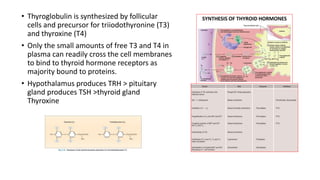
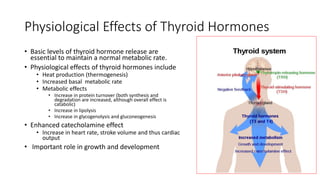
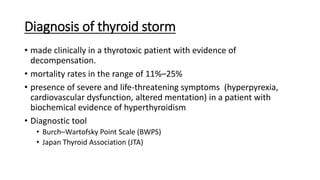
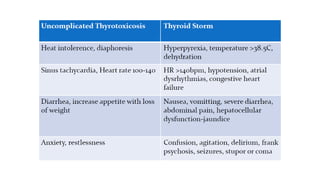
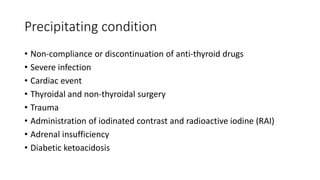
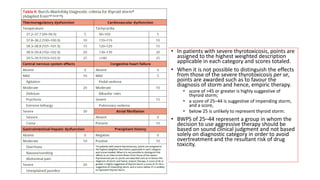
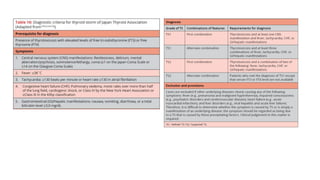
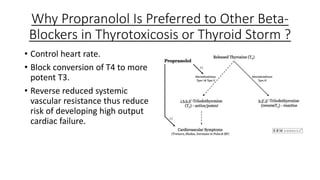
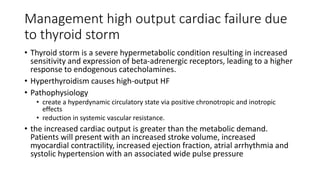
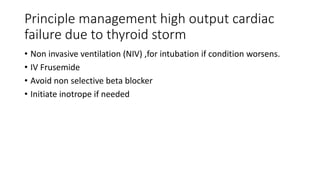
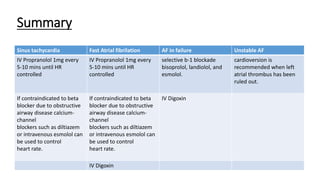
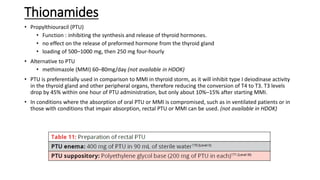
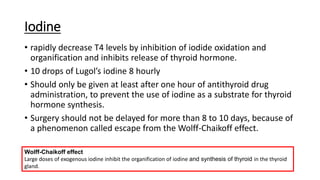
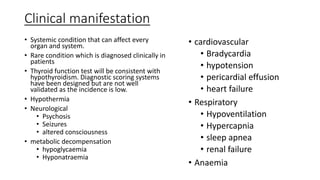
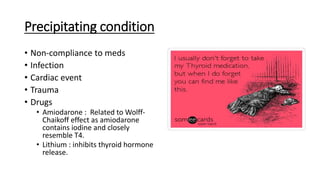
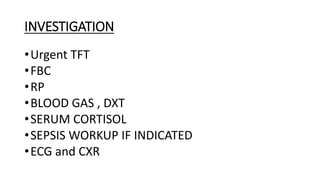
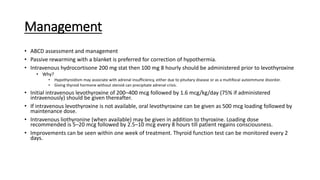
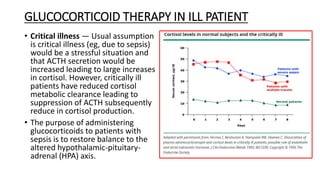
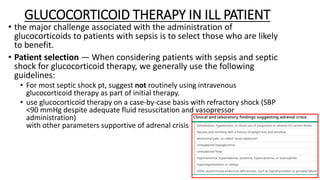
This document discusses thyroid emergencies including thyroid storm and myxedema coma. It provides details on the synthesis and effects of thyroid hormones, diagnosis of thyroid storm using the Burch-Wartofsky Point Scale and Japan Thyroid Association criteria, and management principles for thyroid storm including beta blockers, antithyroid medications, corticosteroids, iodine, and definitive therapy. Precipitating factors and management of myxedema coma are also summarized.