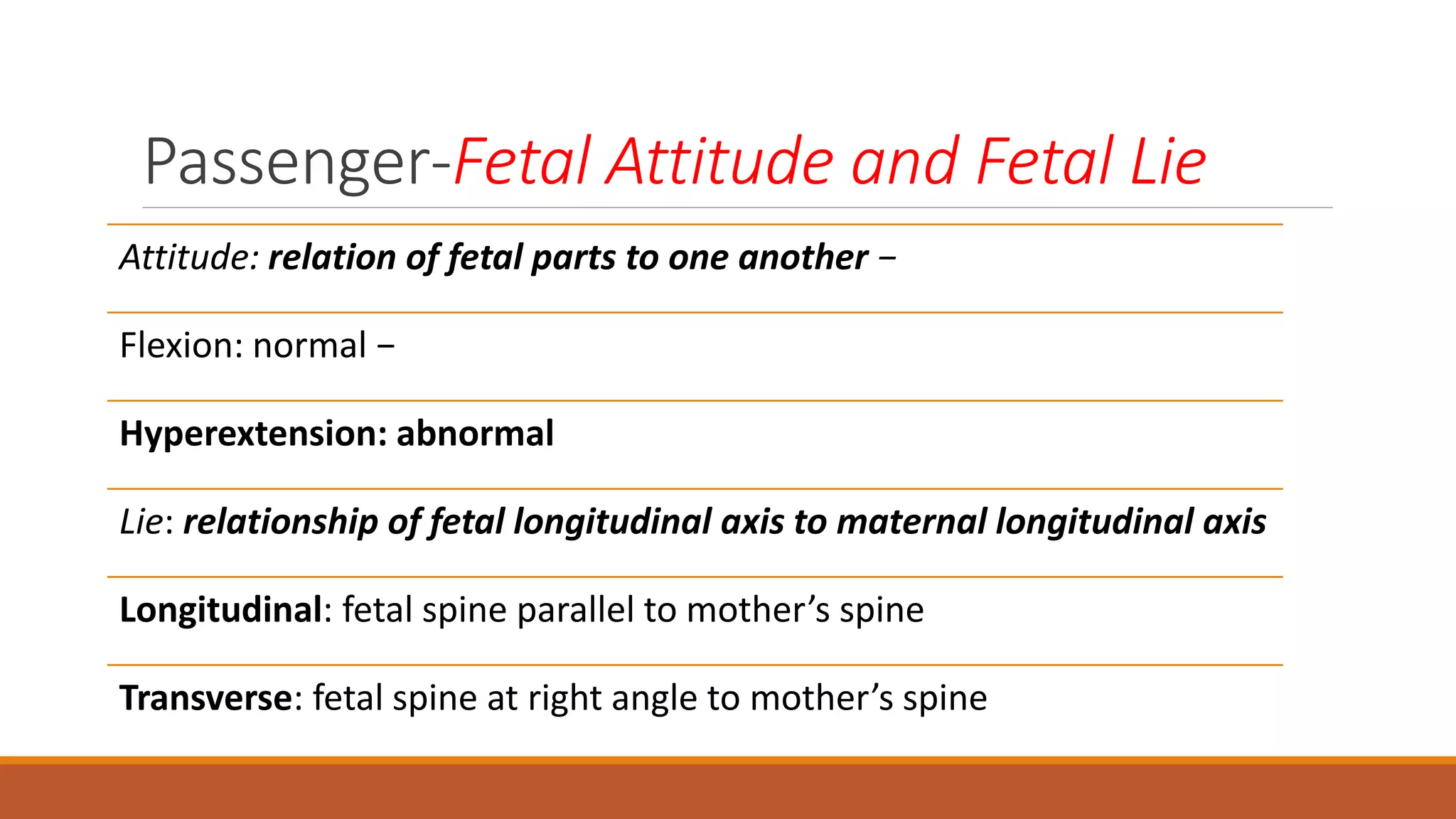
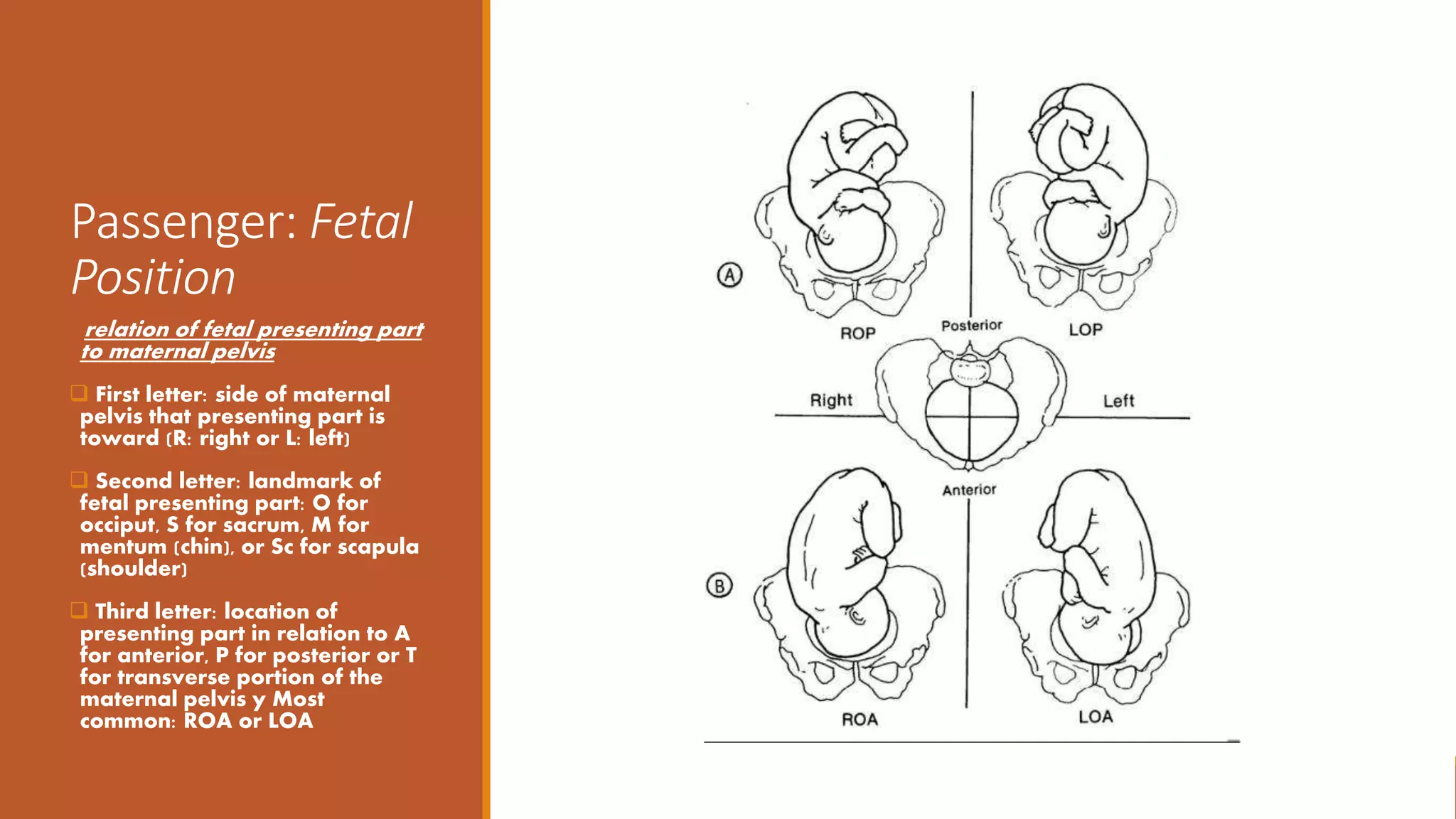
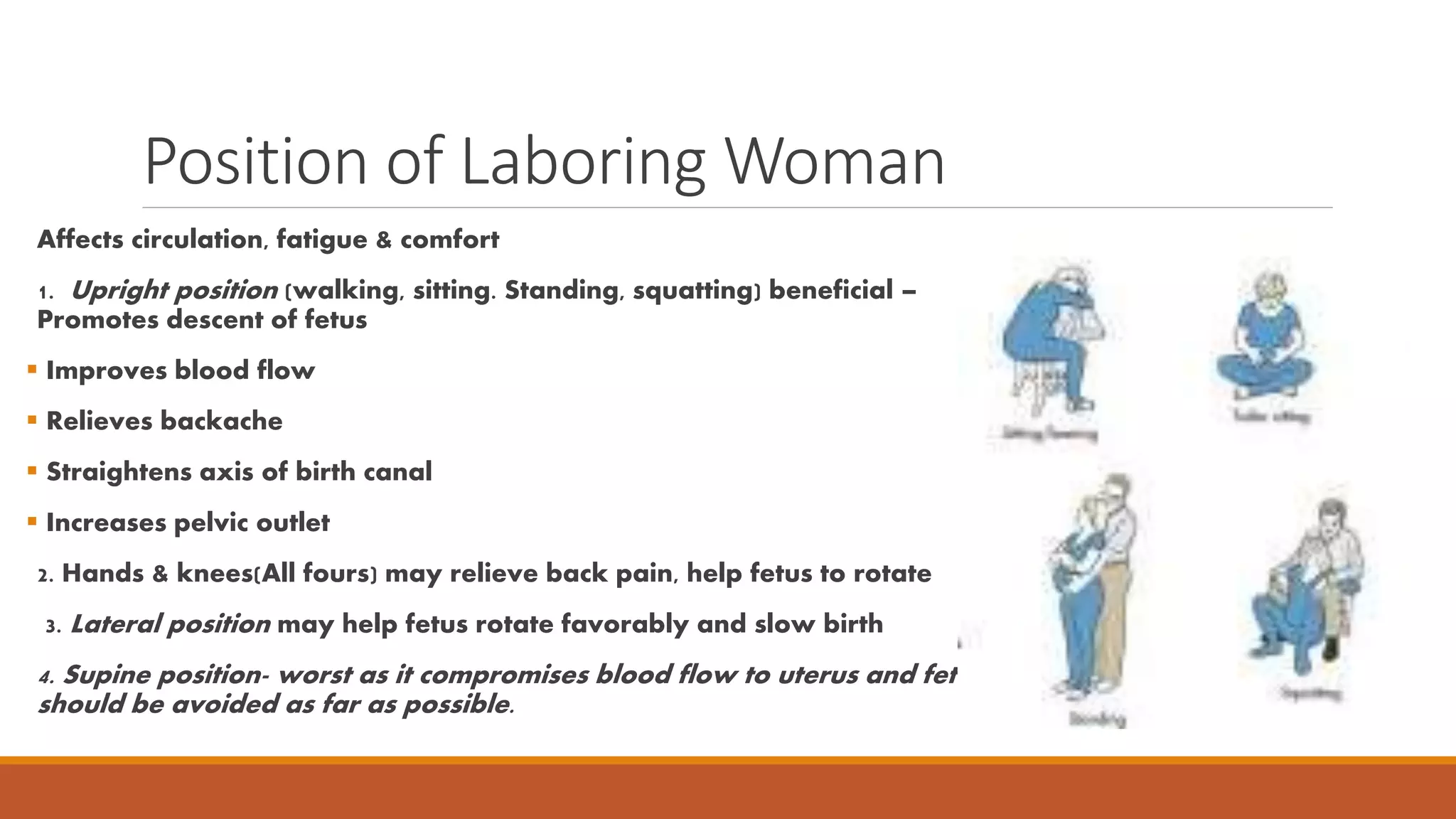
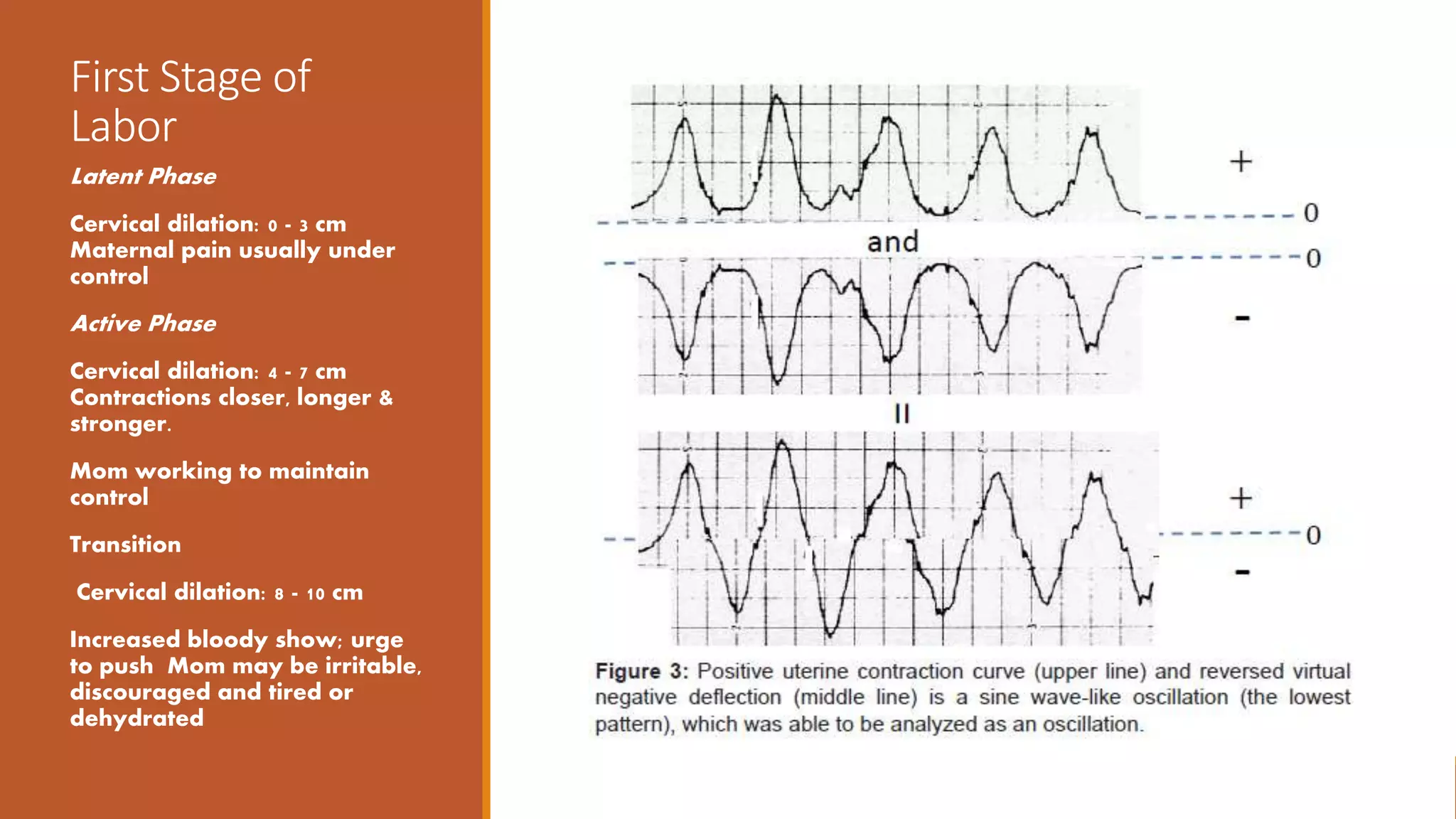
