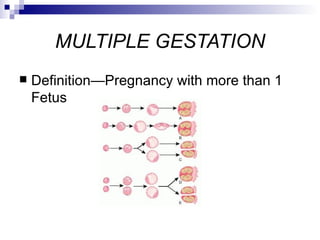
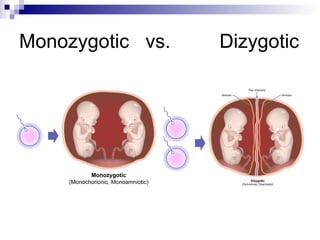
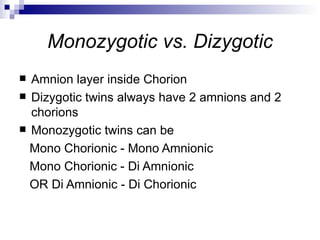
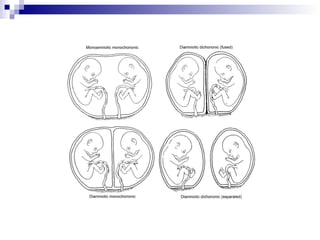
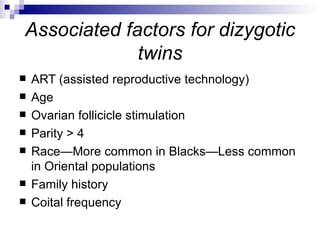
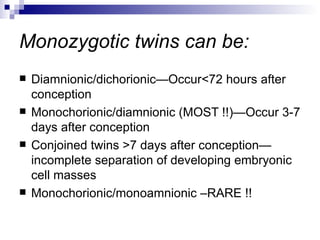
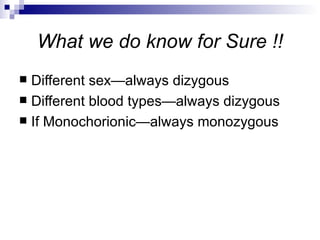
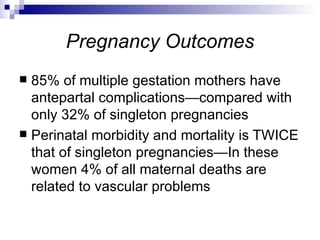
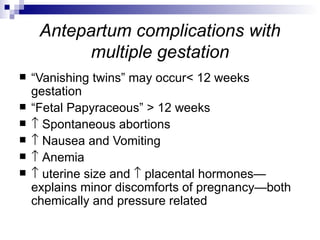
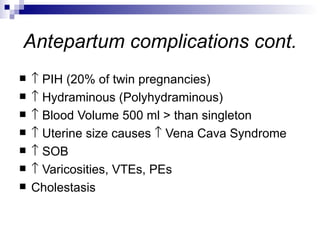
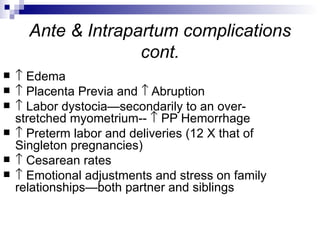
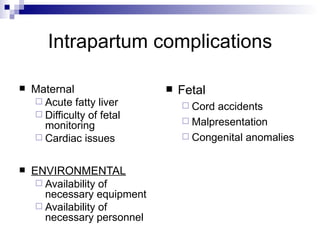
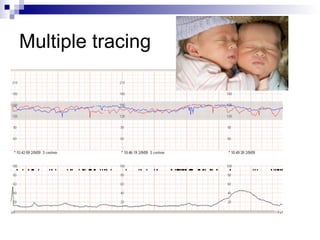
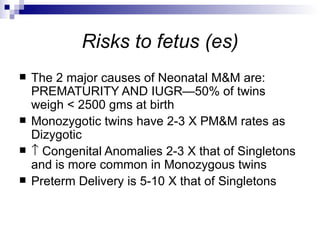
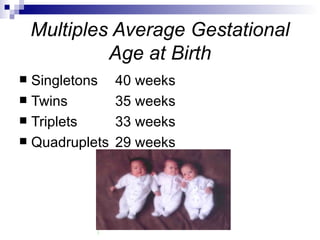
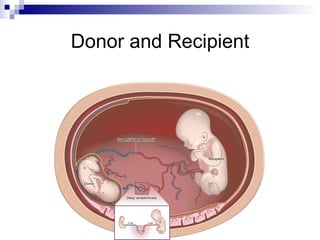
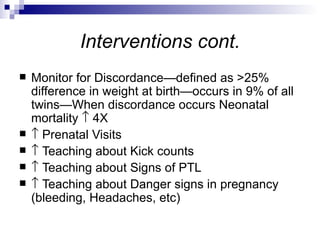
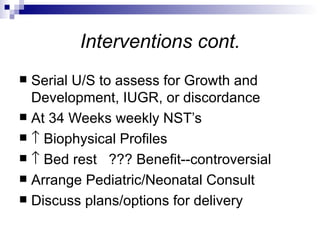
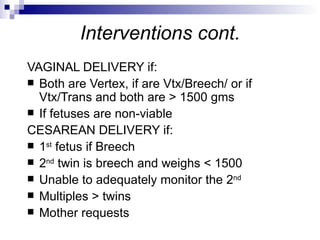
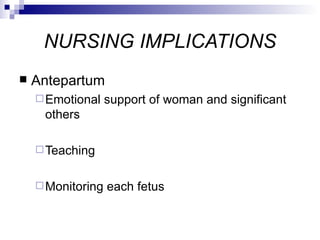
This document discusses multiple gestation pregnancies. It defines multiple gestation as a pregnancy with more than one fetus. The most common type is twins, which can be either monozygotic (identical) or dizygotic (fraternal). Multiple gestation pregnancies have higher risks of complications for both the mother and fetuses, including preterm birth and low birth weight. Close monitoring and interventions are needed to help support a healthy pregnancy outcome.