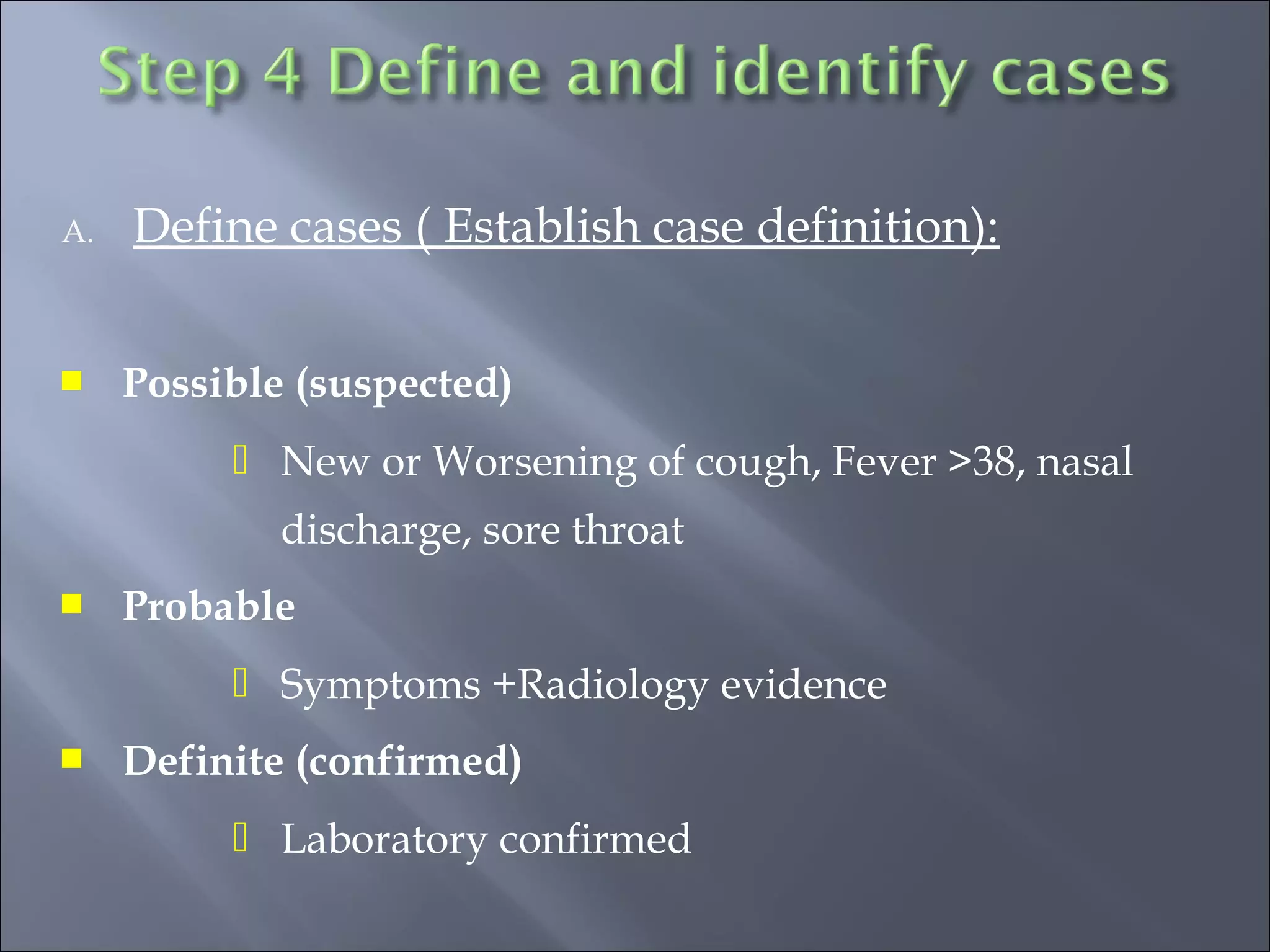
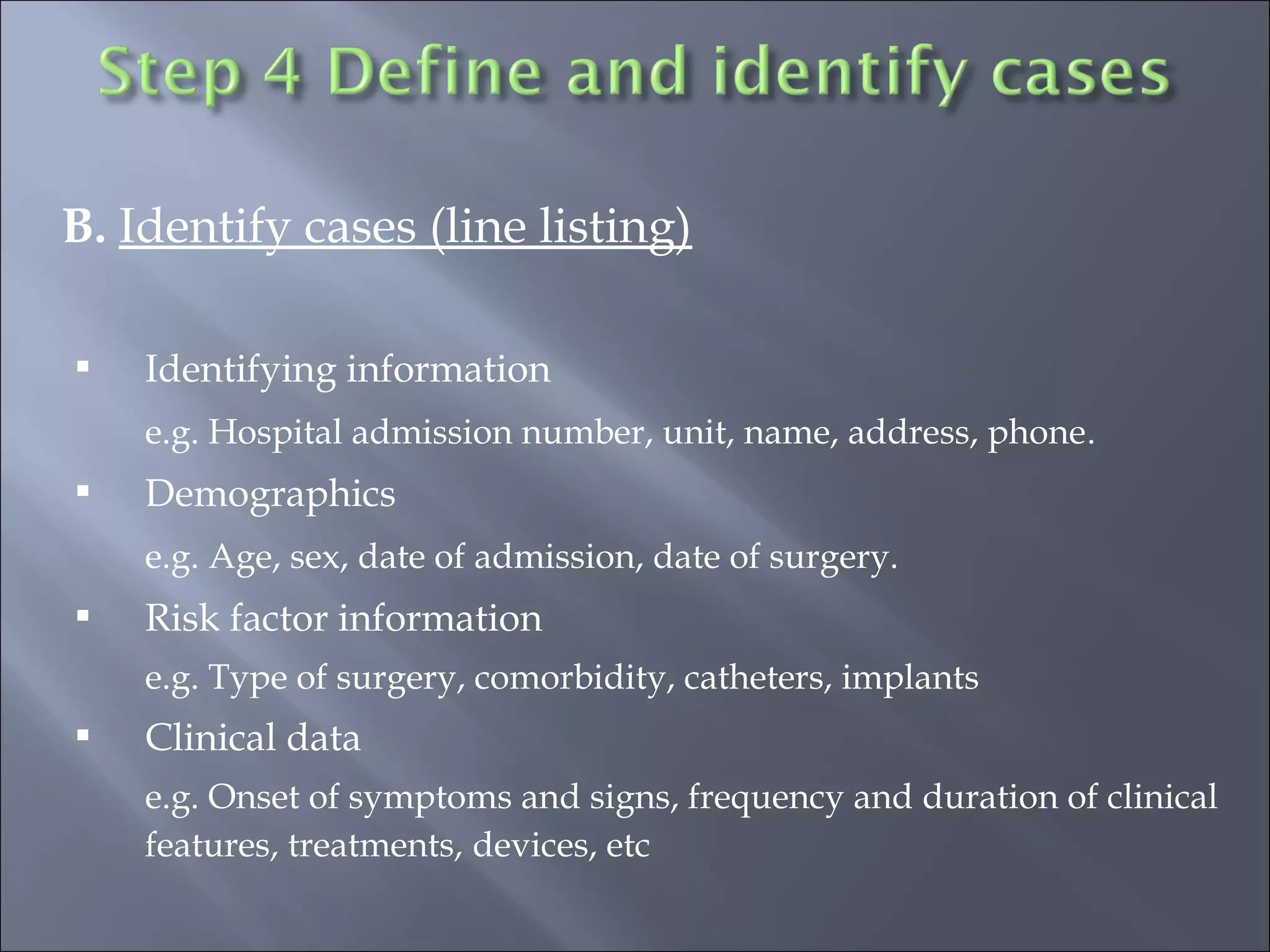
