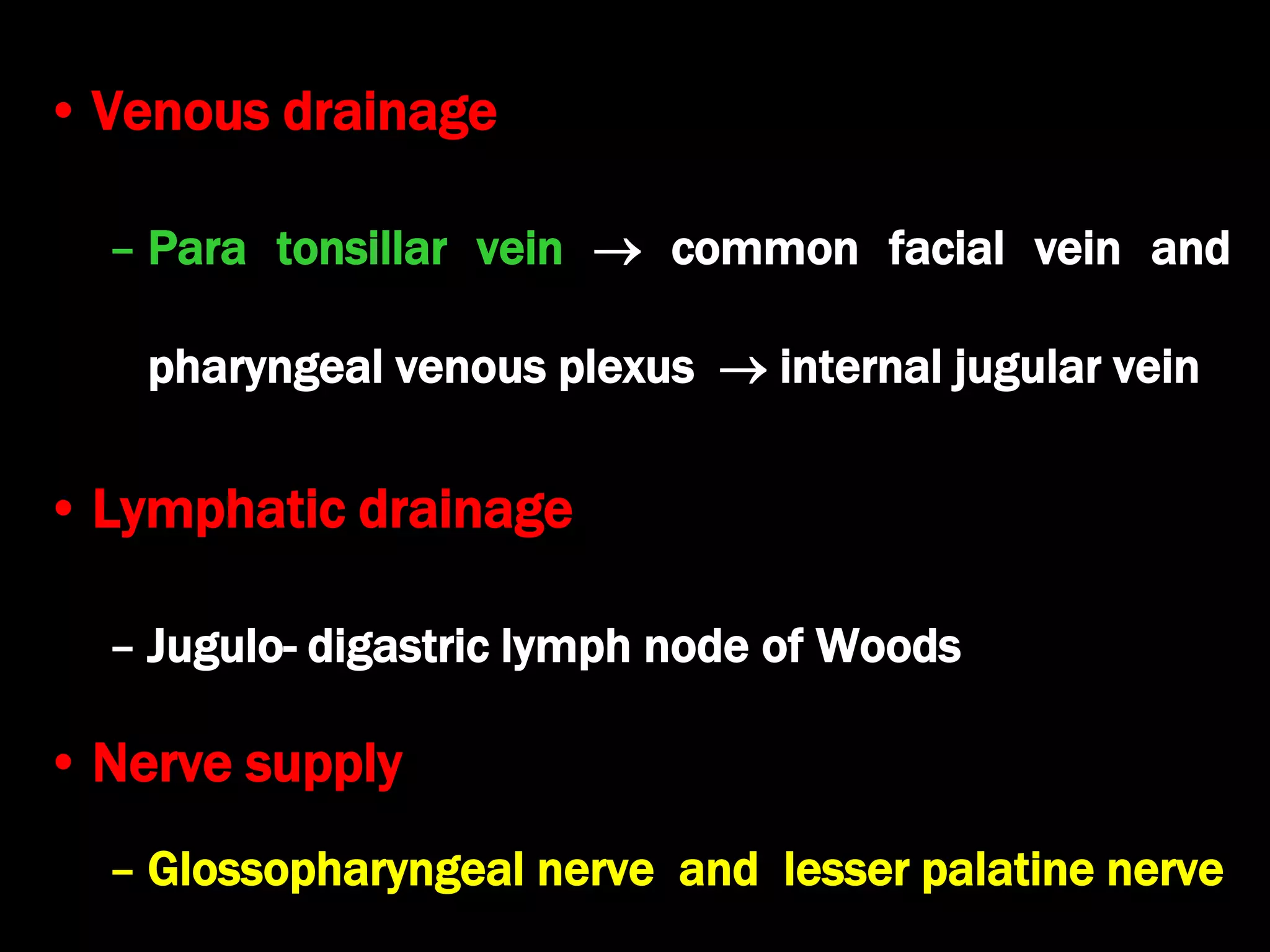
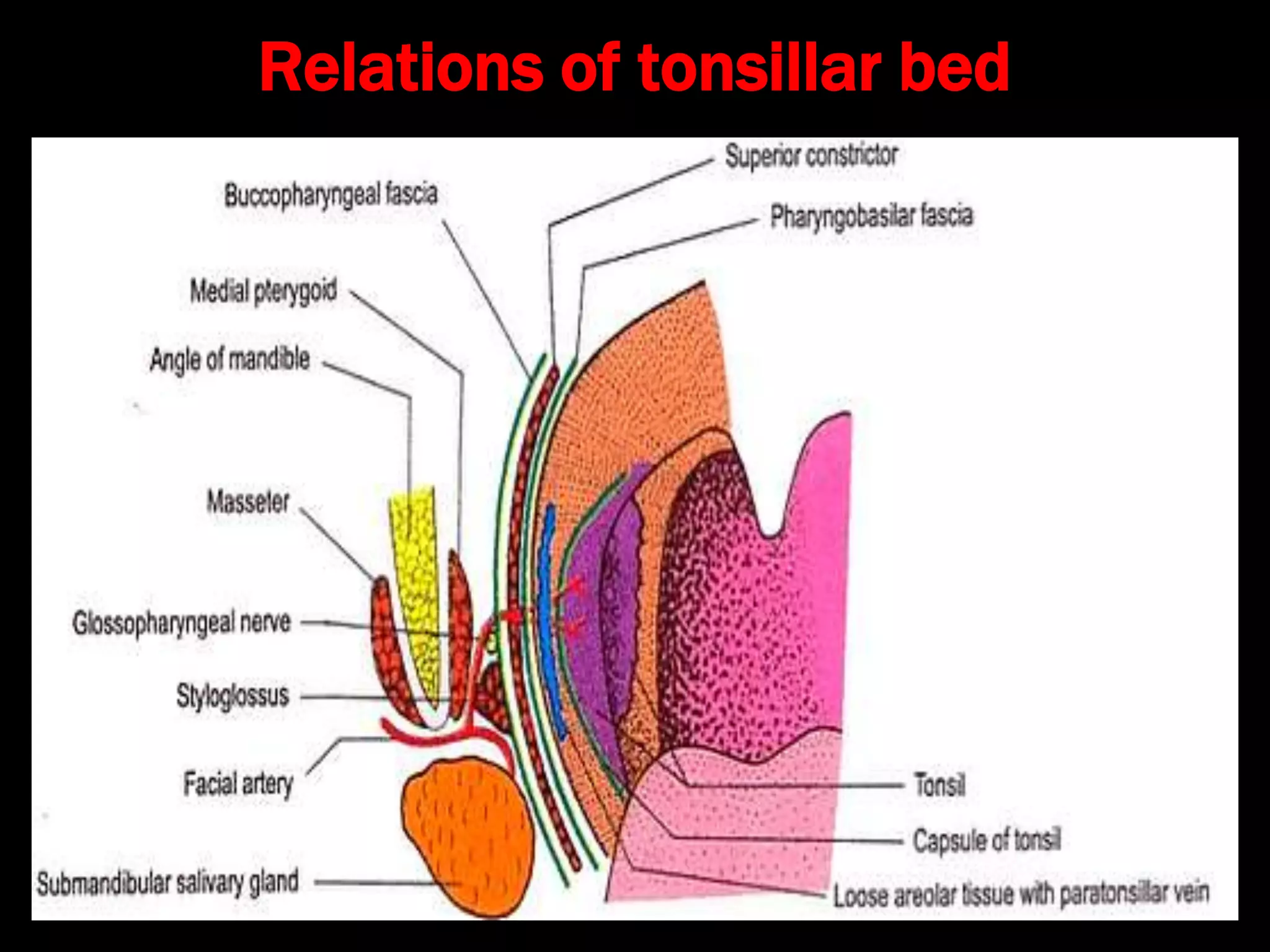
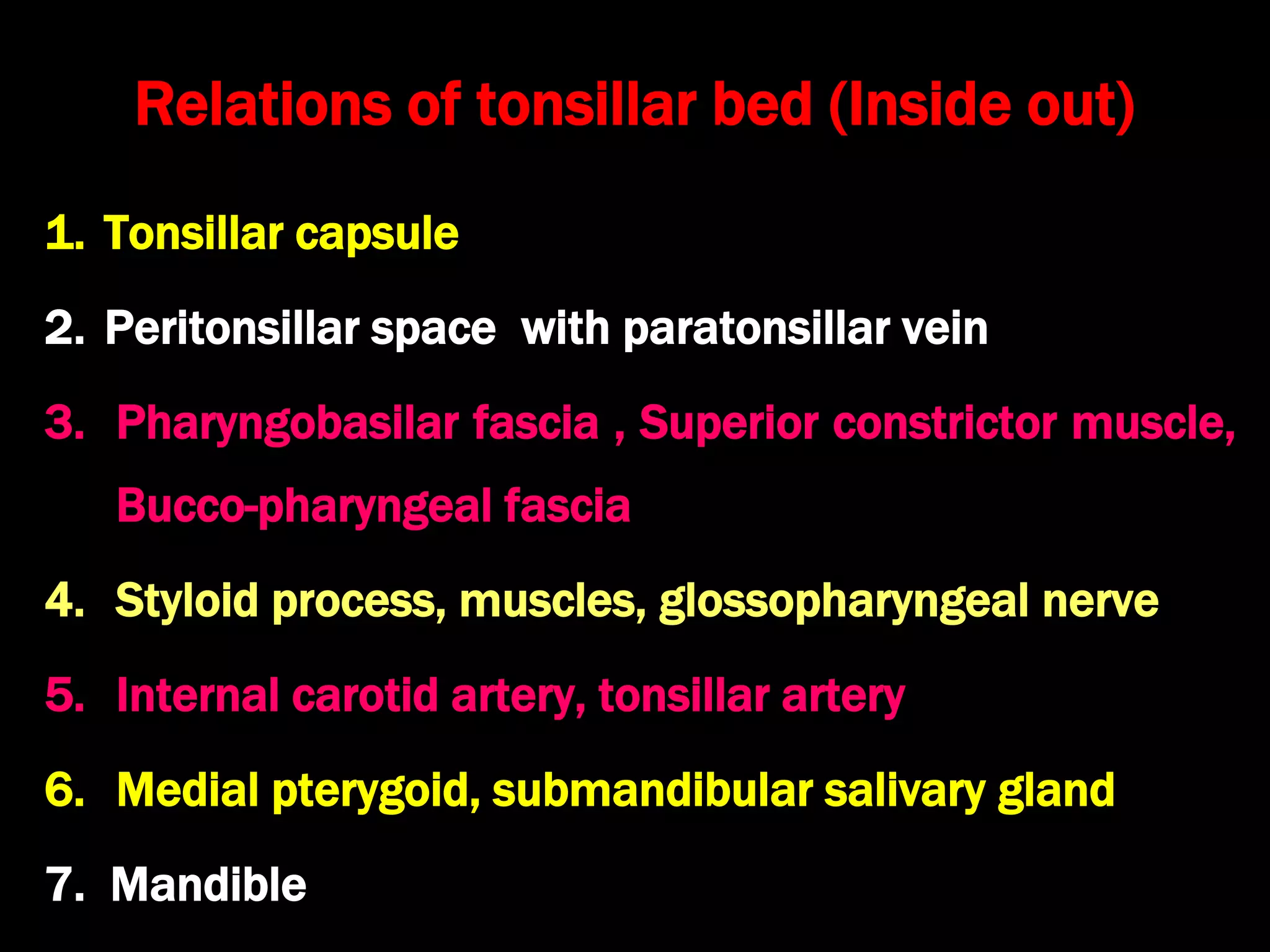
