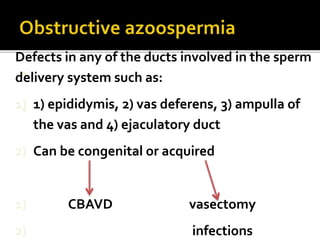
This document summarizes male infertility, including its causes and evaluation/treatment. It discusses spermatogenesis directed by Y chromosome genes and roles of the testes, LH, FSH, and epididymis. Normal sperm counts and definitions of oligospermia and azoospermia are provided. Causes of azoospermia are classified as obstructive or non-obstructive and can be pretesticular, testicular, or post-testicular. Evaluation involves endocrine and genetic testing as well as imaging of the testes and ducts. Treatment depends on the location and cause, such as hormone therapy, surgical repair, or sperm retrieval techniques.