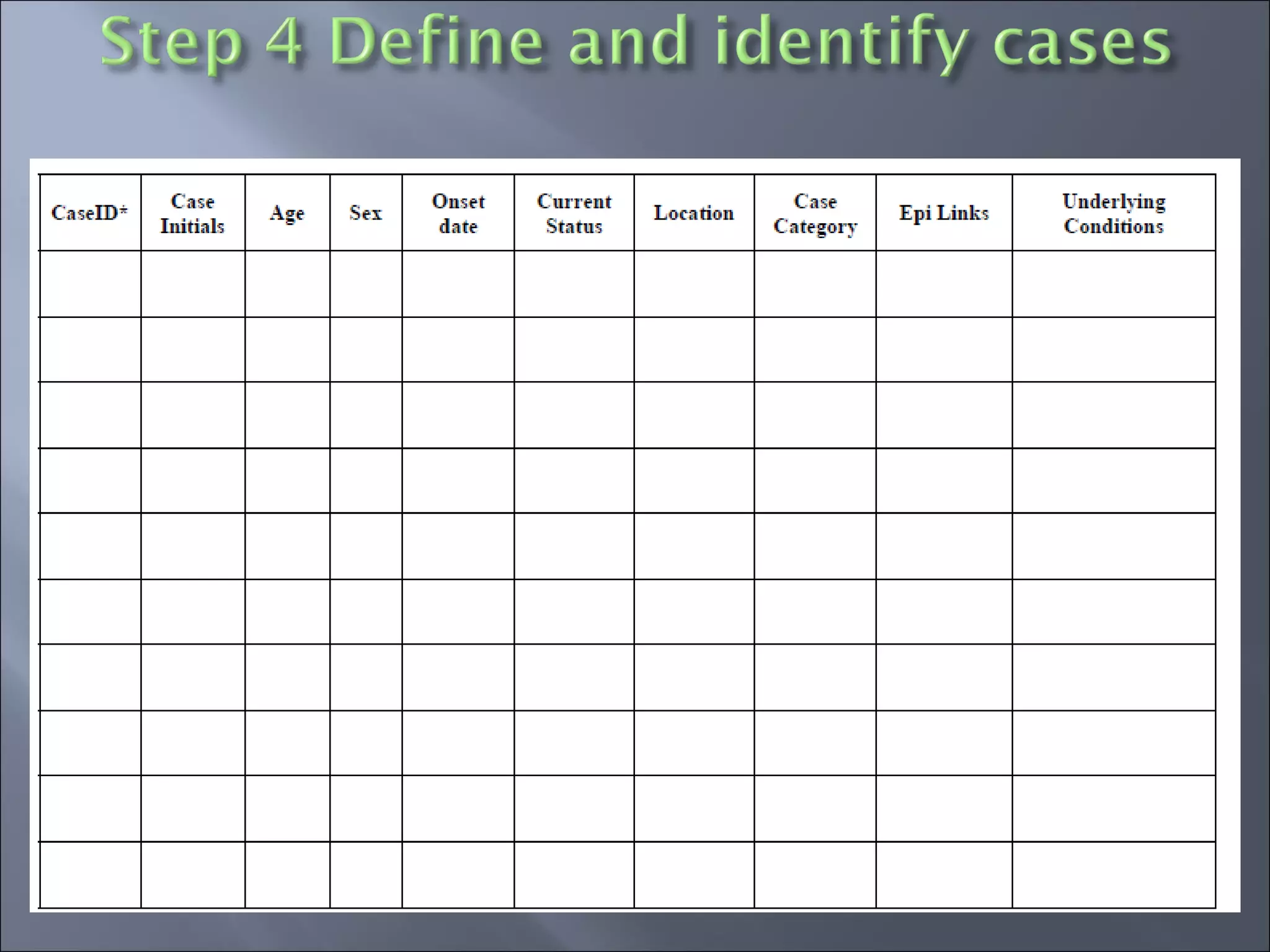
