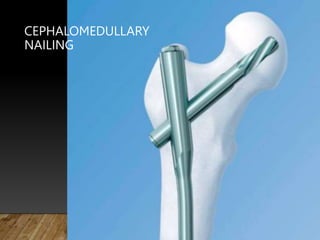
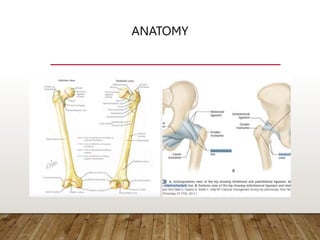
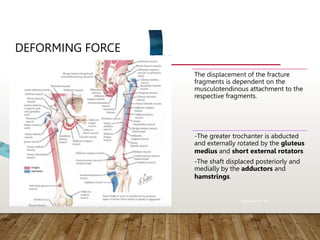
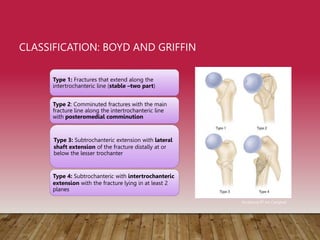
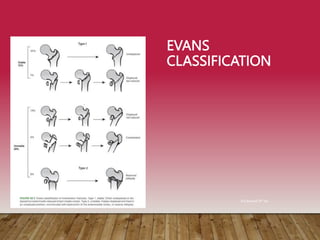
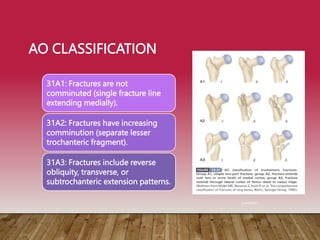
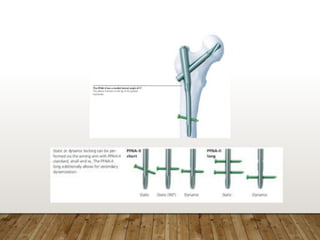
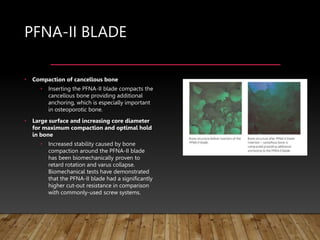
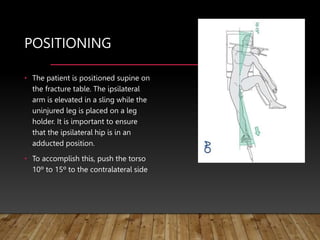
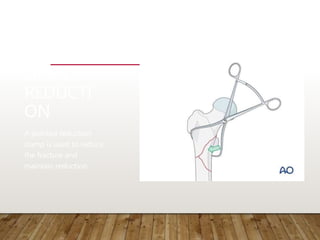
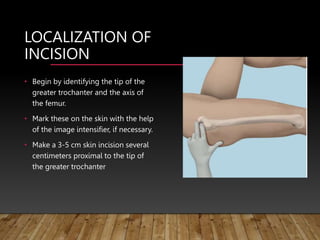
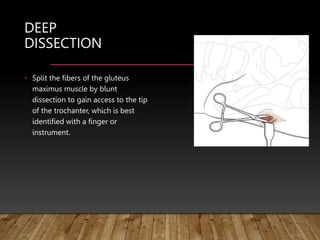
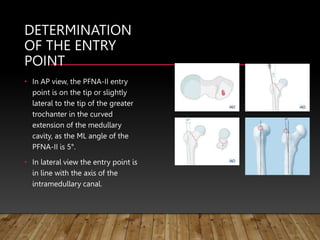
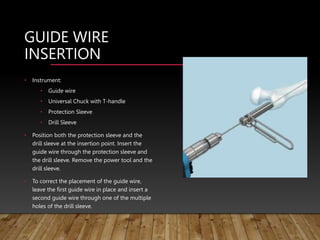
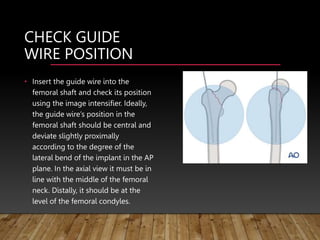
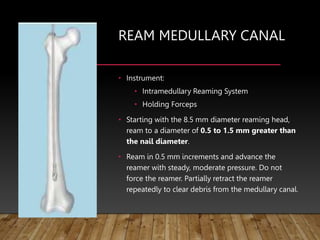
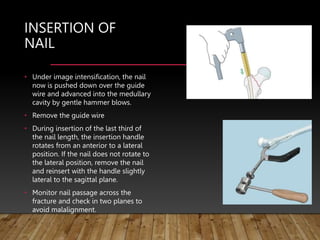
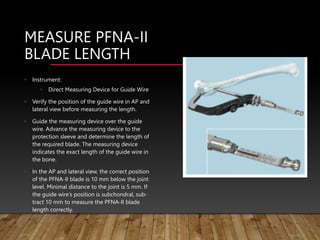
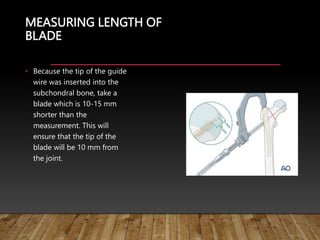
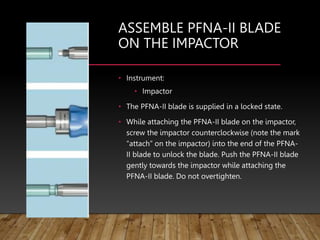
This document provides information on cephalomedullary nailing for hip fractures. It begins with discussing the anatomy and mechanisms of injury for hip fractures. It then covers classification systems for hip fractures, considerations for surgical treatment, and techniques for cephalomedullary nailing. Key steps discussed include preoperative planning, closed or open reduction, determining nail length and diameter, guide wire insertion, reaming the medullary canal, inserting the nail, and performing proximal locking.