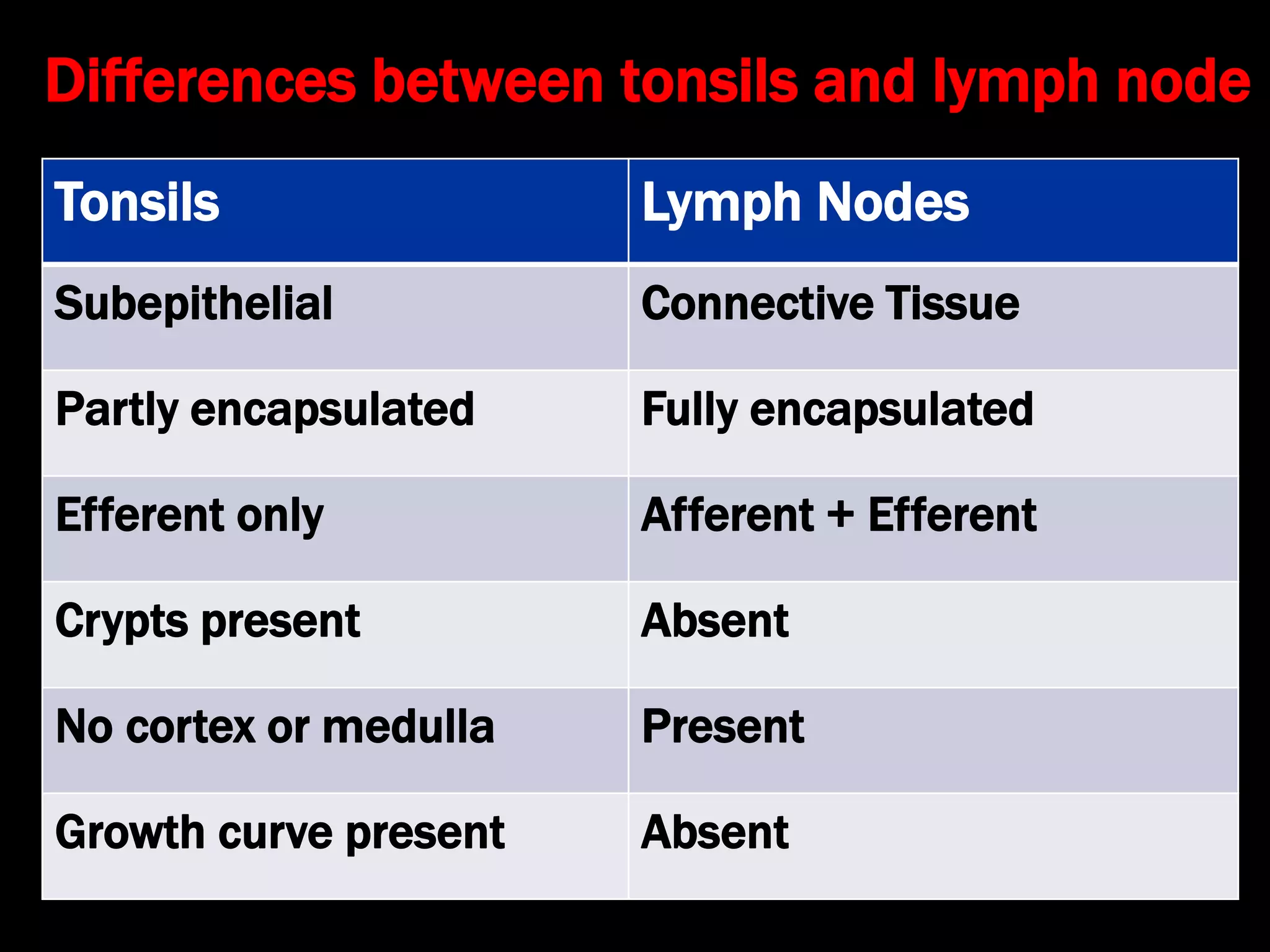
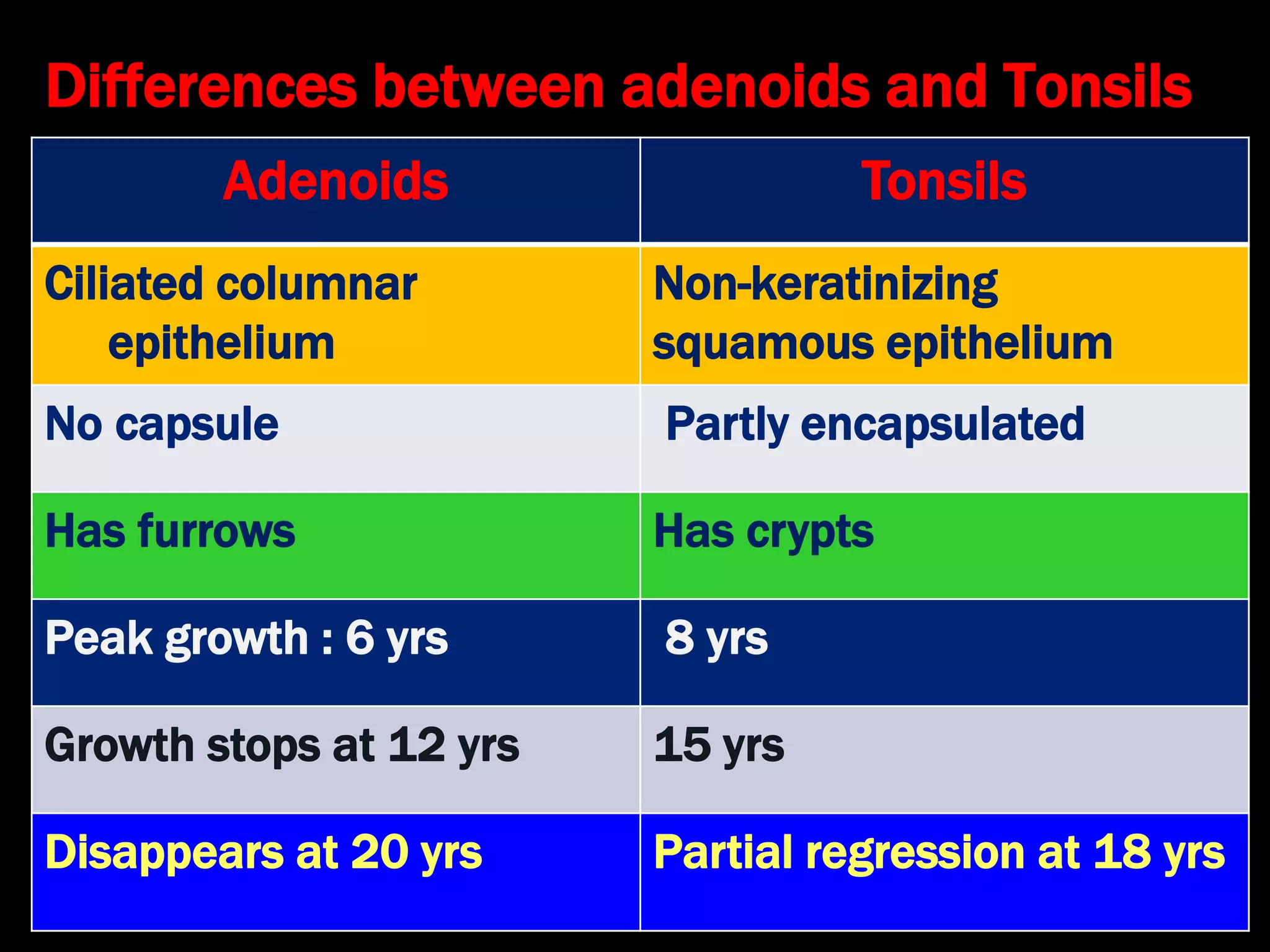
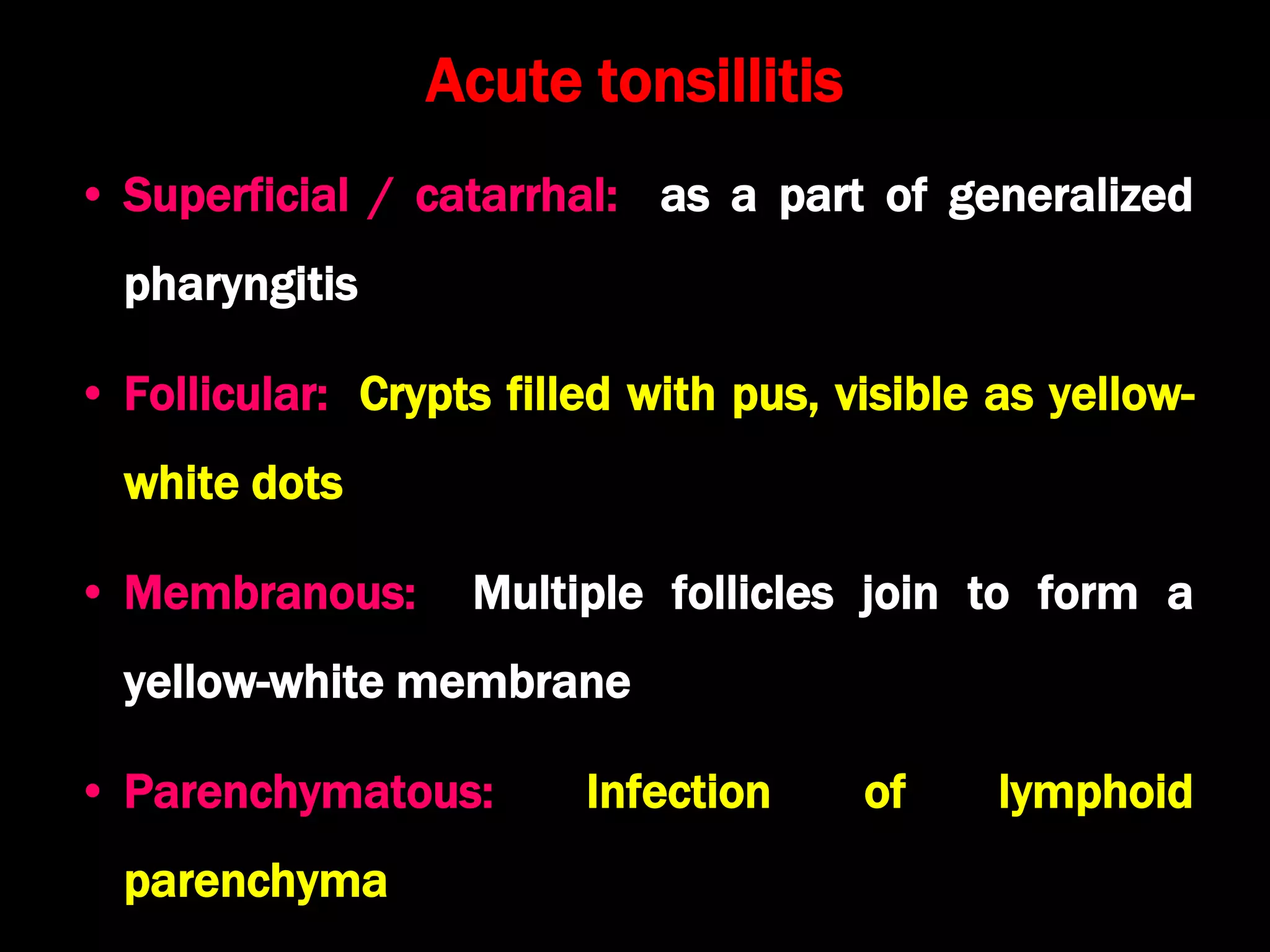