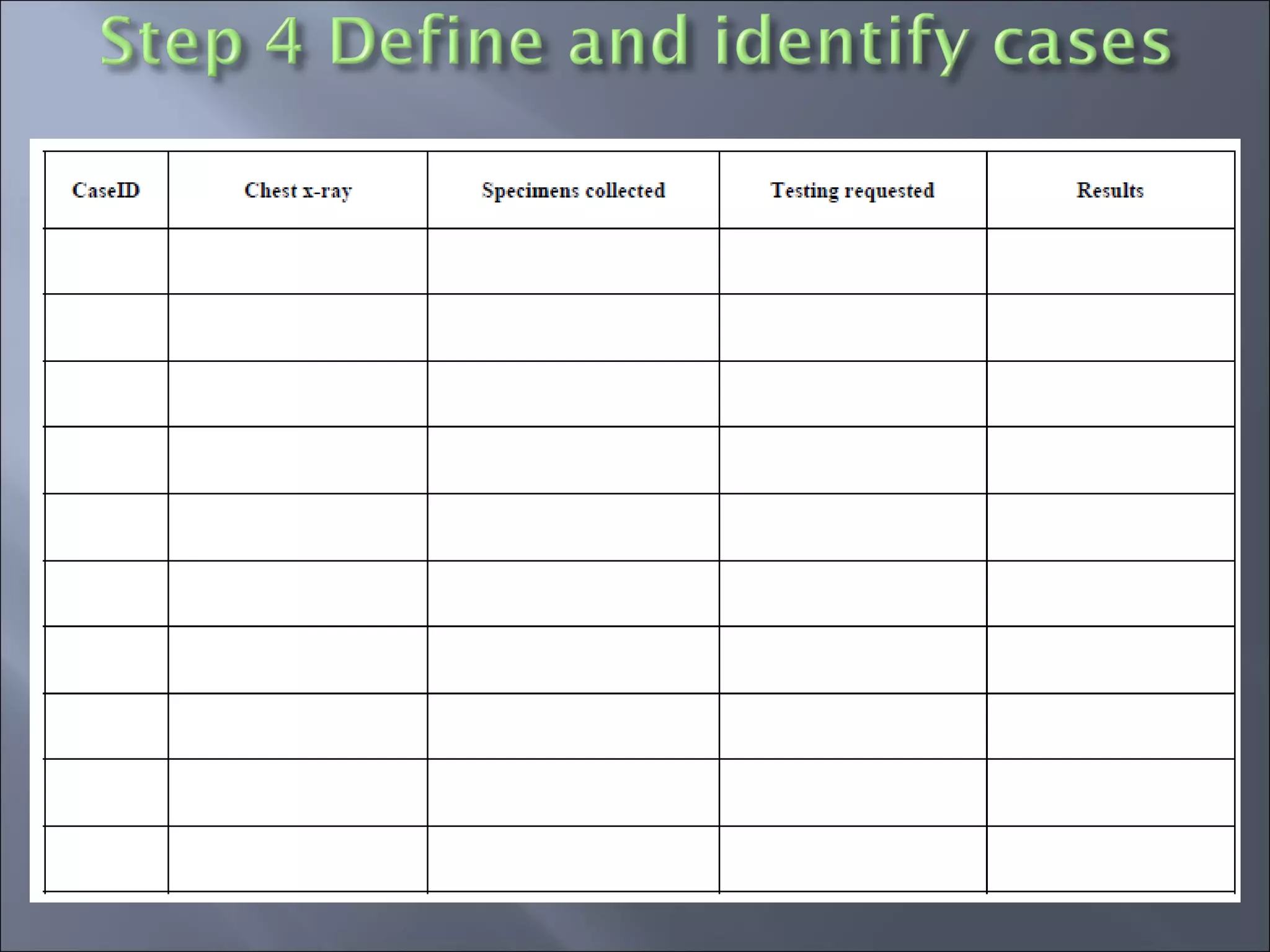
