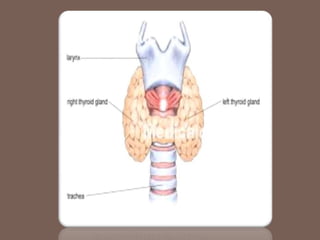
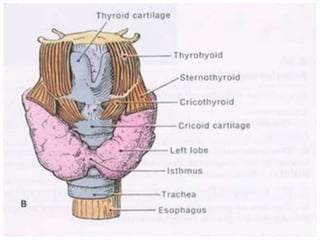
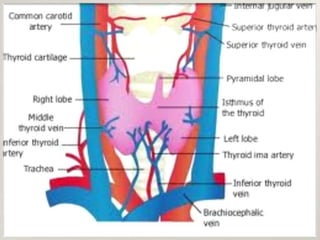
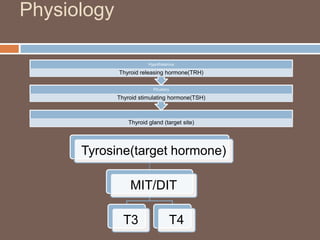
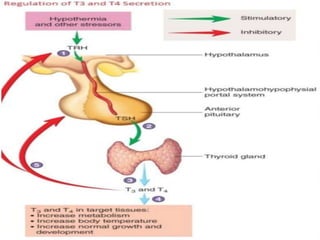
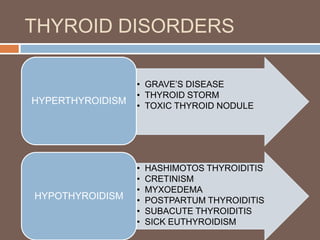
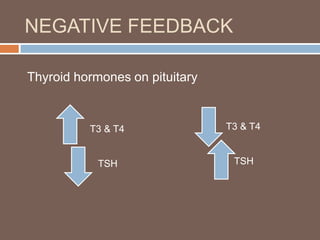
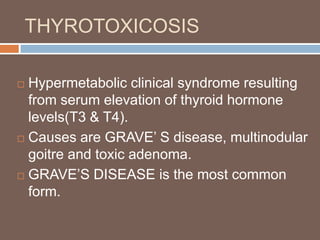
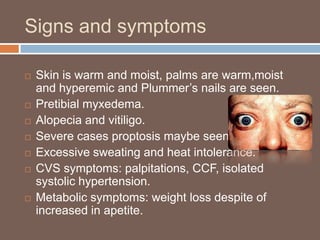
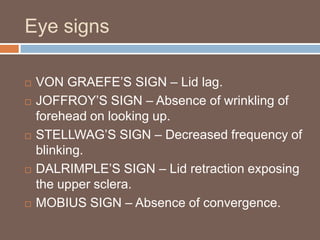
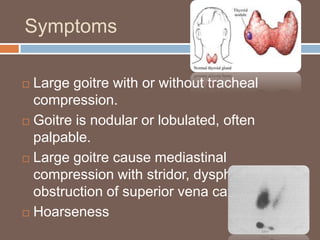
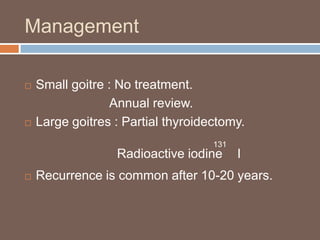
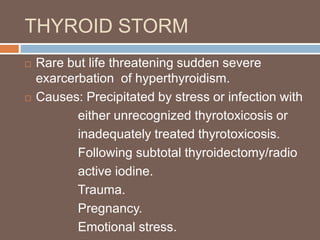
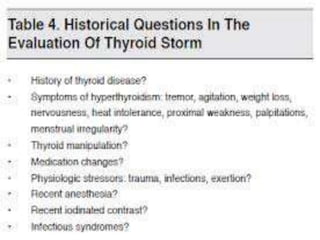
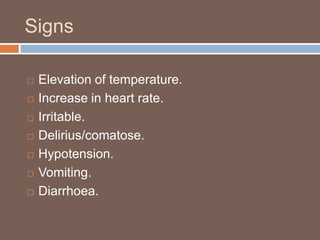
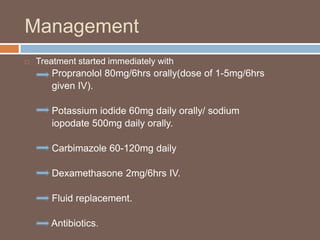
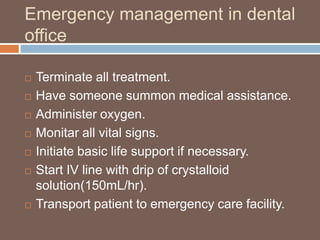
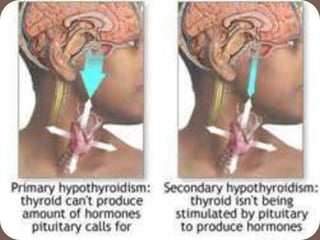
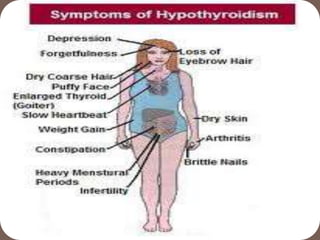
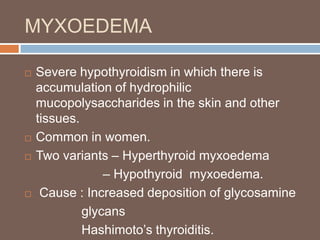
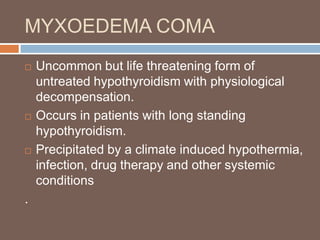
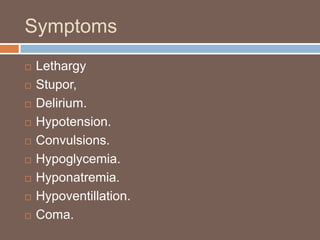
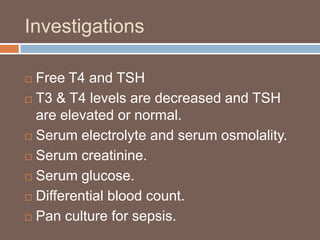
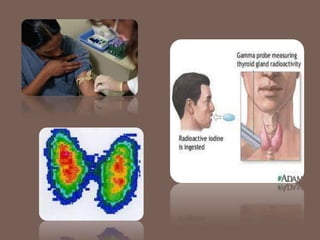
The document presents an overview of thyroid disorders, focusing on hyperfunction (such as Graves' disease and thyroid storm) and hypofunction (including hypothyroidism and related conditions like Hashimoto's thyroiditis). It details the thyroid gland's anatomy, physiology, symptoms, diagnostic methods, and management strategies for various conditions. The document emphasizes the importance of early detection and treatment of thyroid disorders.