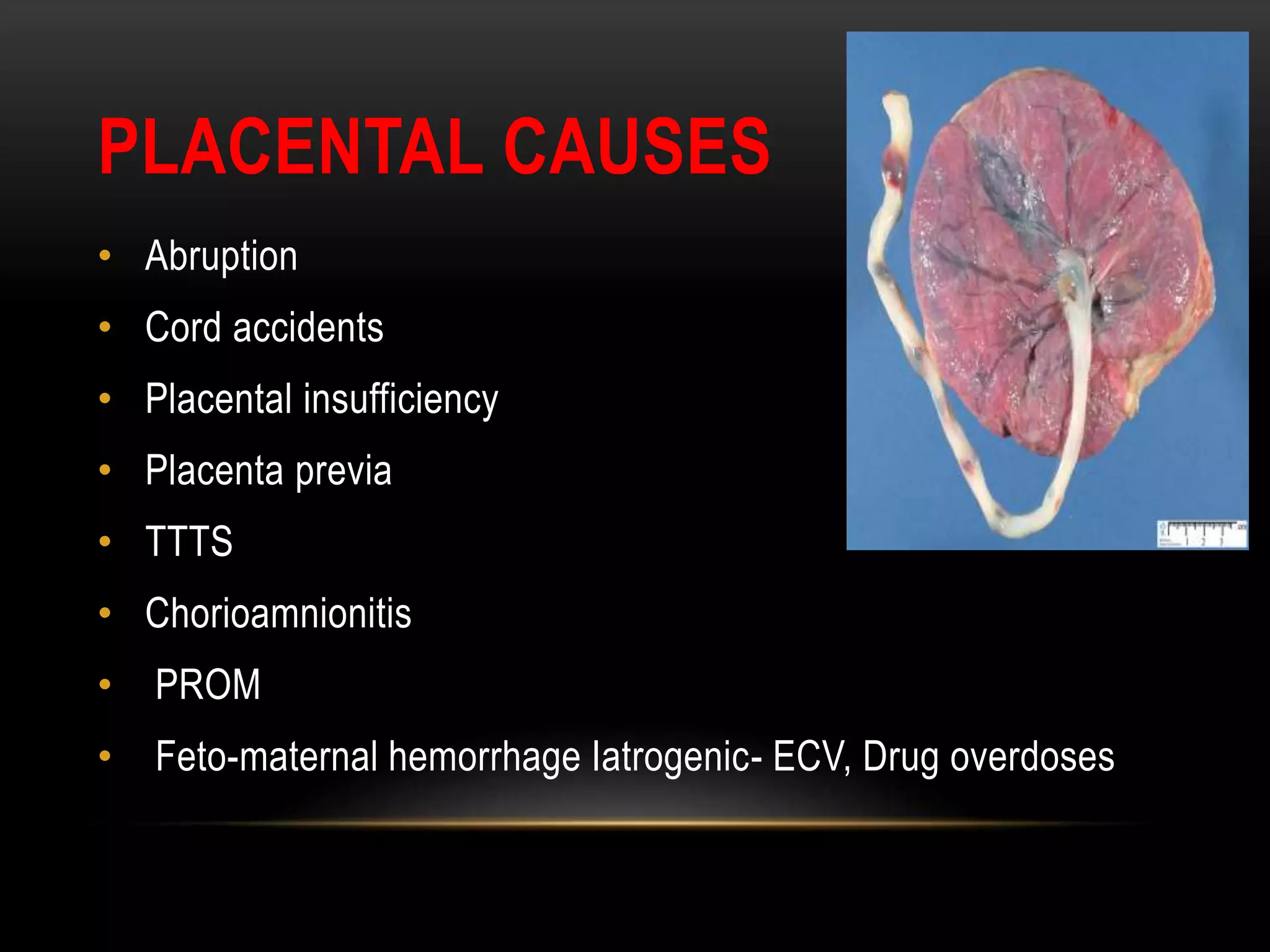
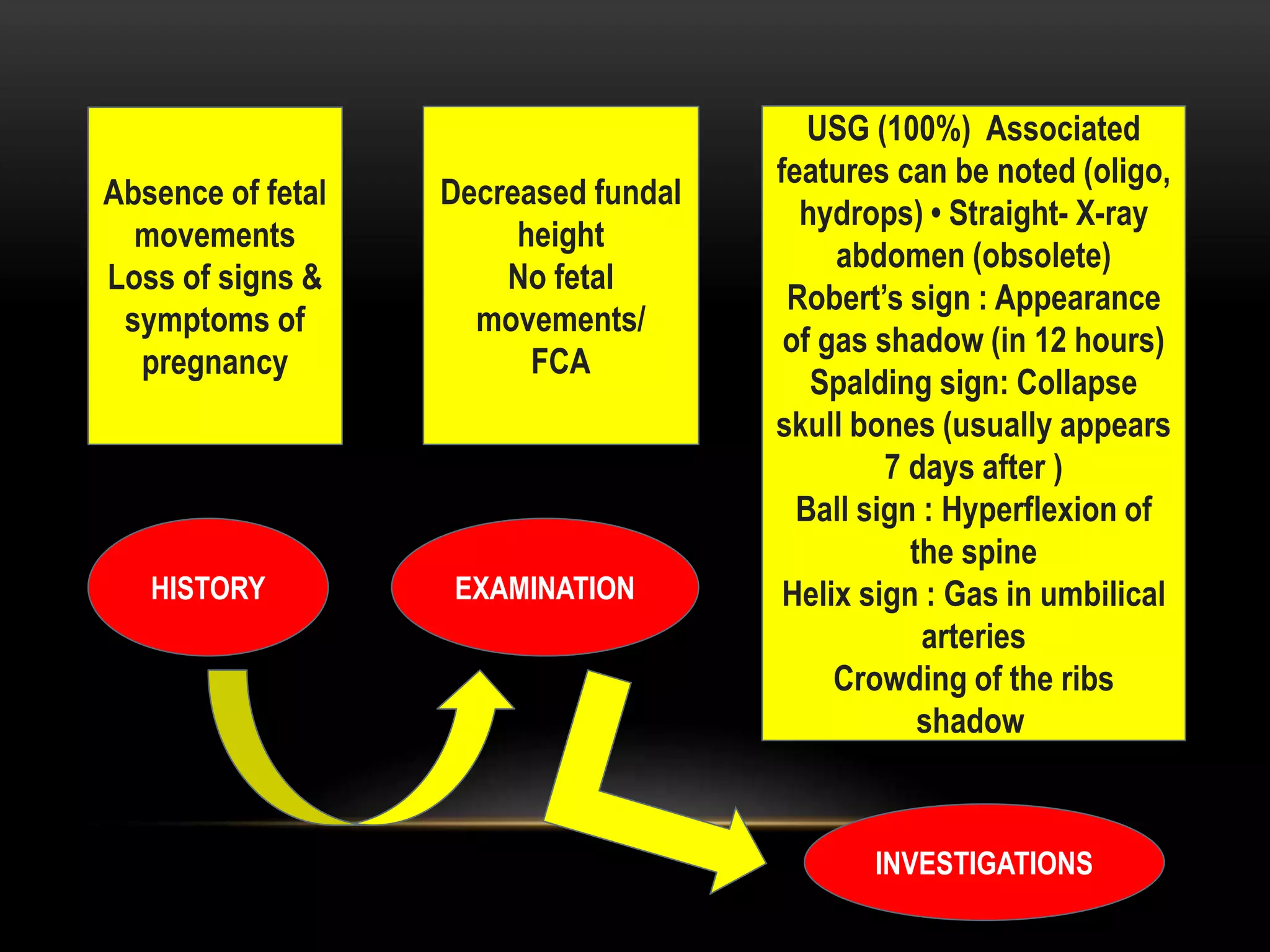
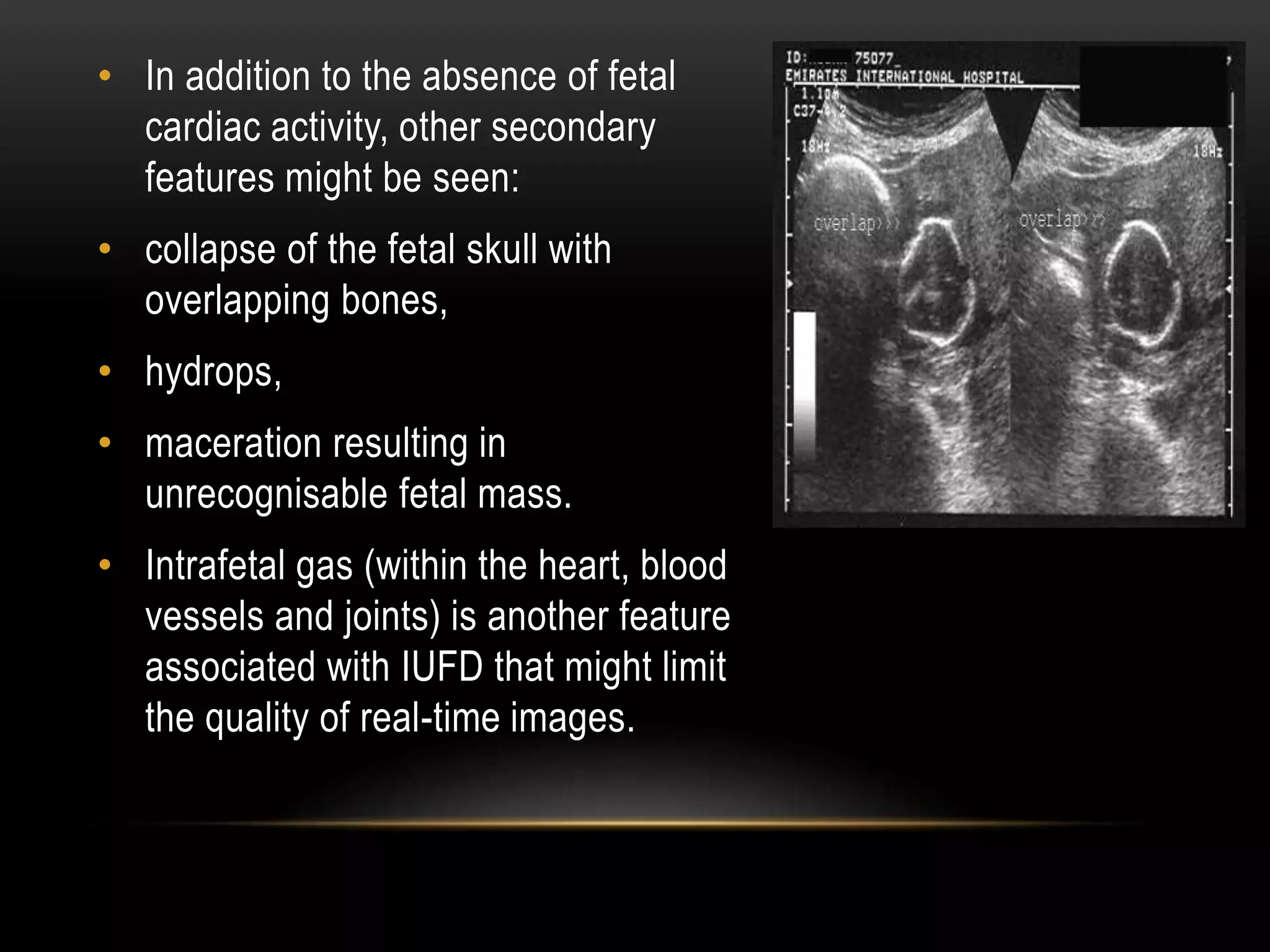
Intrauterine fetal death refers to babies with no signs of life in utero after 24 completed weeks of gestation or weighing over 500g. The document discusses the definition, incidence, impacts, causes, diagnosis, investigations, labour and birth process, complications, lactation, postmortem examination, legal issues, psychological aspects, and follow up considerations for intrauterine fetal death. The overall goal is to provide compassionate care for the health of the mother and support for her and her partner during this difficult time.