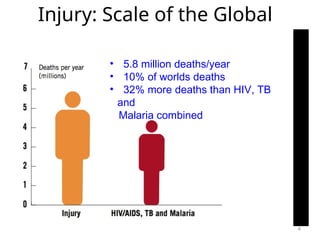
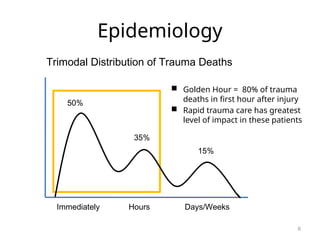
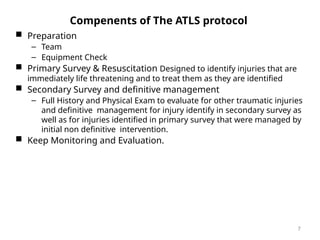
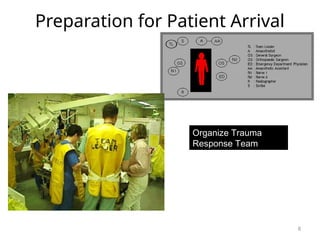
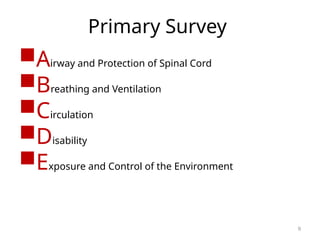
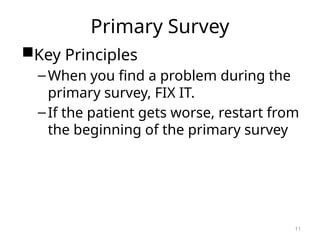
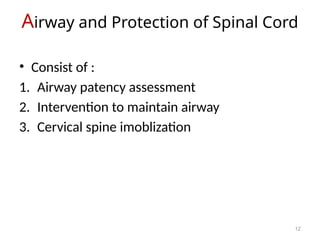
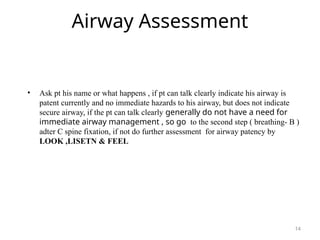
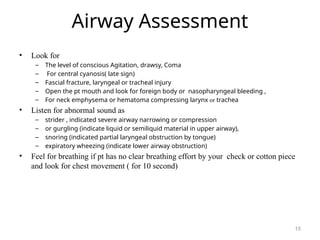
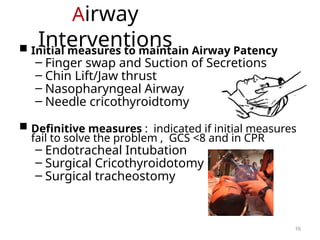
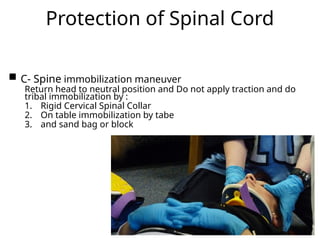
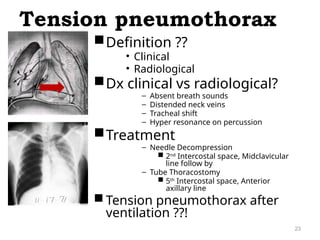
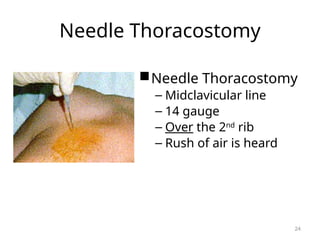
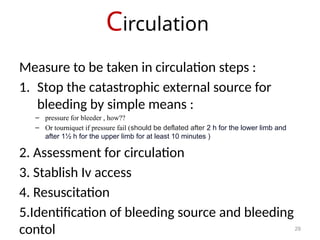
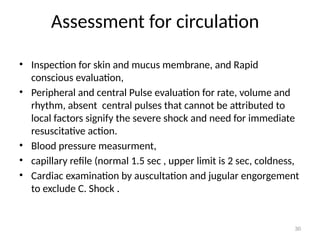
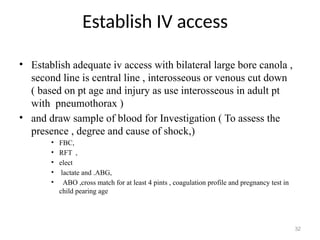
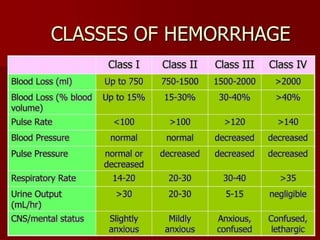
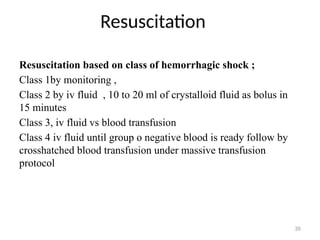
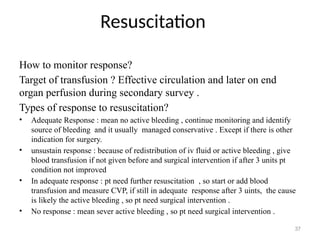
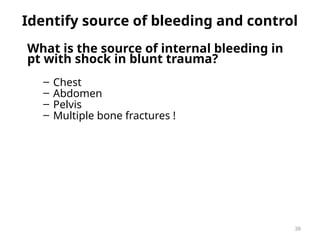
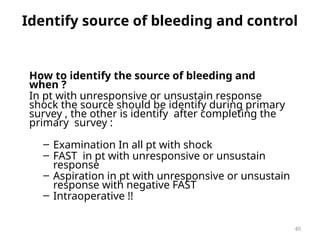
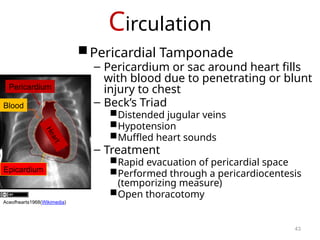
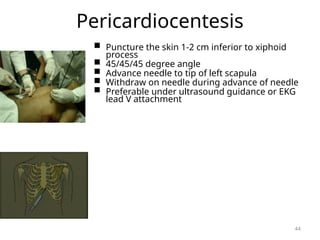
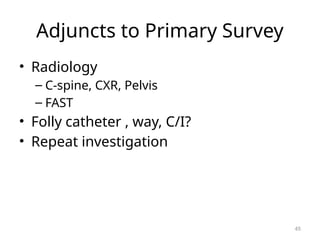
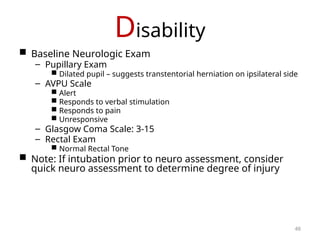
