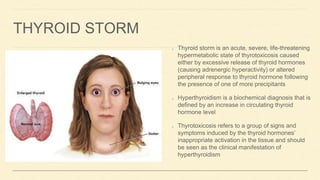
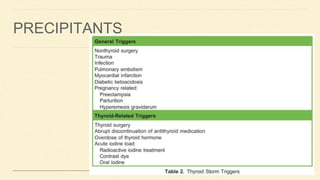
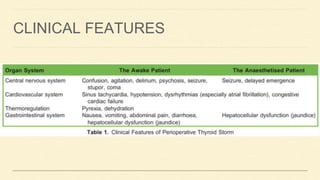
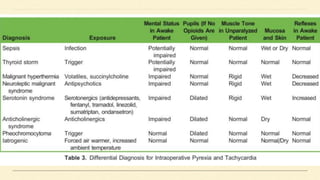
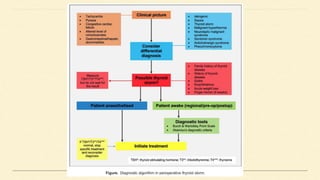
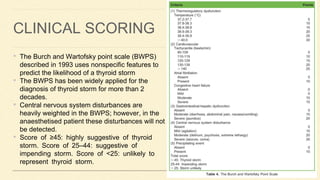
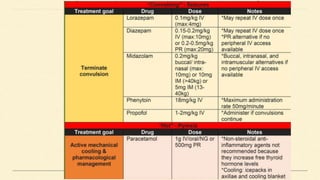
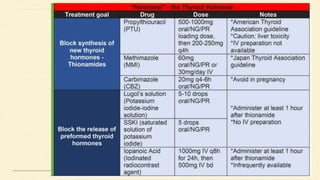
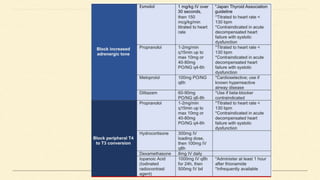
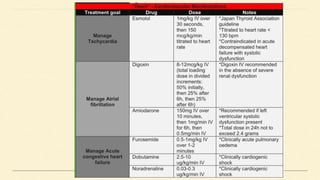
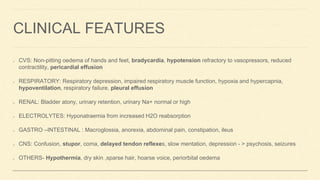
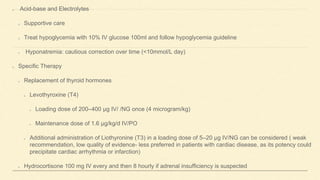
The document discusses two critical thyroid emergencies: thyroid storm and myxedema coma. It outlines the diagnosis criteria, clinical features, and management strategies for each condition, emphasizing the importance of early recognition and treatment to reduce mortality rates. The management involves supportive care, hormone replacement, and addressing underlying precipitating factors.