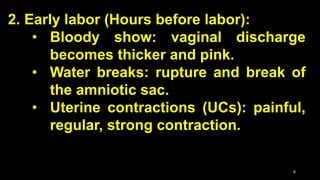
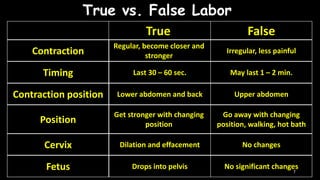
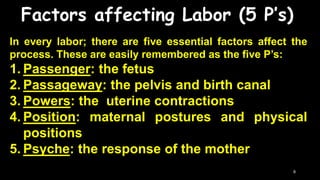
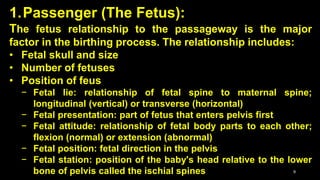
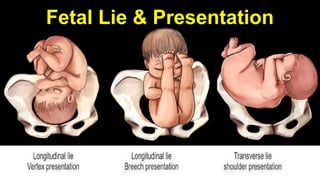
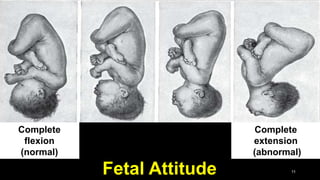
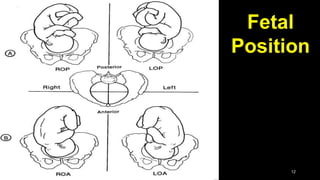
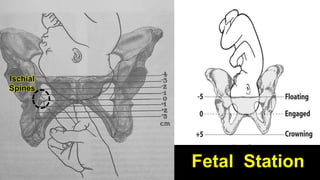
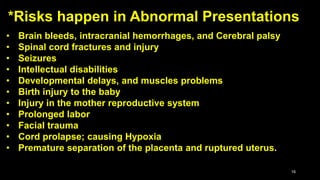
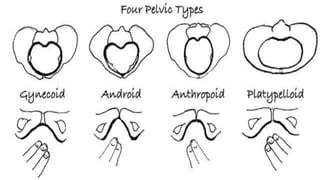
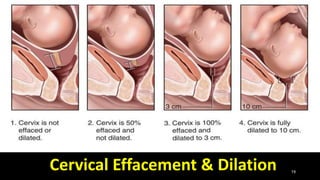
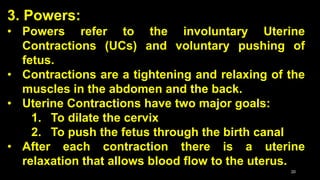
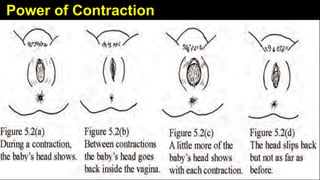
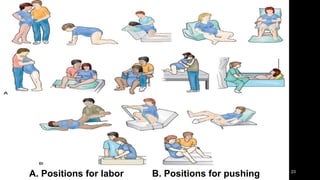
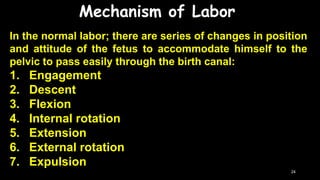
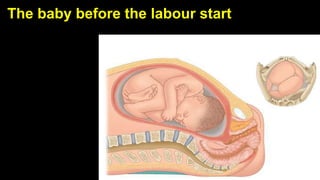
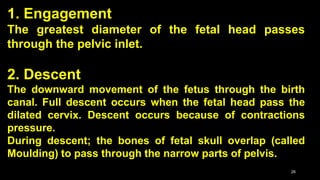
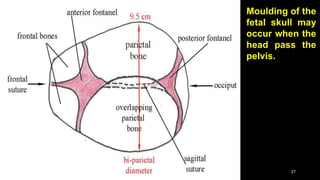
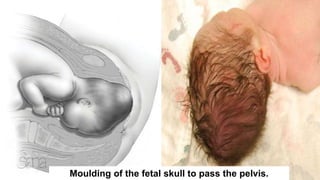
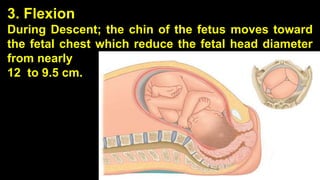
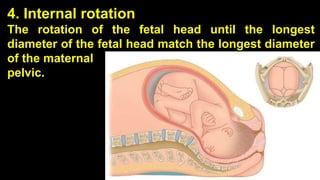
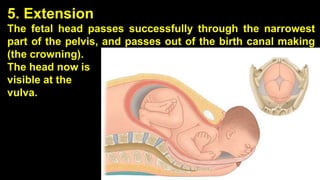
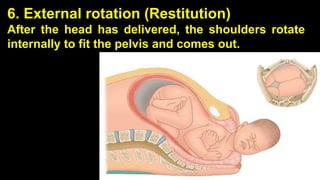
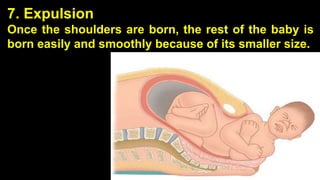
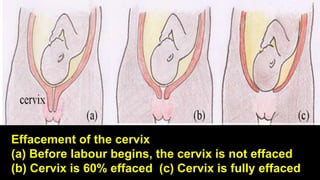
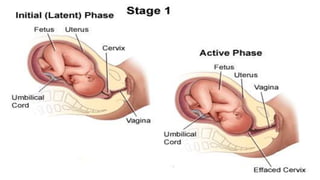
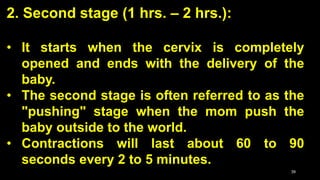
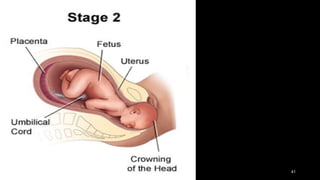
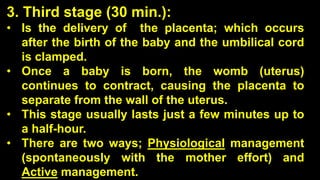
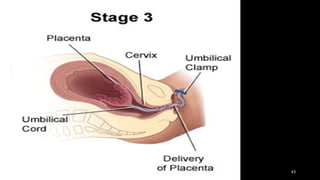
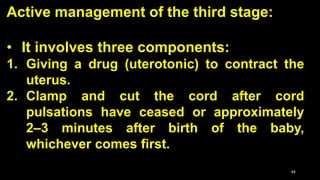
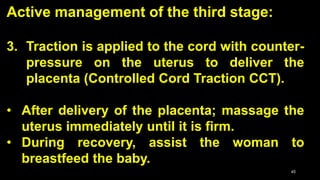
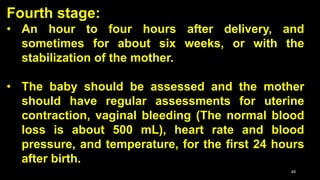
The document outlines the process of labor, defining it as the physiological process where the fetus and associated membranes are expelled from the uterus between 38 and 42 weeks of pregnancy. It describes the stages of labor, normal labor characteristics, signs of labor, and key influencing factors, known as the five p's: passenger, passageway, powers, position, and psyche. The document also details the mechanisms and stages of labor from cervical dilation to the delivery of the placenta and the postpartum recovery period.