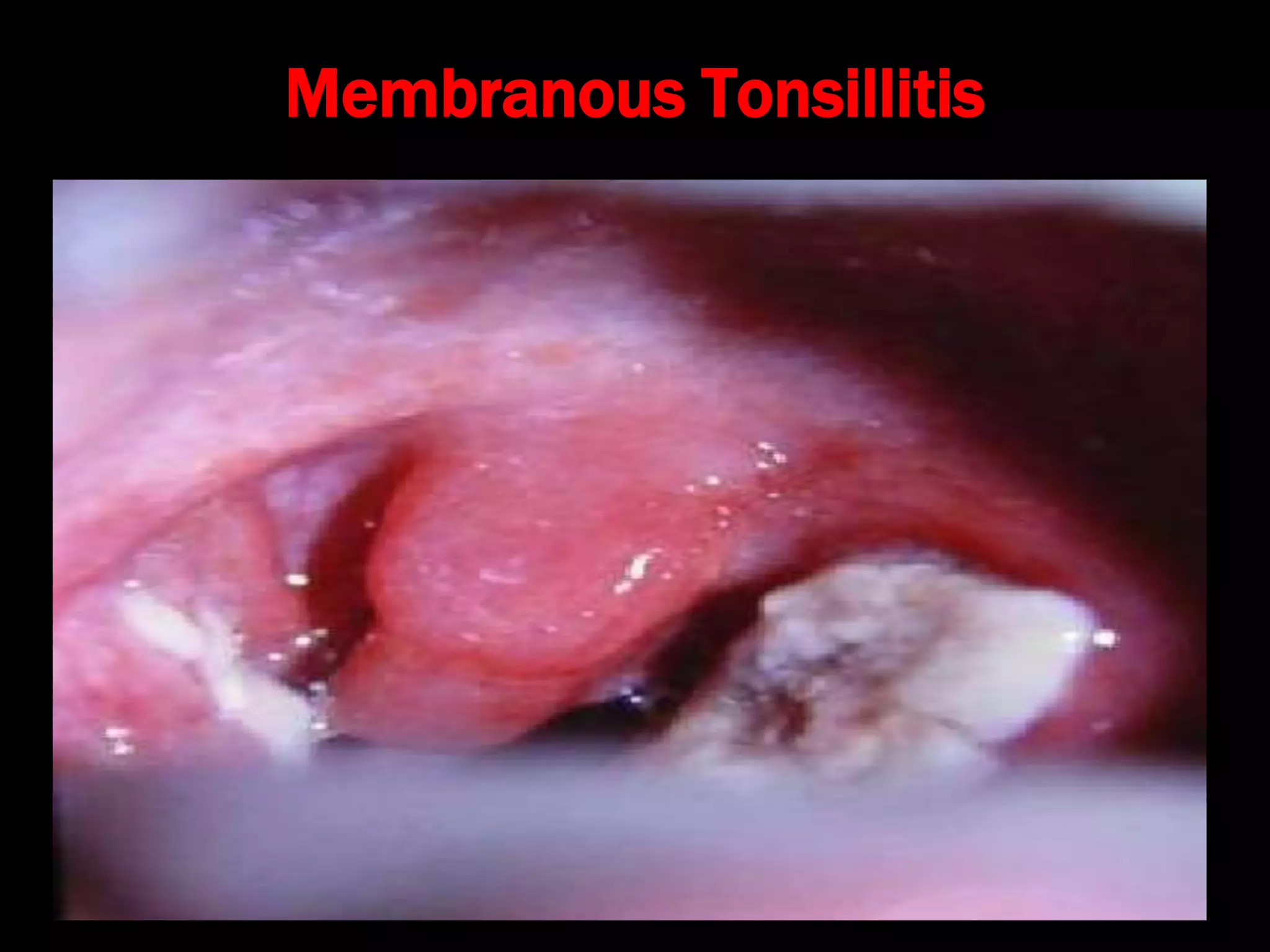
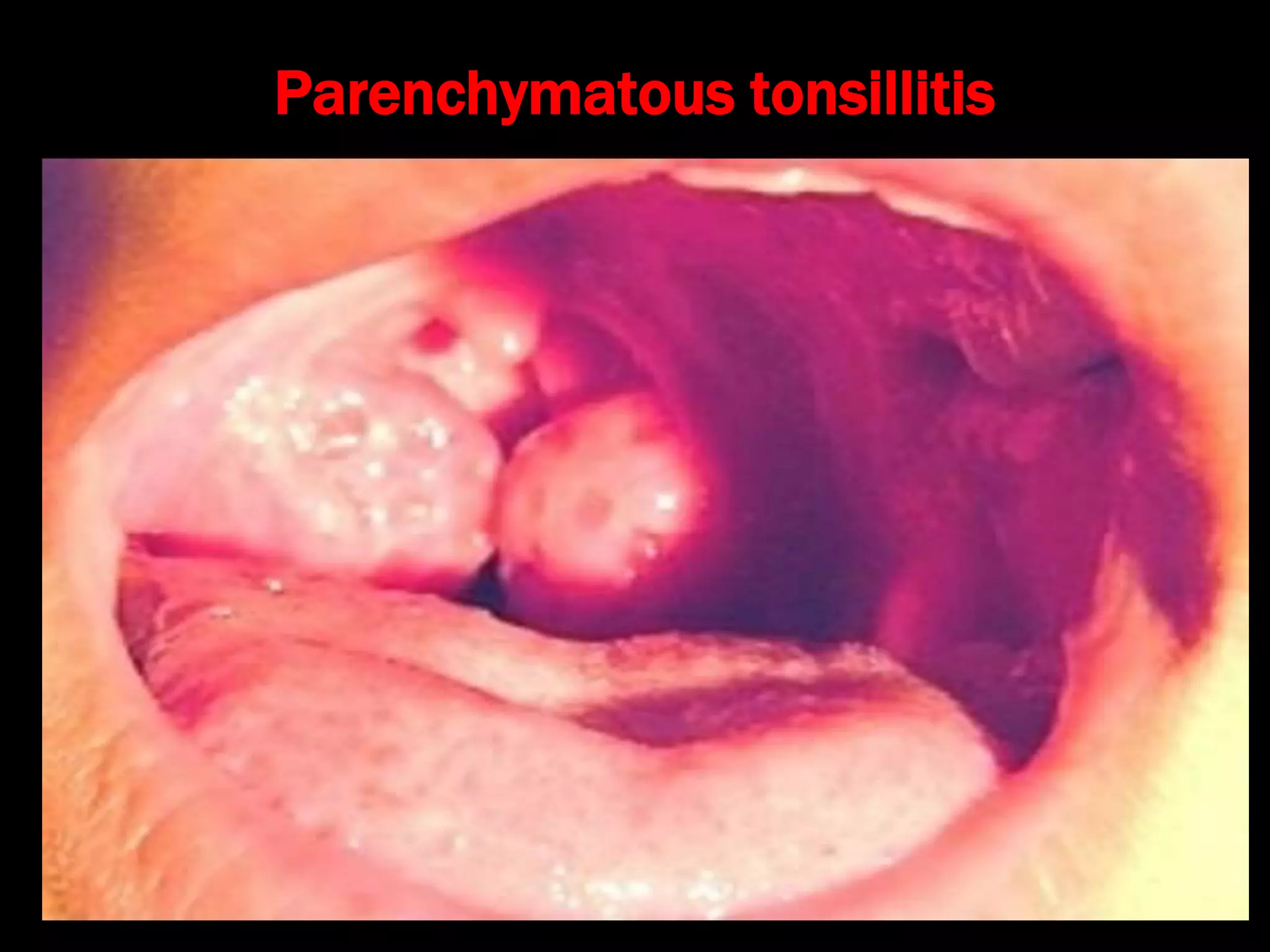
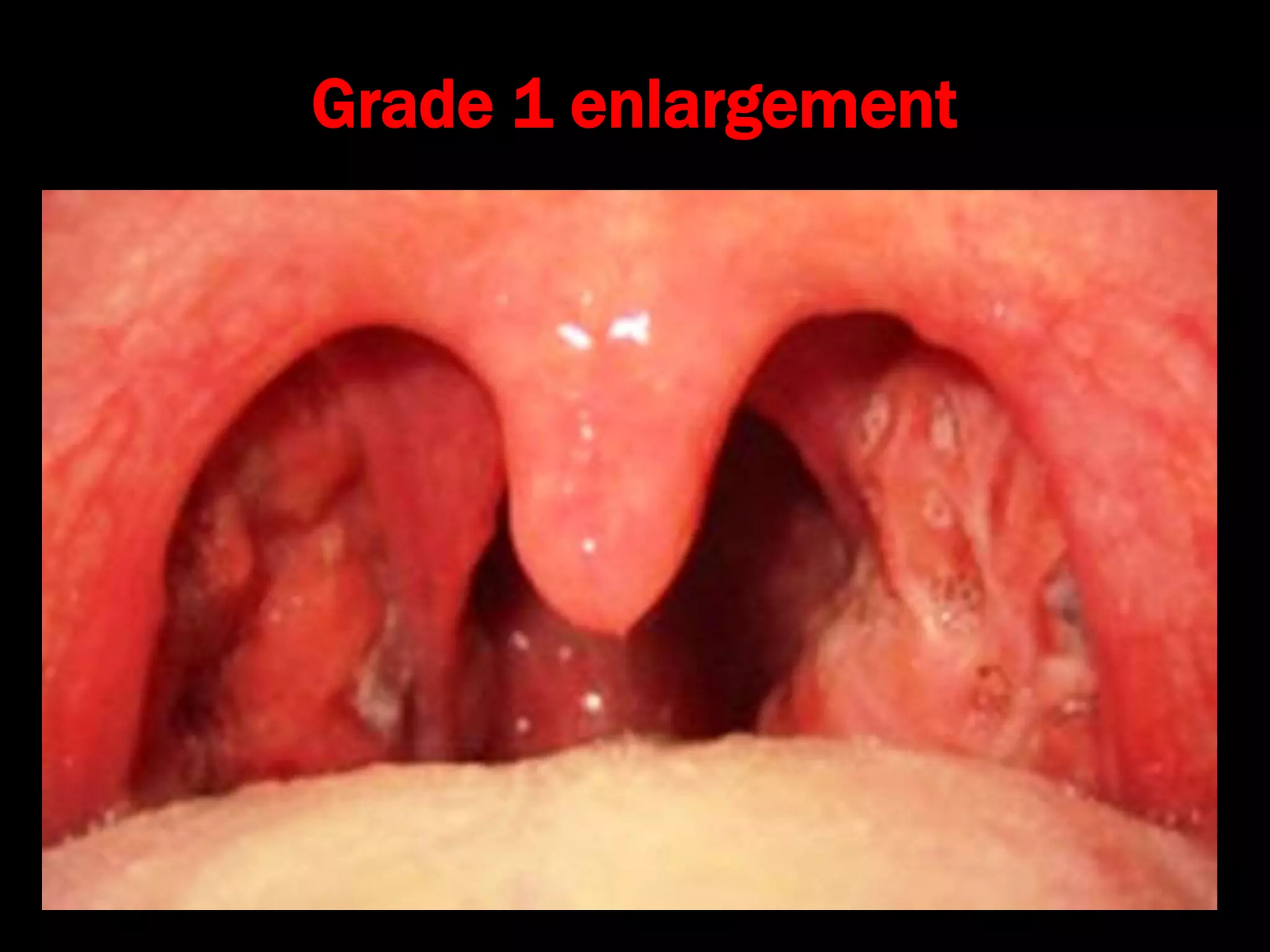