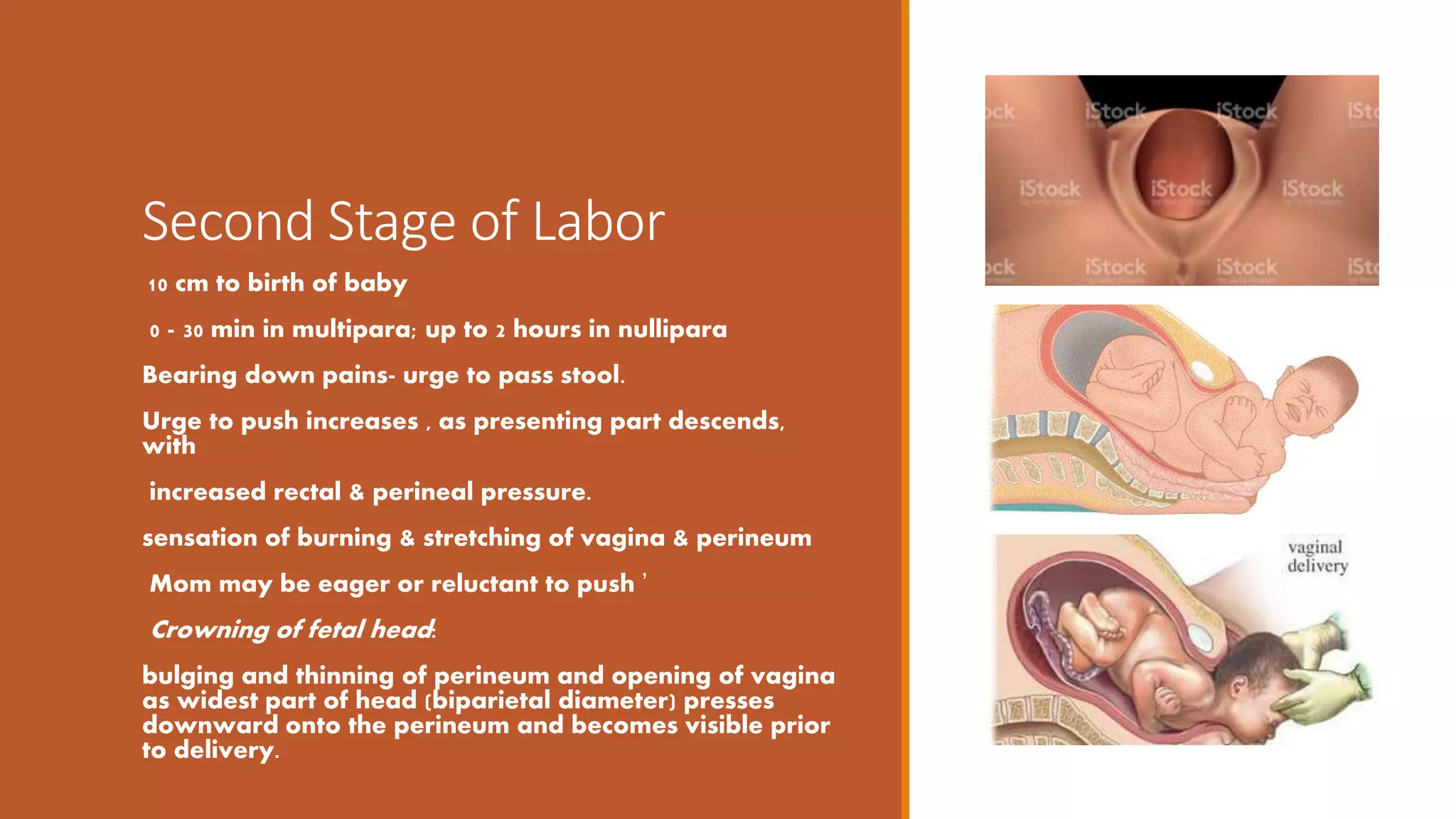
This document discusses the normal labor and birth process. It covers the five Ps of labor (passageway, passenger, powers, position, and psyche), the stages of labor, fetal positioning and engagement, maternal positioning during labor, and pain management techniques. The stages of labor include dilation of the cervix from 0-10 cm in the first stage, delivery of the baby in the second stage, and delivery of the placenta in the third stage. Fetal positioning refers to the fetal lie, presentation, and station. Maternal positioning can help with circulation, fatigue, and comfort during labor. Both non-pharmacologic and pharmacologic techniques are discussed for pain management.