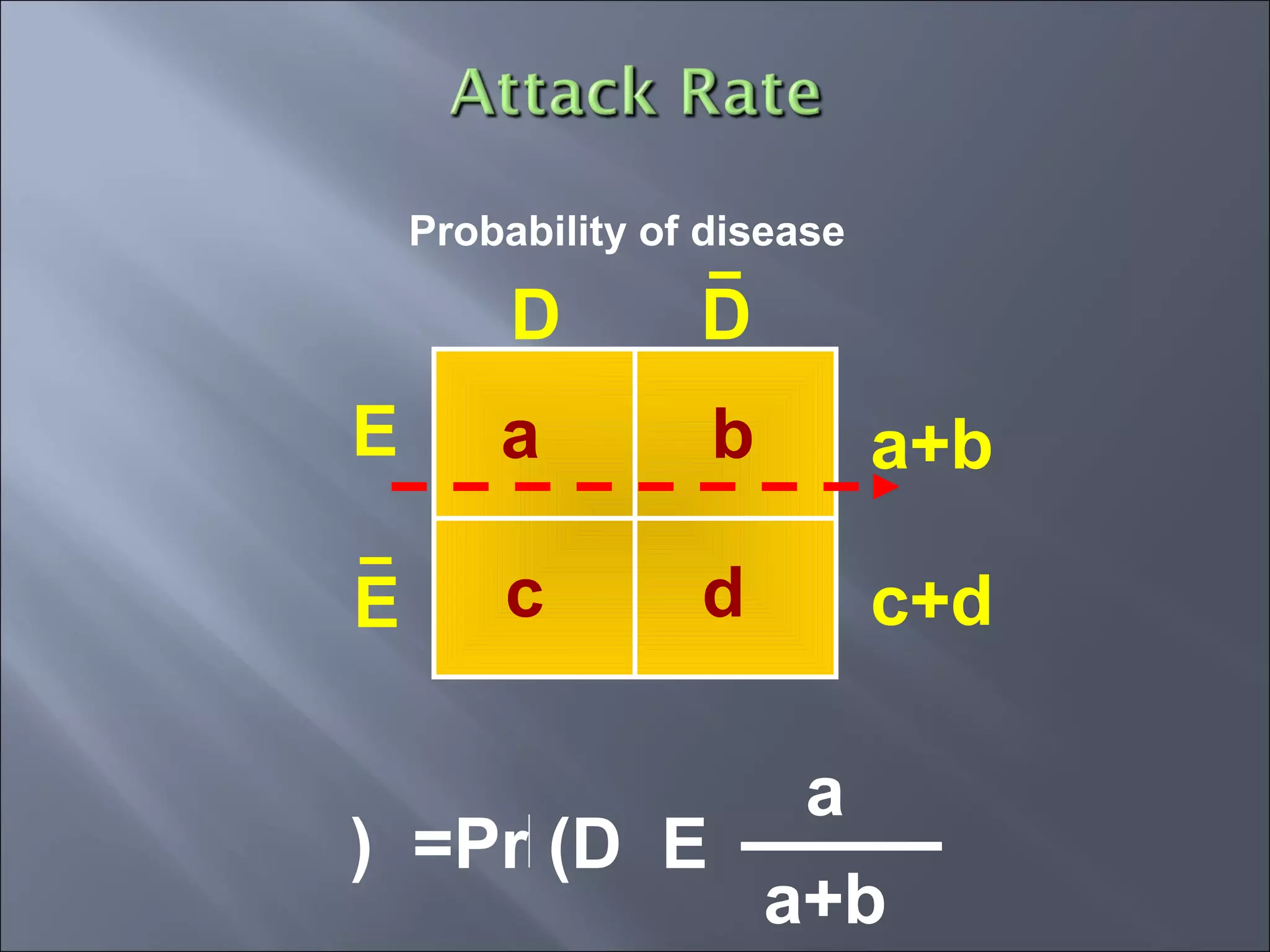
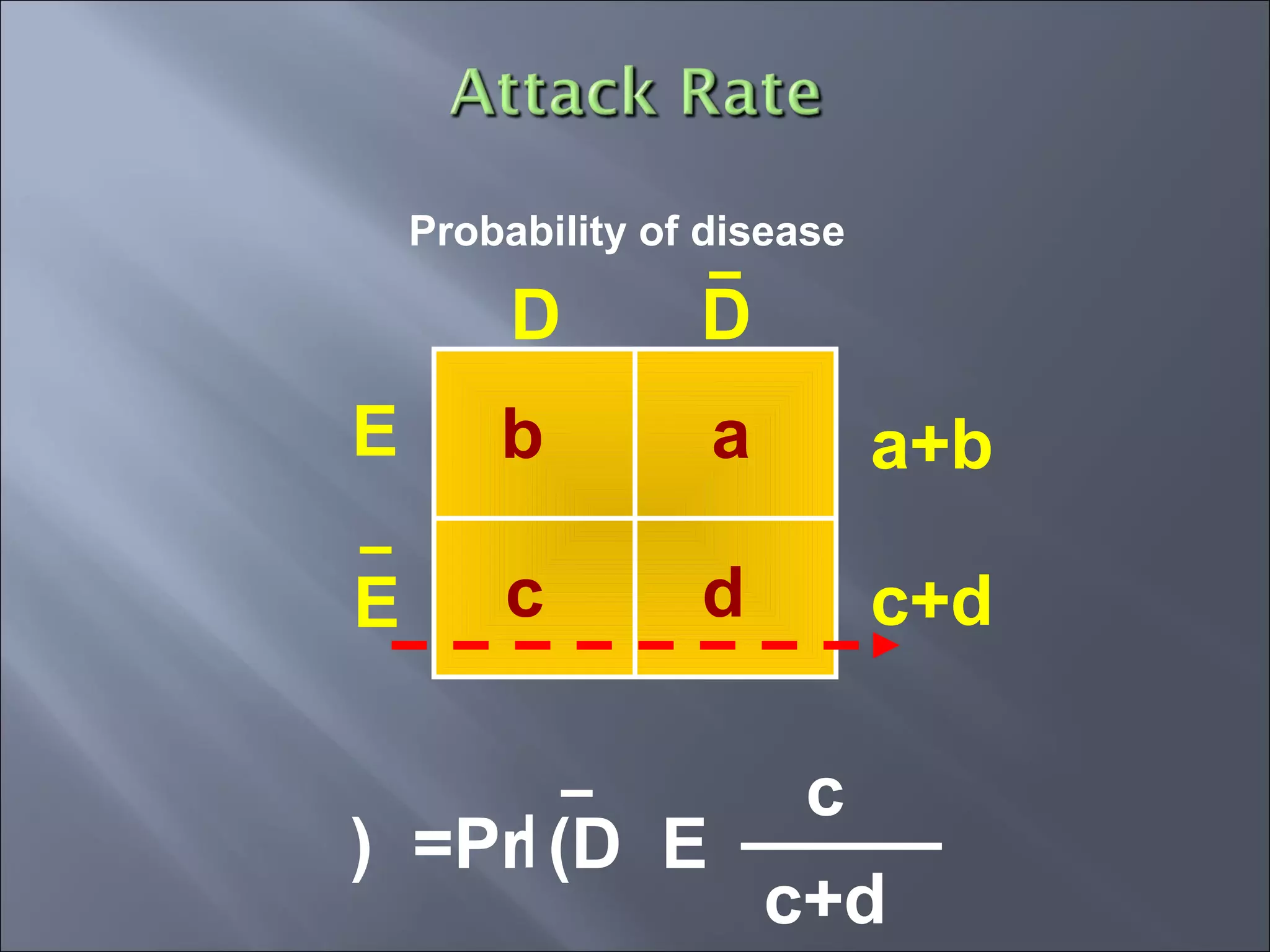
