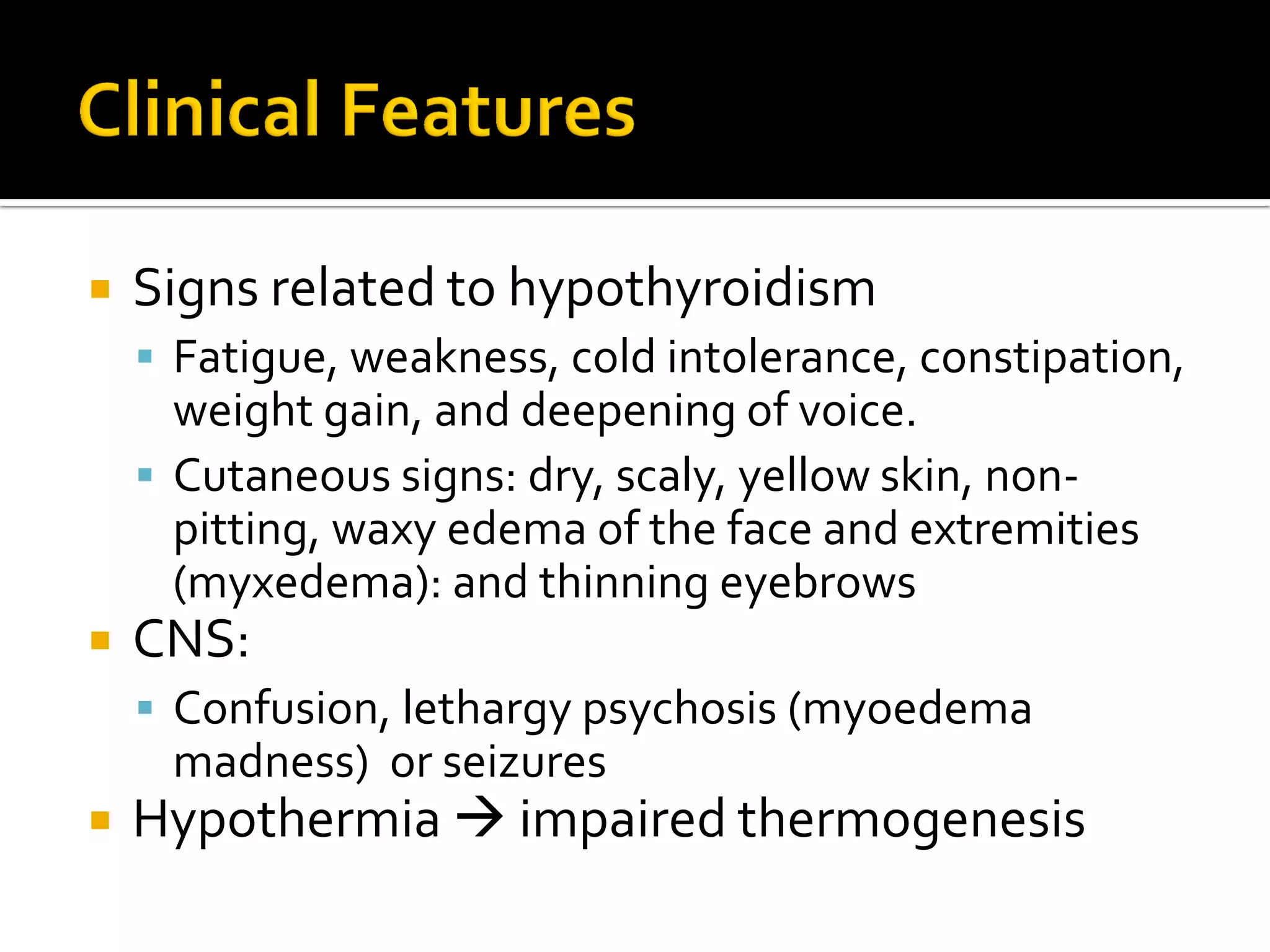
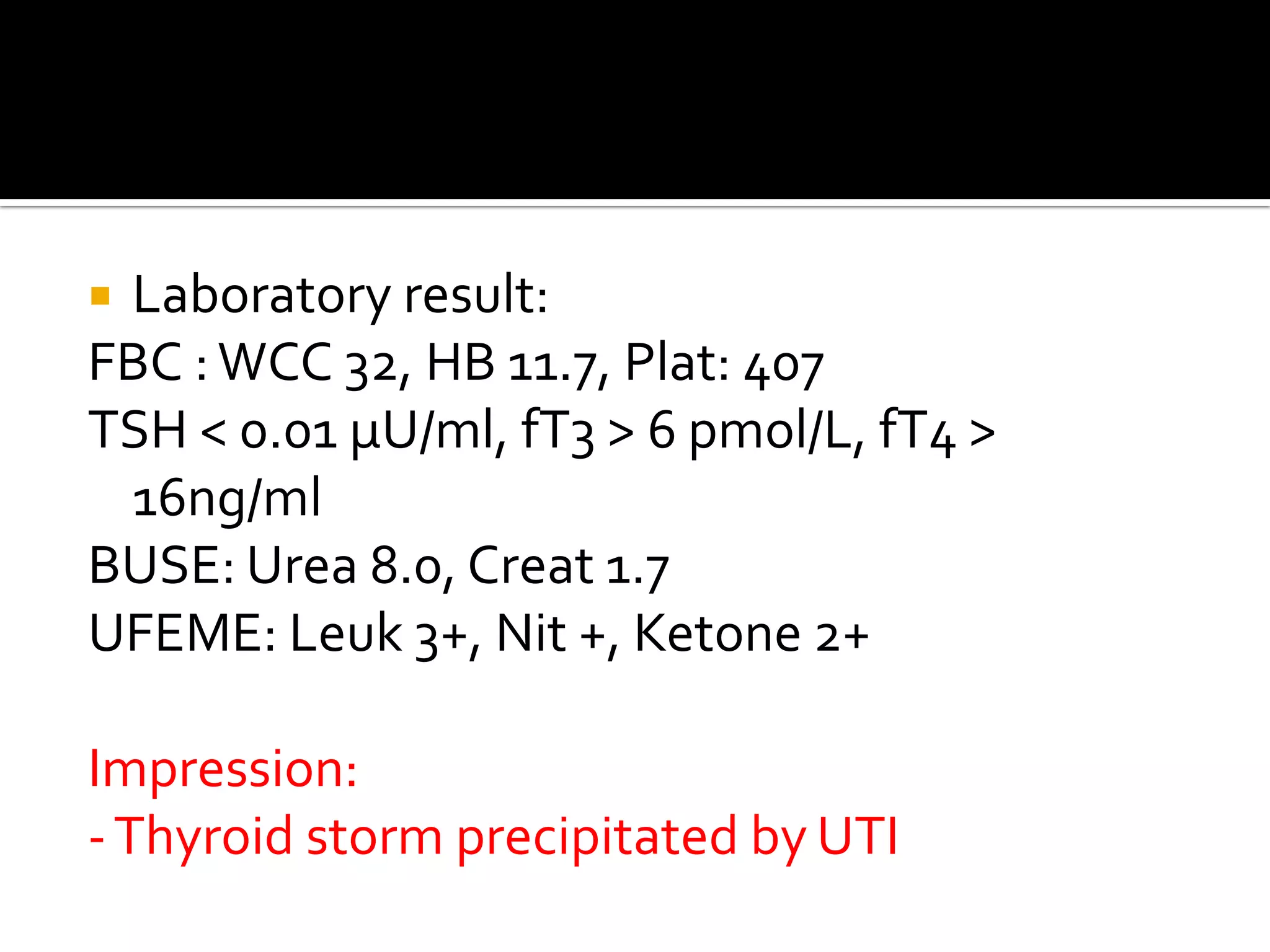
A 27-year-old female master's student presented with back and flank pain, nausea, vomiting and palpitations. She had a history of Graves' disease and was non-compliant with medications. Examination found a temperature of 40°C, heart rate of 132, enlarged thyroid with bruit. Laboratory results showed hyperthyroidism and a UTI. Her Burch-Wartofsky score was 75, highly suggestive of thyroid storm precipitated by the UTI given her non-compliance with anti-thyroid medications. She required critical care management in hospital.