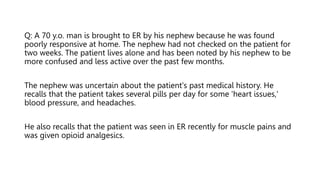
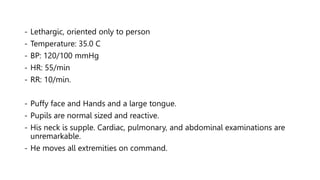
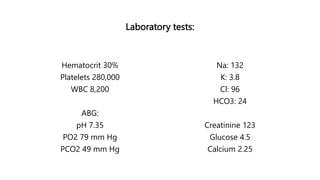
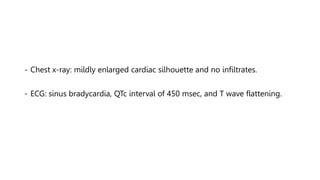
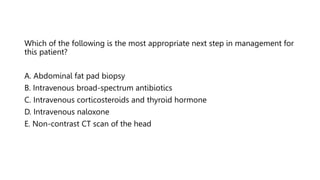
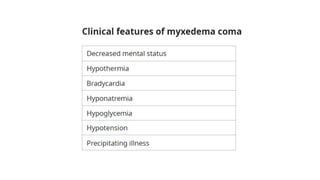
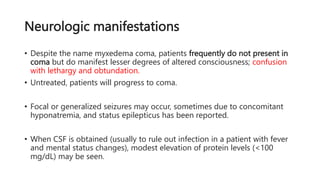
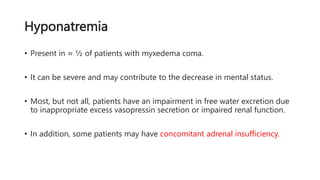
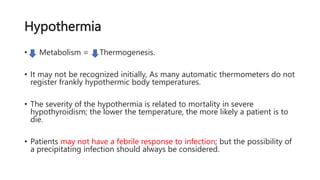
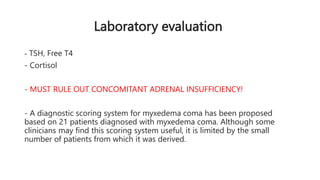
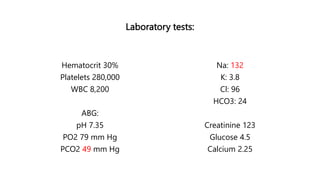
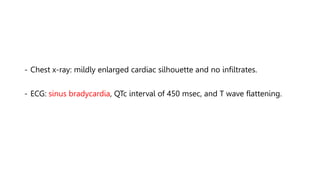
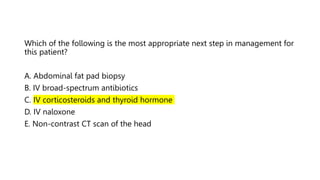
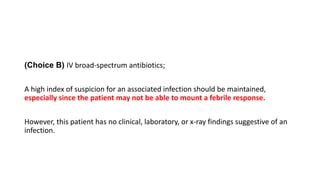
The document discusses a case of a 70-year-old man presenting in a poorly responsive state, potentially indicative of myxedema coma due to severe hypothyroidism. Key features pointing to this condition include lethargy, hypothermia, bradycardia, and characteristic physical symptoms such as facial puffiness. The management of myxedema coma involves immediate administration of thyroid hormones, glucocorticoids, and supportive measures to improve the patient's condition and reduce mortality risks.