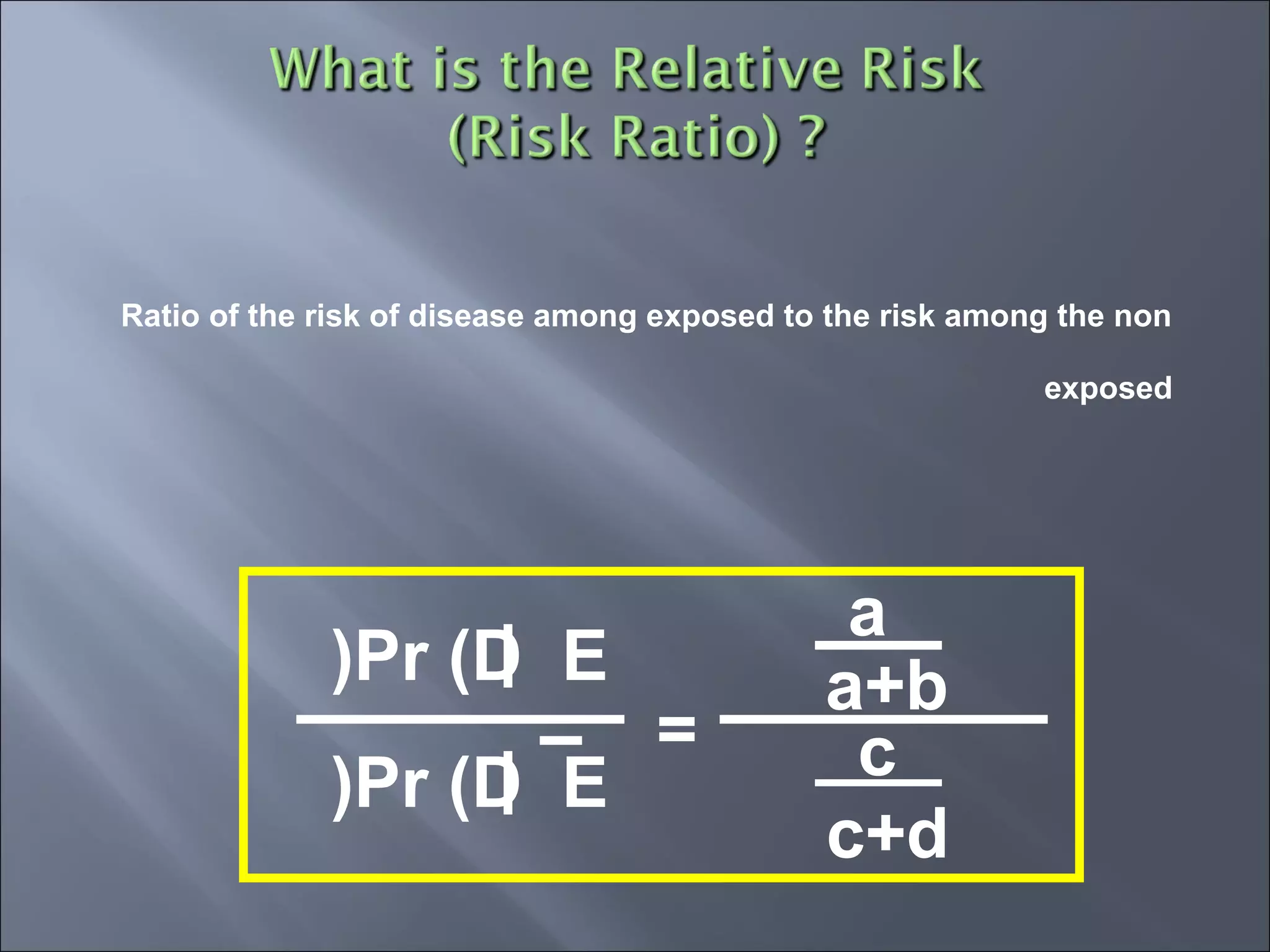
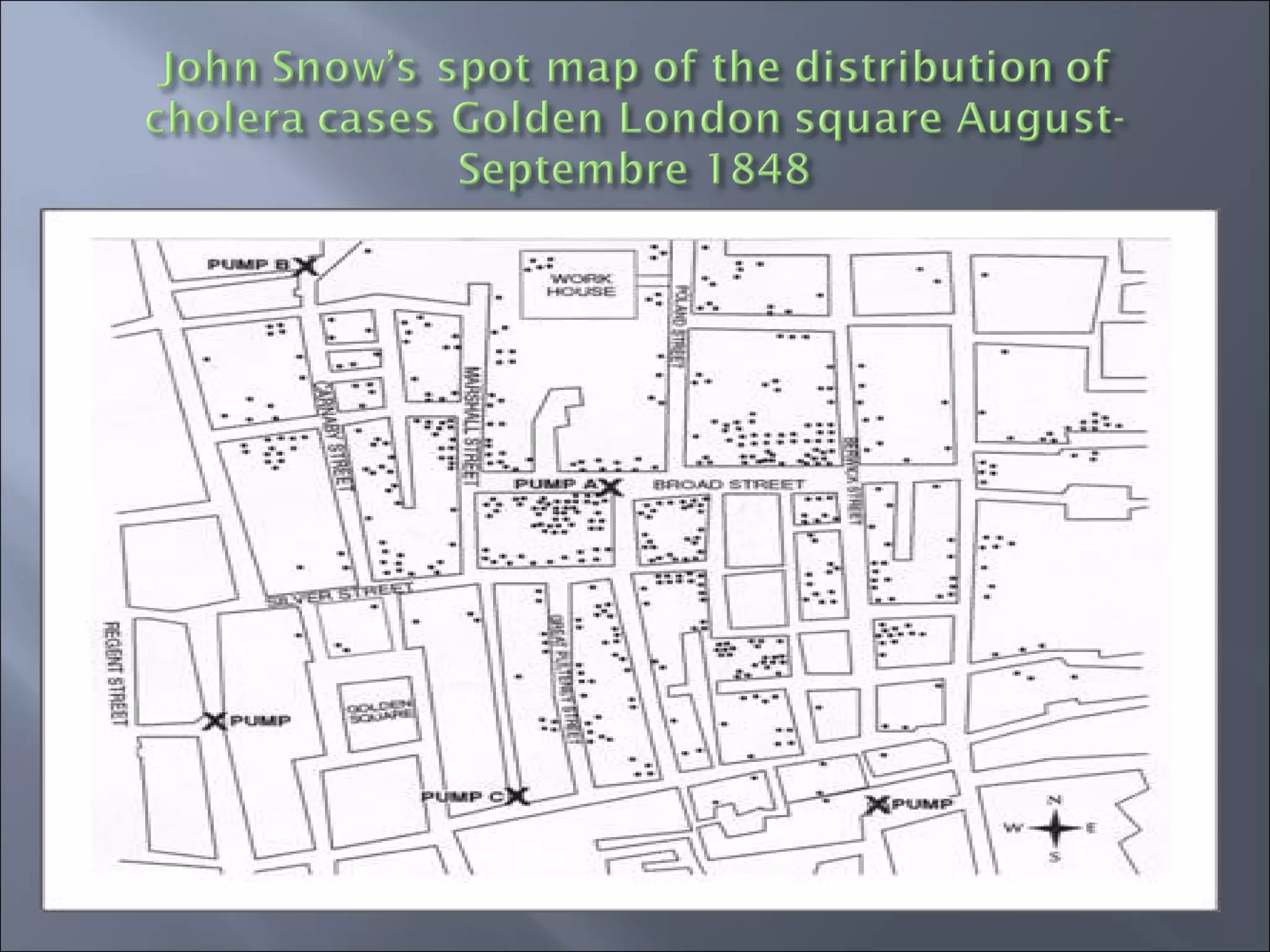