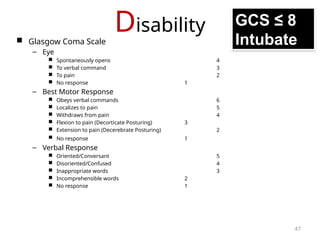
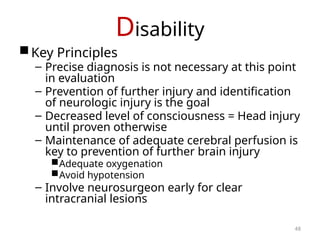
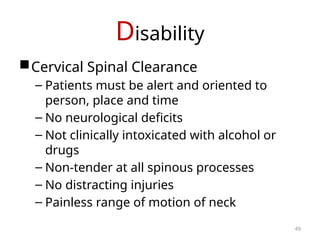
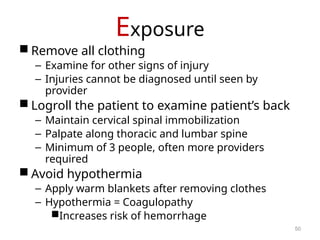
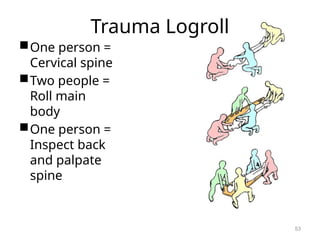
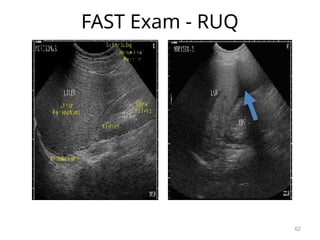
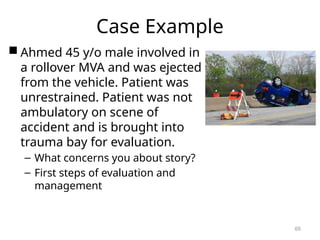
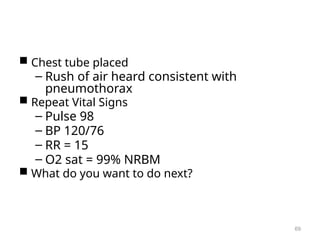
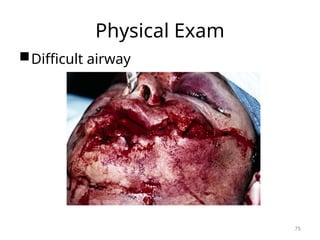
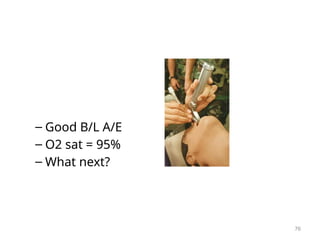
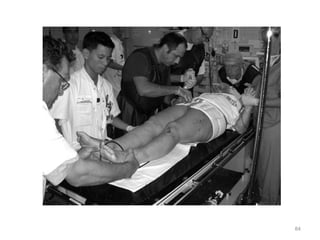
The document outlines the Advanced Trauma Life Support (ATLS) protocol aimed at improving trauma care through a structured approach to identifying and treating life-threatening injuries. It details the components of the protocol, including the primary survey and resuscitation, as well as methods for assessing airway, breathing, circulation, and disability in trauma patients. The importance of rapid response in trauma situations, particularly during the 'golden hour', and the necessity for continuous evaluation and monitoring during patient care are emphasized.