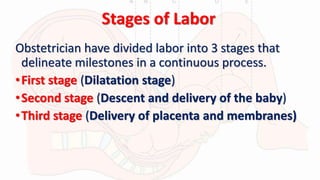
Labor and delivery involves three stages:
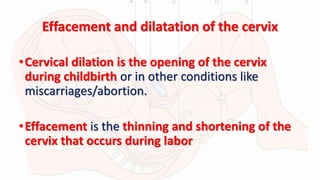
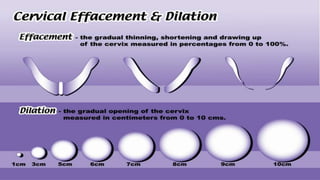
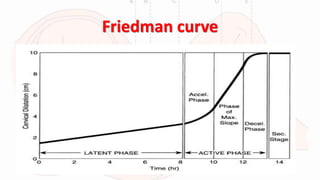
1) The first stage begins with contractions and ends with full cervical dilation. It includes early latent and active phases of dilation.
2) The second stage begins at full dilation and ends with baby's delivery. It involves baby's descent and delivery.
3) The third stage begins after delivery and ends with placenta delivery, usually within 30 minutes but sometimes requiring intervention.