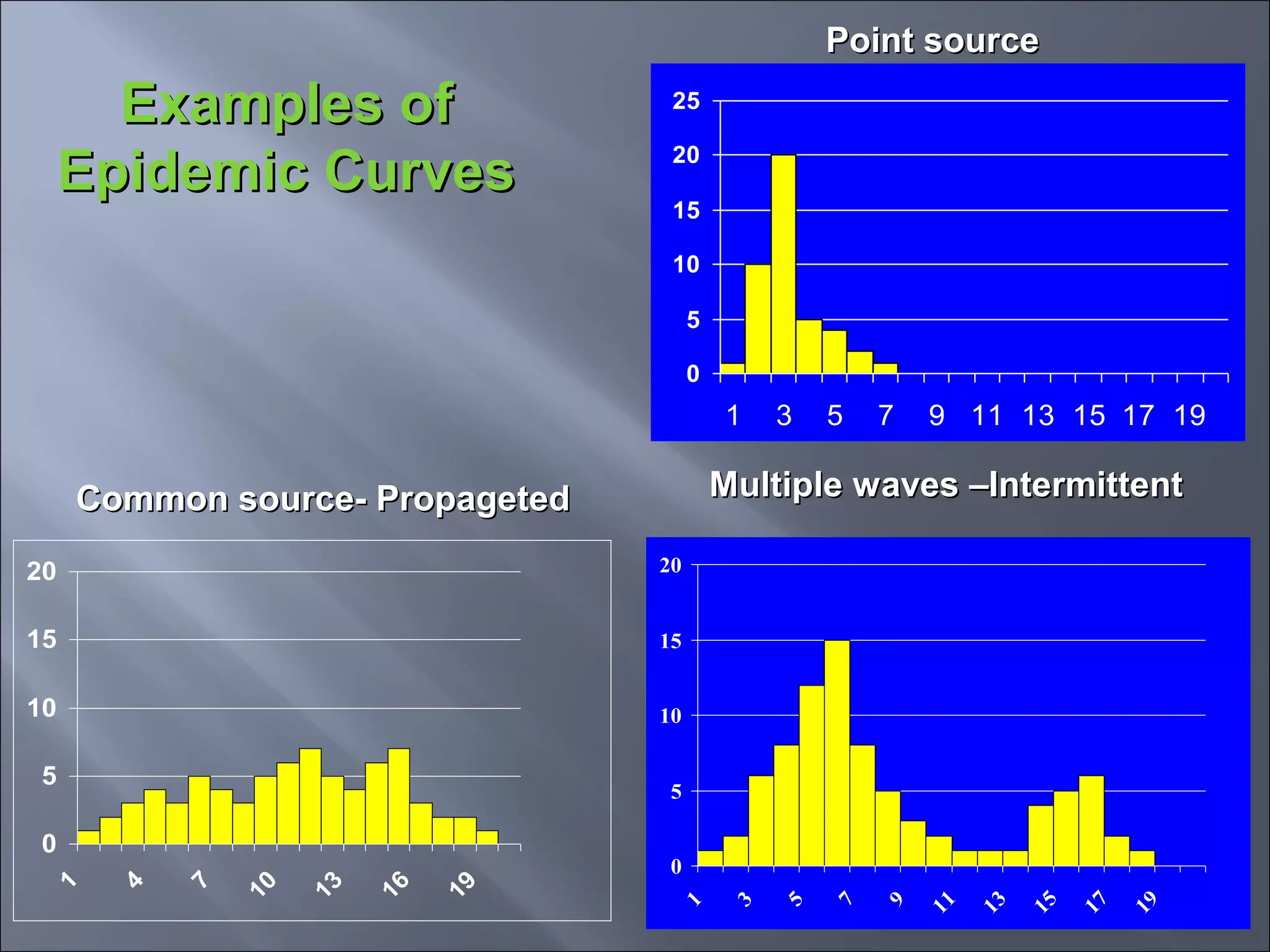
