This document provides information on tuberculosis (TB) including:
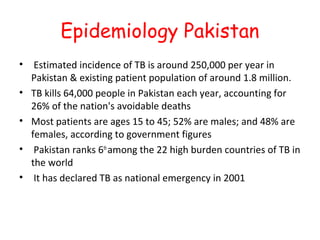
1. TB epidemiology statistics for Pakistan which has a high burden of TB with an estimated 250,000 new cases and 64,000 deaths per year.
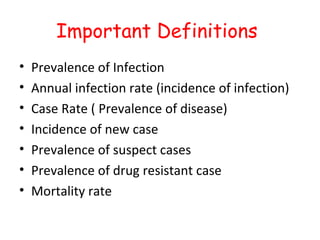
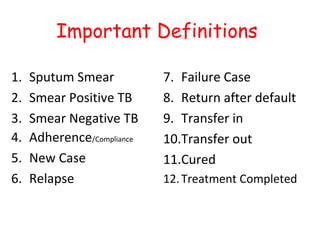
2. Definitions of key TB terms such as prevalence, incidence, drug resistant cases, and treatment outcomes.
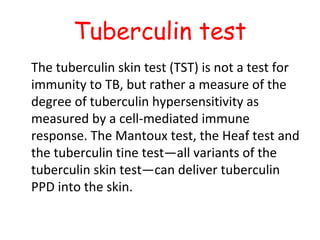
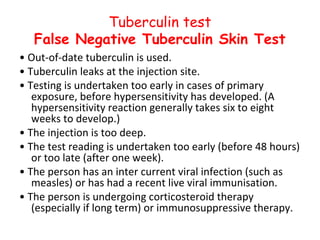
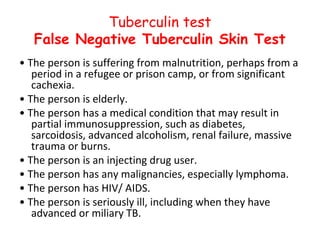
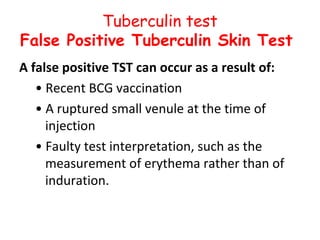
3. Descriptions of diagnostic tests for TB including the tuberculin skin test and its limitations, as well as the QuantiFERON blood test.
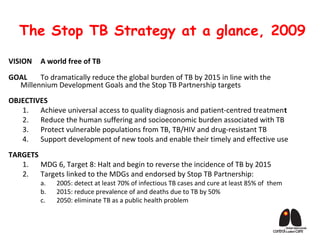
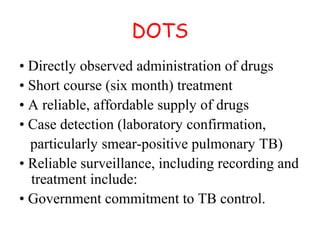
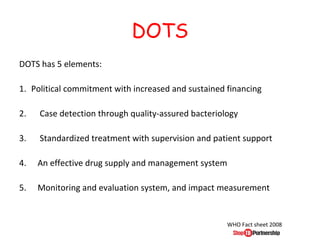
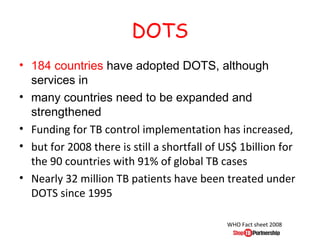
4. Overviews of the WHO recommended DOTS strategy for TB control, which involves direct observation of treatment, and the five elements of effective TB programs.