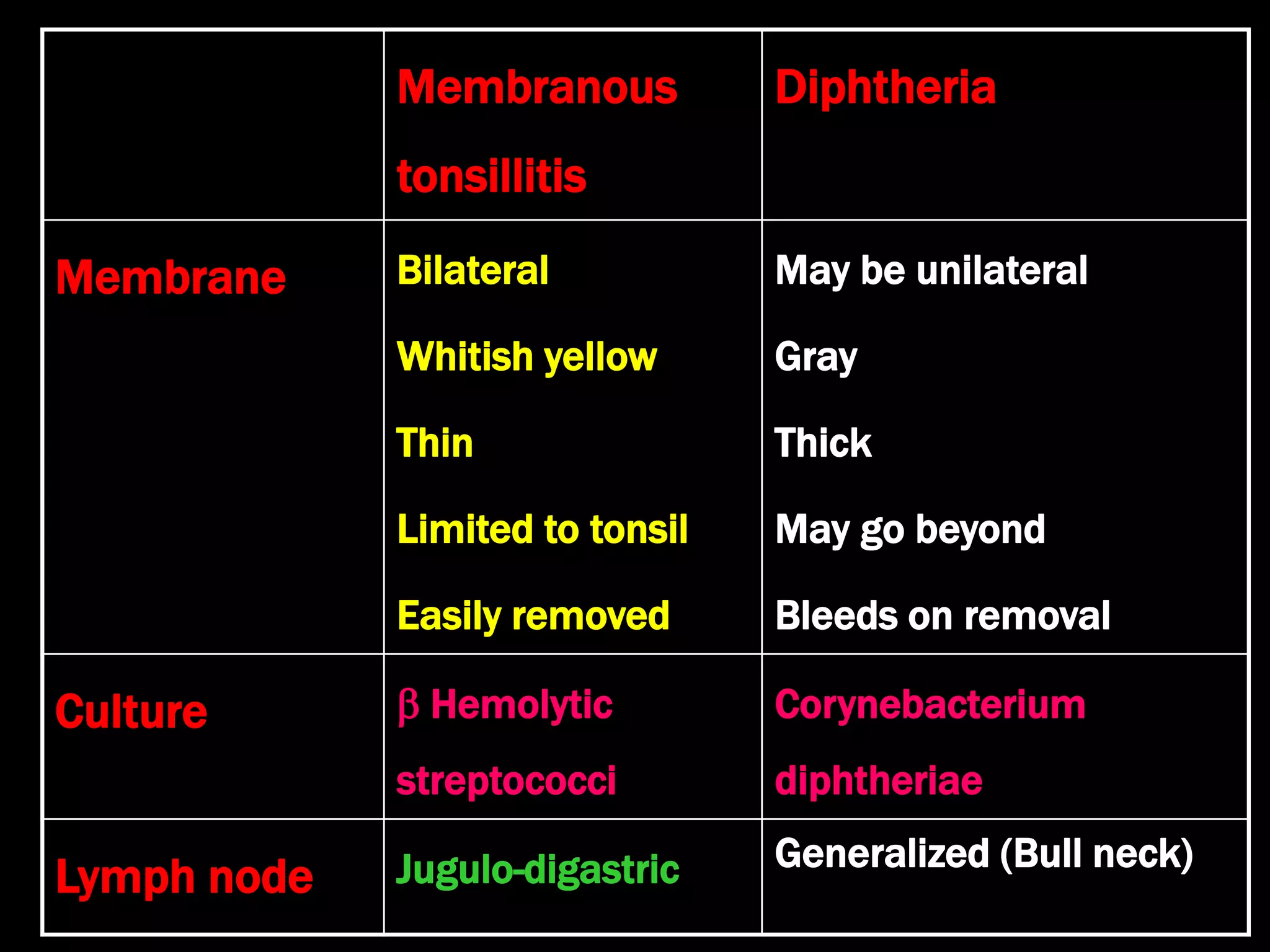
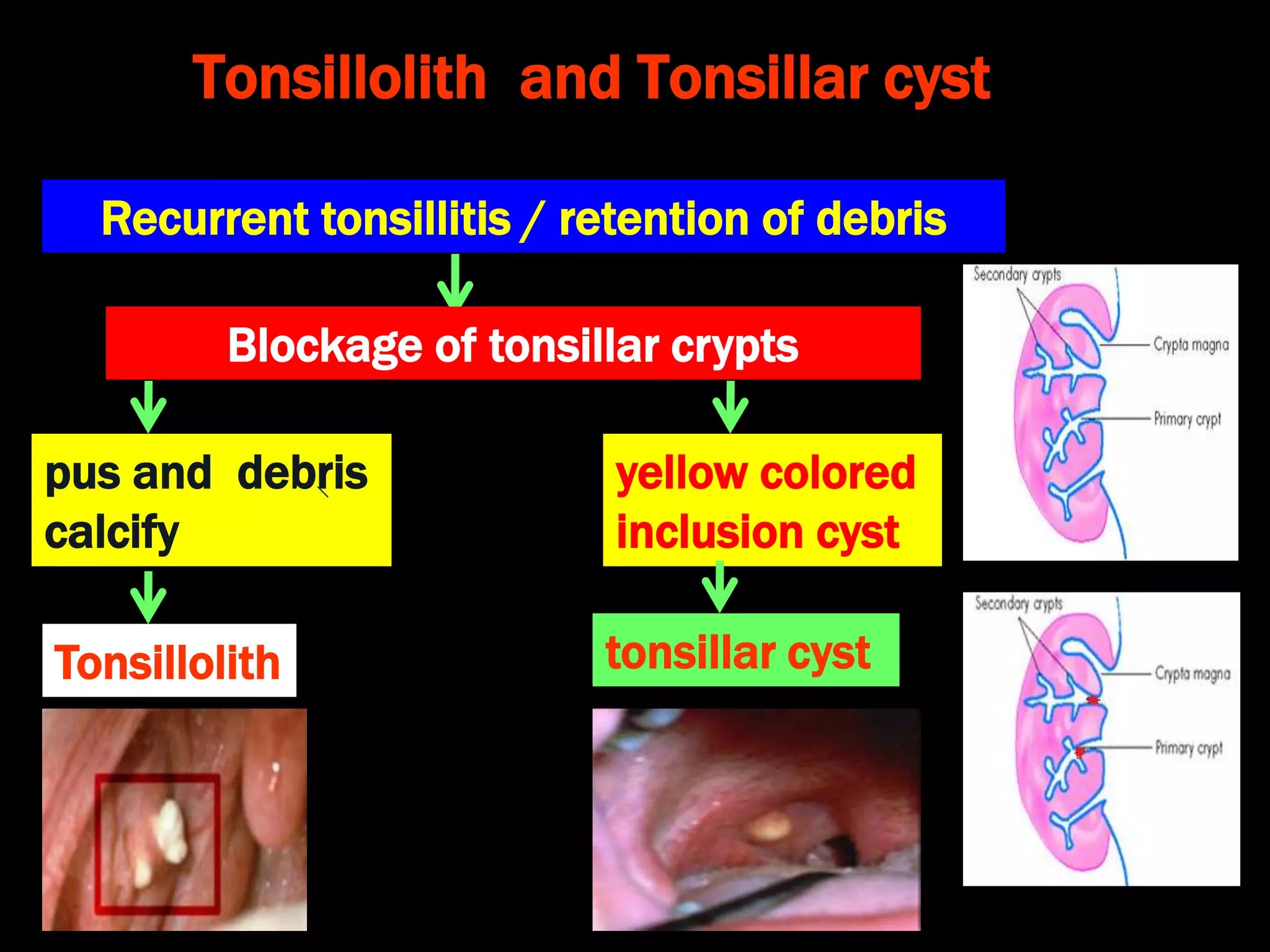
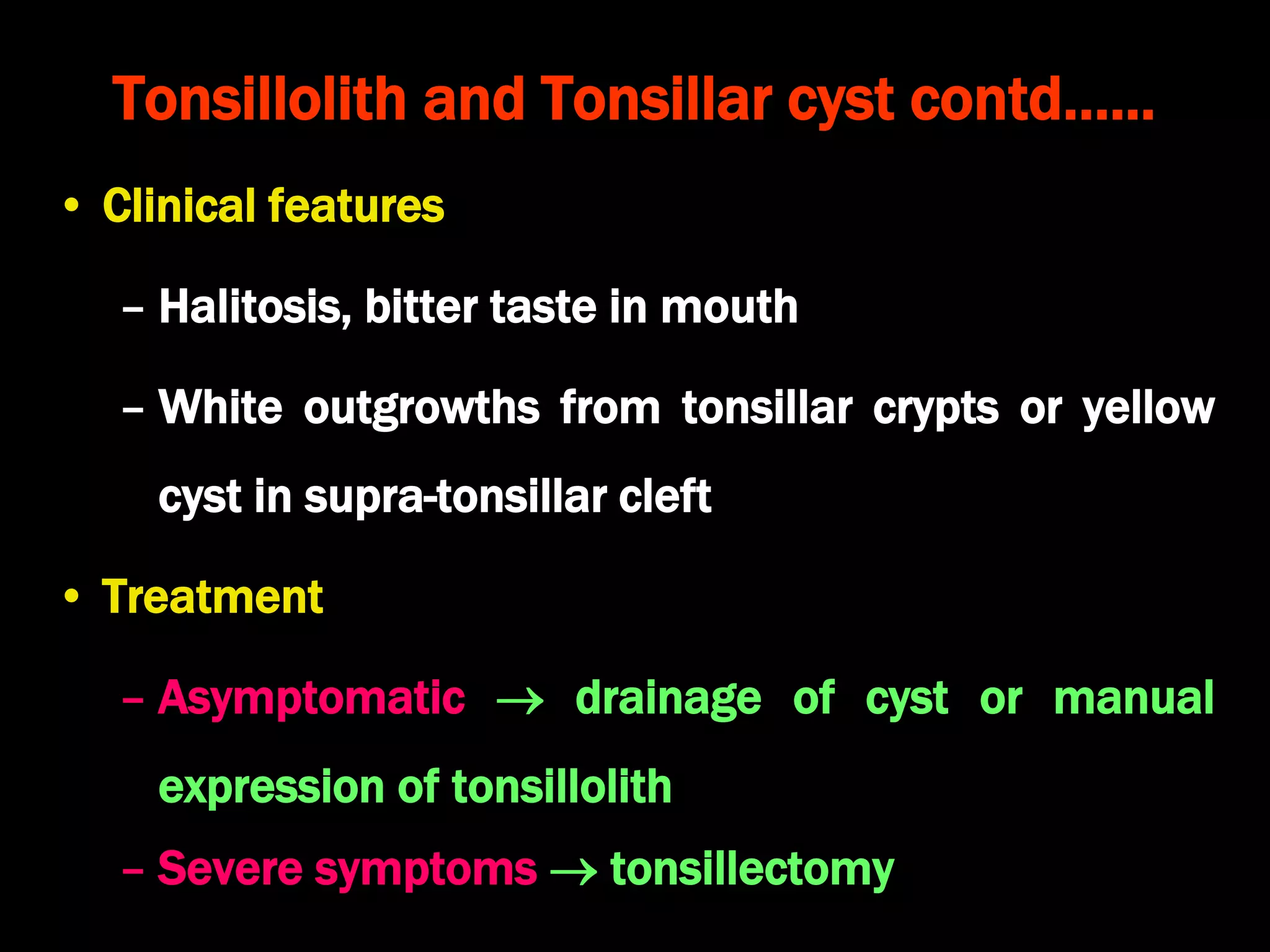