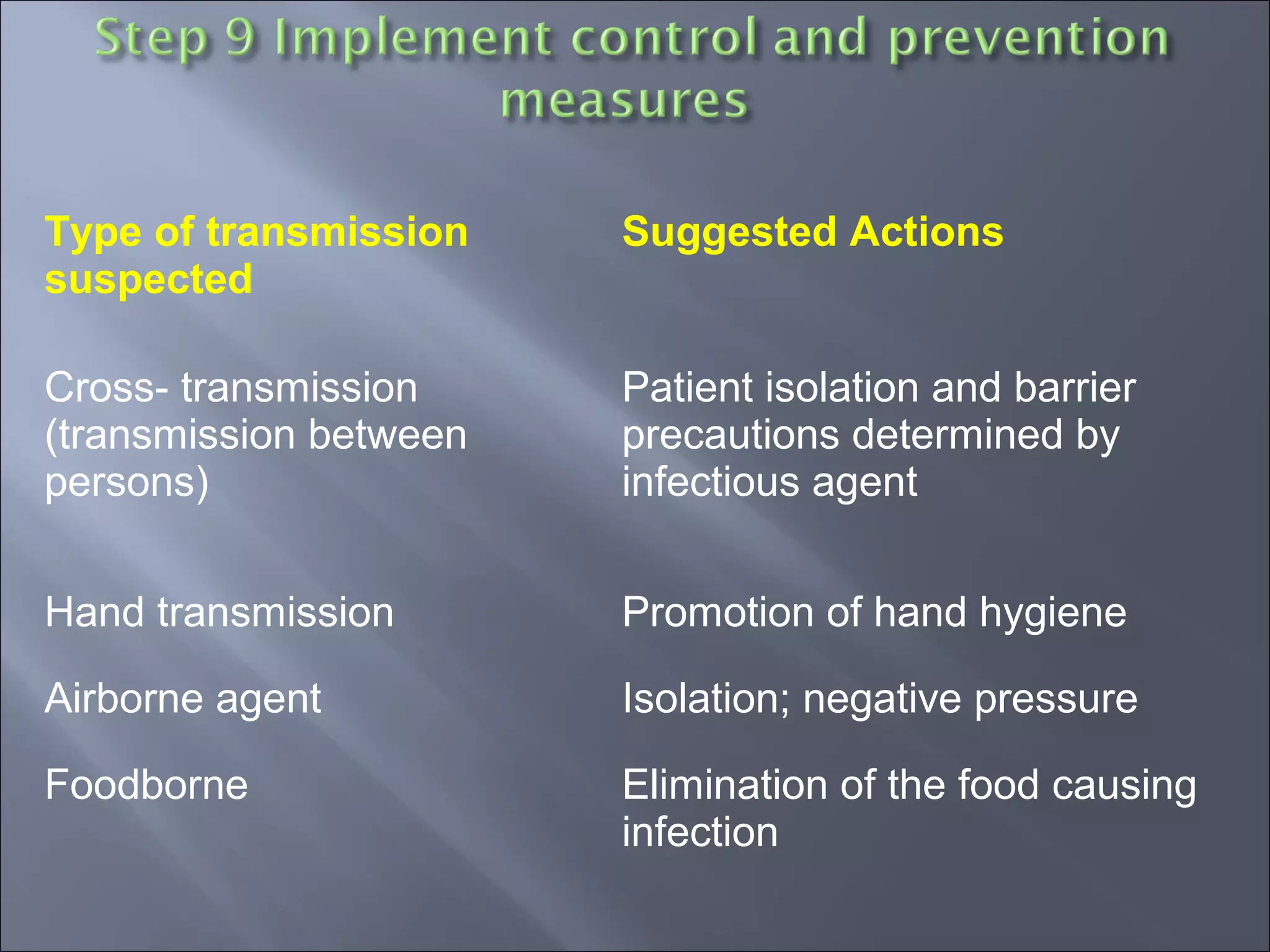
