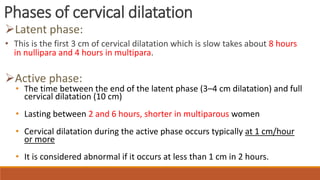
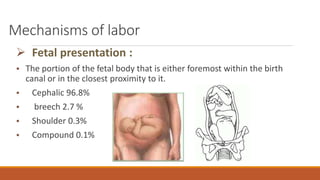
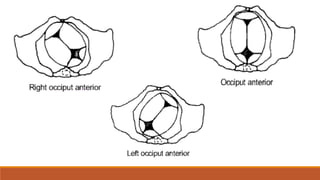
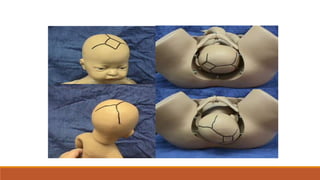
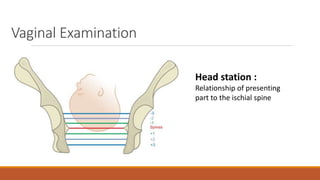
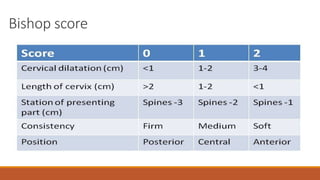
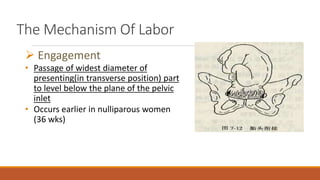
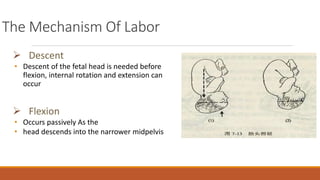
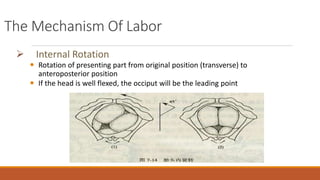
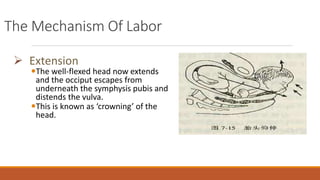
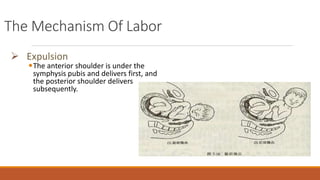
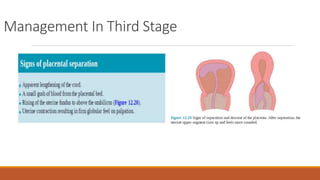
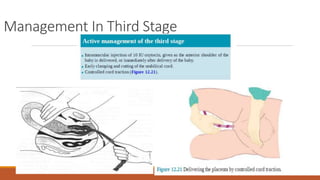
Normal labor and delivery involves 3 stages: 1) dilation of the cervix, 2) delivery of the baby, and 3) delivery of the placenta. The fetus moves through the birth canal via engagement, descent, flexion, internal rotation, extension, and external rotation. Labor is considered normal if it is spontaneous in onset, involves a single cephalic fetus at term, lasts less than 12 hours for first-time mothers and 8 hours for others, and results in an unassisted vaginal birth.