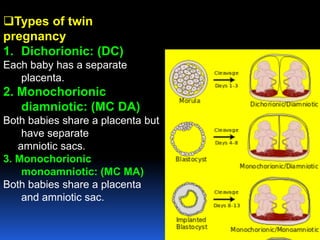
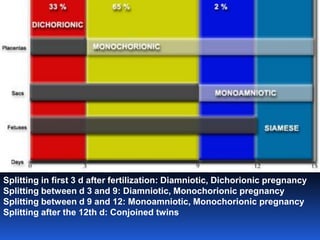
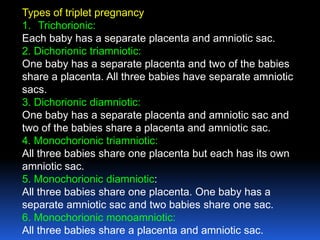
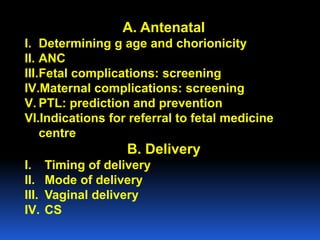
This document provides guidelines for the management of multiple pregnancies. It discusses the types of twin and triplet pregnancies based on placental and membrane characteristics. Key aspects of antenatal care are outlined, including determining gestational age and chorionicity, antenatal visits, screening for fetal and maternal complications, monitoring growth and preventing preterm birth. Indications for referral to a tertiary center are provided. For delivery, optimal gestational ages for different multiple pregnancies are noted as well as considerations for mode of delivery including vaginal versus cesarean section. Intrapartum management for both types of delivery is described.





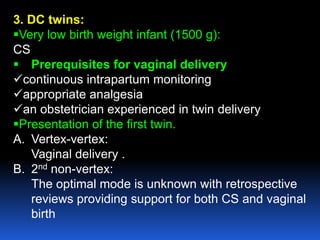
![Second stage:
1. Delivery must be attended by
Obstetric Consultant
Neonatal team
Anaesthetic Registrar
Operating department assistant should also be
immediately available.
2. Both fetal hearts should be electronically
monitored continuously
3. Syntocinon infusion should be made ready for
use after the first twin has delivered, to be used at
the discretion of the consultant
[20 units added to 500ml NS at 30ml/h – i.e.20 milliunits
/min.]](https://image.slidesharecdn.com/multiplepregnancy-140617064211-phpapp02/85/Multiple-pregnancy-Aboubakr-Elnashar-45-320.jpg)
![THIRD STAGE:
{significant risk of PPH}
syntocinon and methrgin to be given according to
protocol following delivery of the second twin.
A syntocinon infusion of 20 units in 500ml NS
immediately after the birth of the second twin, and
given at a rate of 120ml/h
[i.e.80 milliunits/minute] for 2-3 h.](https://image.slidesharecdn.com/multiplepregnancy-140617064211-phpapp02/85/Multiple-pregnancy-Aboubakr-Elnashar-48-320.jpg)