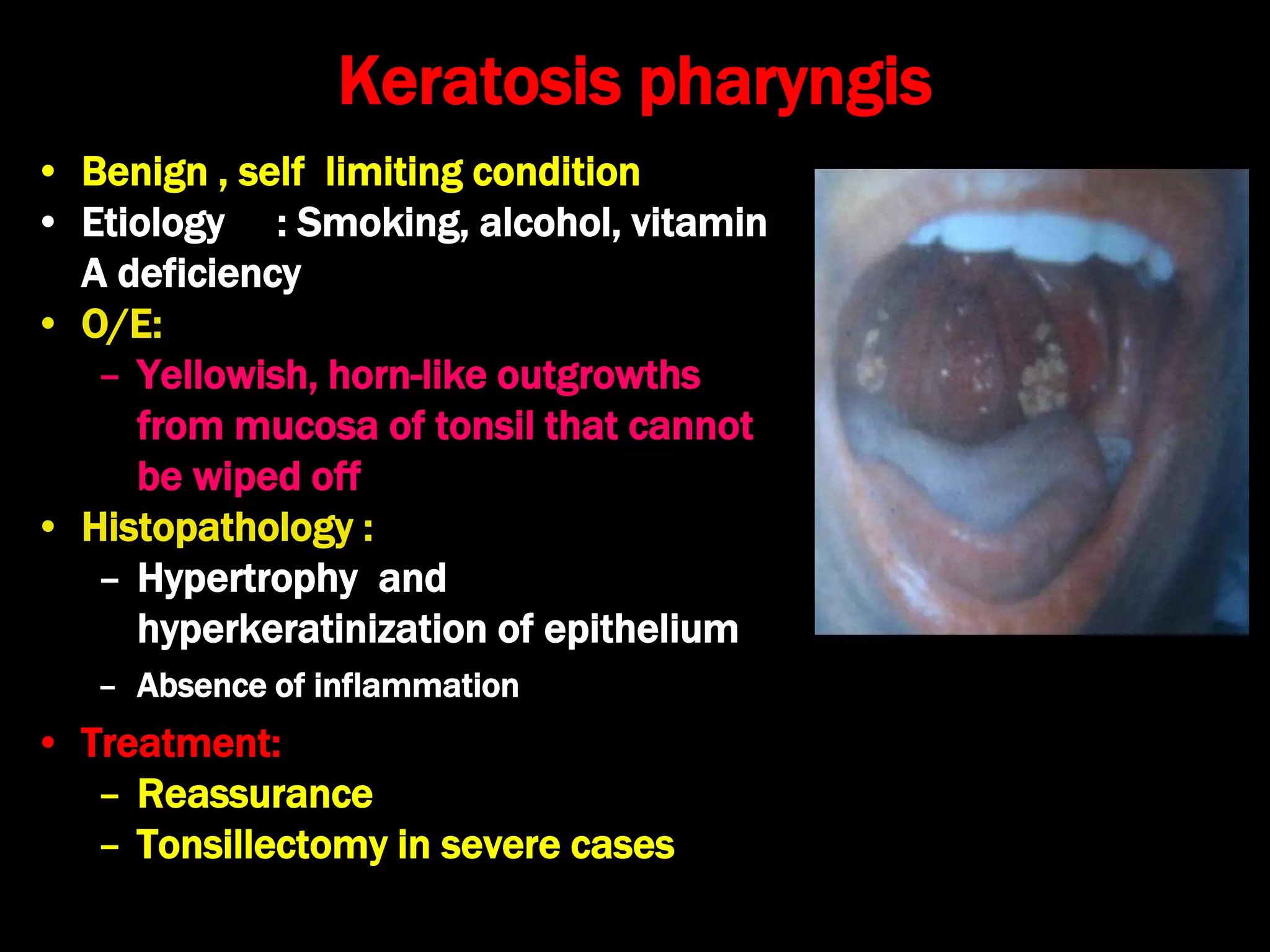
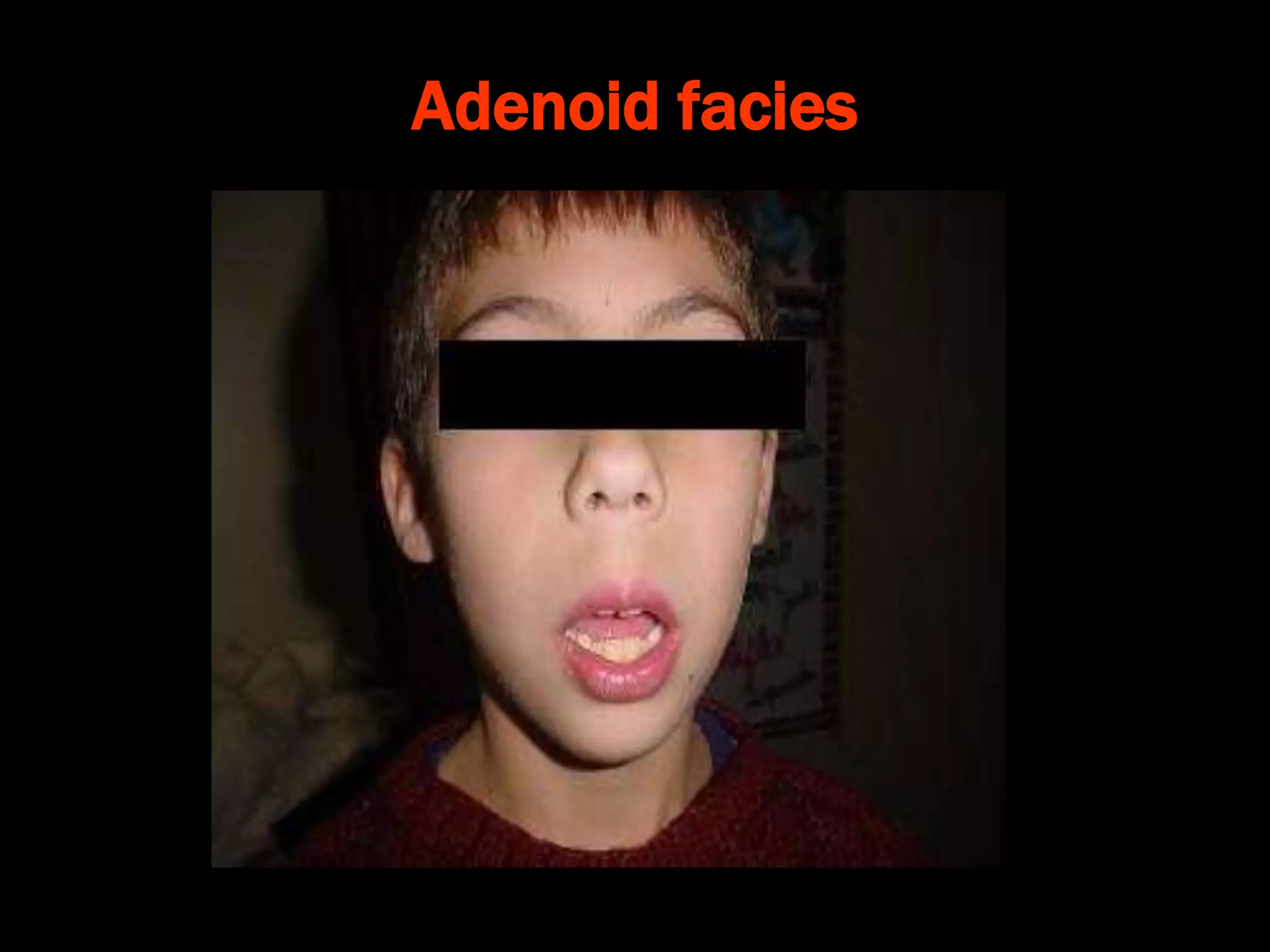
The document provides a comprehensive overview of tonsils and adenoids, including their anatomy, arterial supply, differences, and types of tonsillitis. It discusses clinical features, complications, treatment options, and differential diagnoses associated with tonsillitis and adenoid hypertrophy. Additionally, it covers management strategies such as medications and surgical interventions for severe cases.