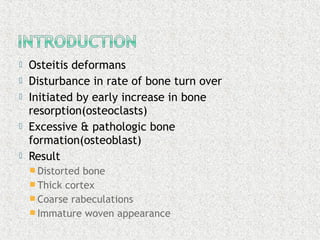
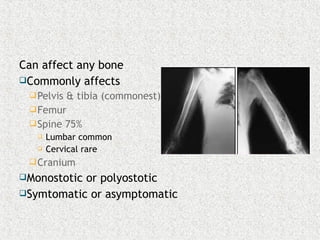
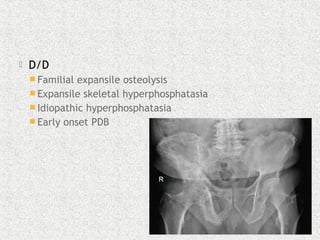
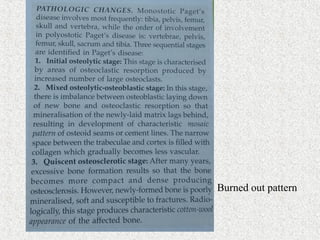
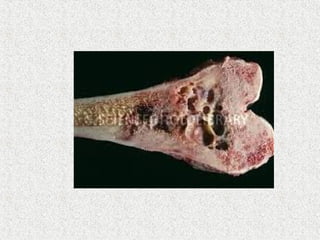
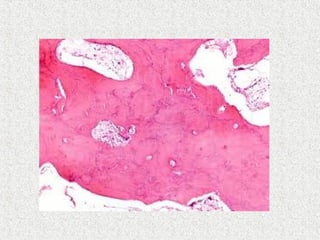
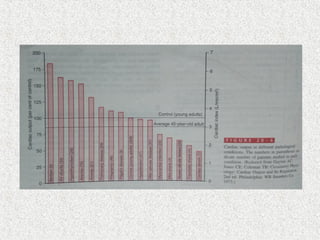
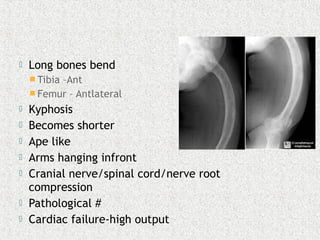
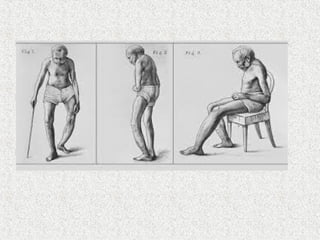
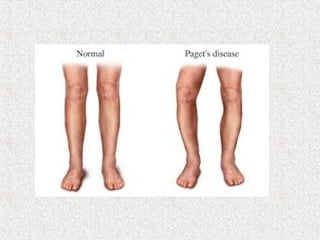
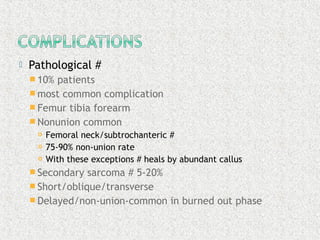
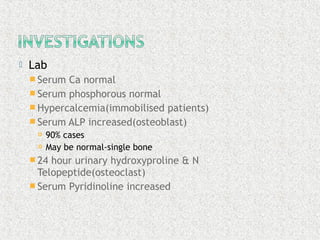
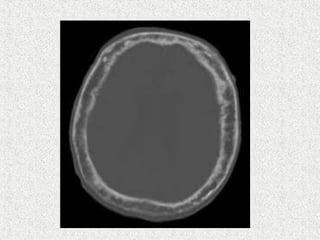
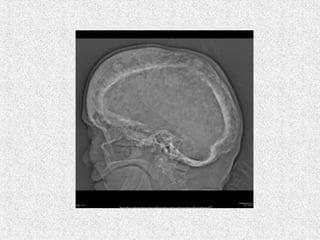
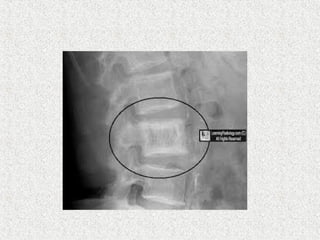
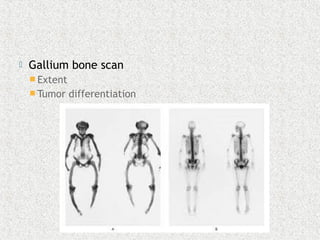
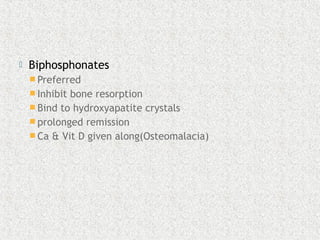
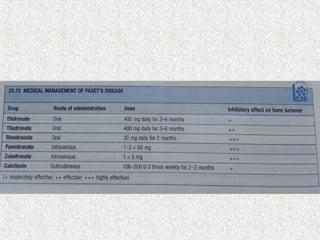
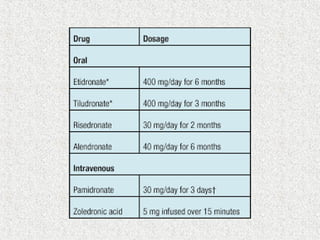
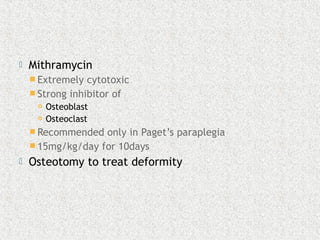
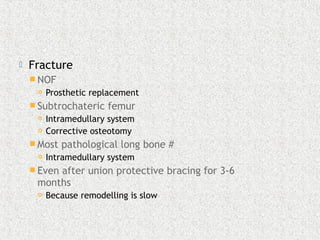
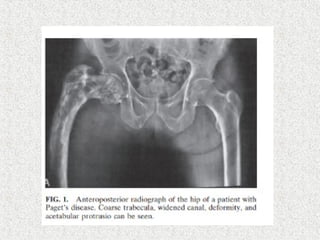
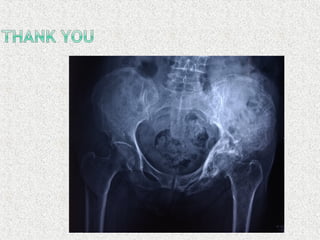
Osteitis deformans, also known as Paget's disease of bone, is a chronic bone disorder characterized by increased and irregular bone remodeling. It results in thickened and misshapen bones with weakened structural integrity. The cause is unknown but may be related to viral infection or genetic factors. It typically affects people over 50 years of age and involves bones of the pelvis, femur, spine and skull. Symptoms range from bone pain, deformities, fractures to neurological complications. Diagnosis is confirmed by x-ray findings and elevated bone turnover markers. Treatment focuses on reducing bone turnover with bisphosphonates or calcitonin to relieve symptoms and prevent complications like fractures.