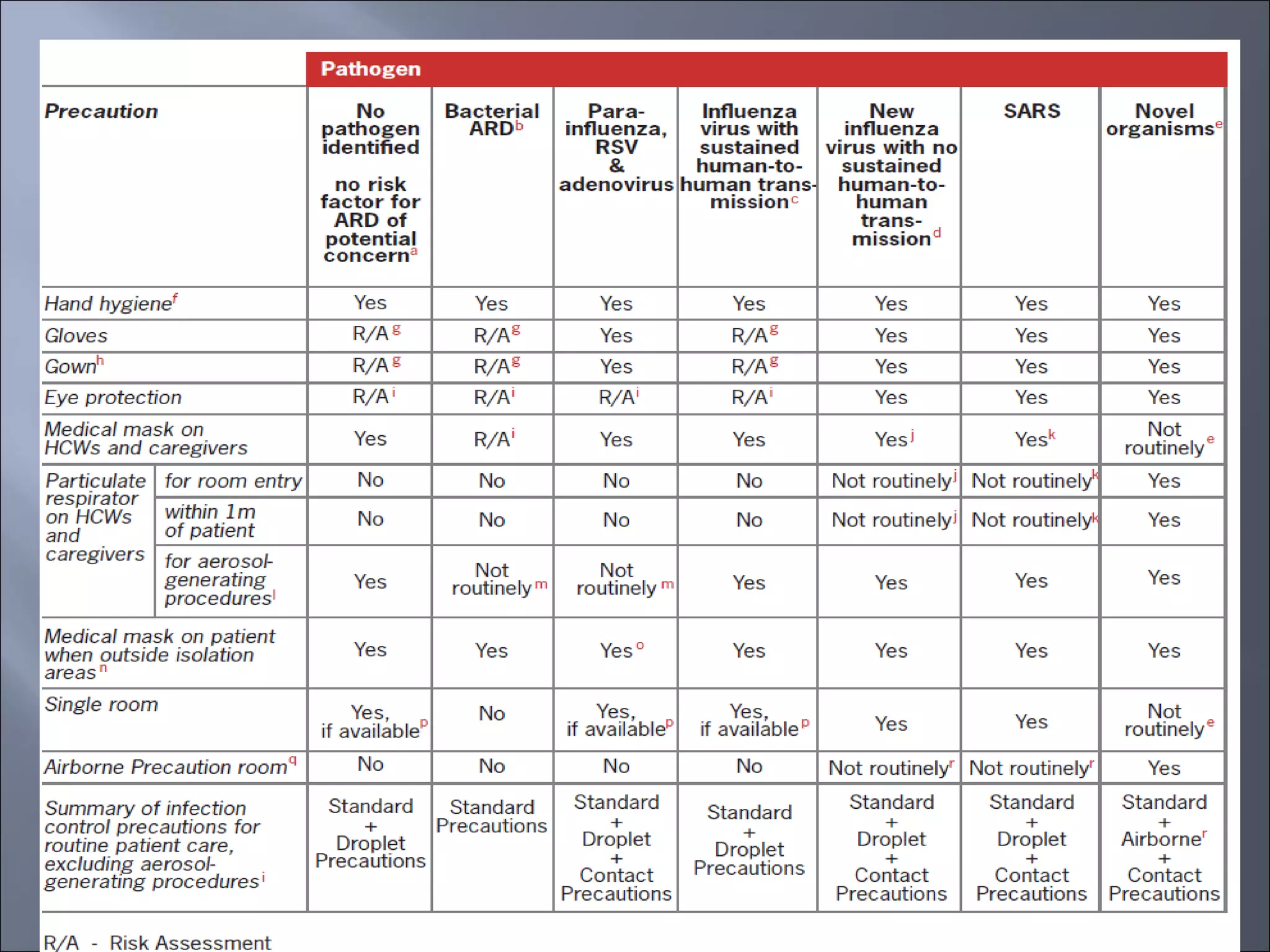
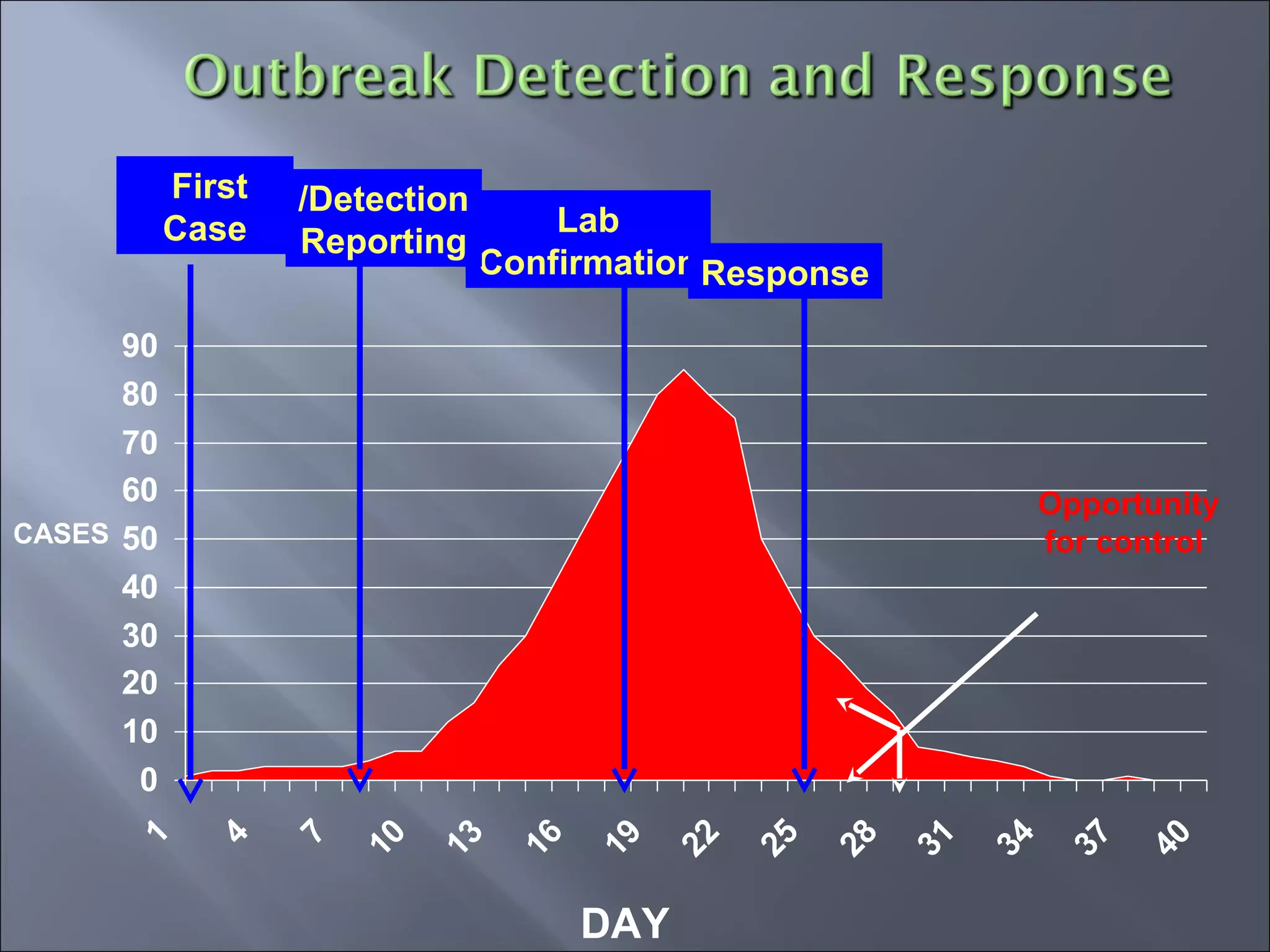
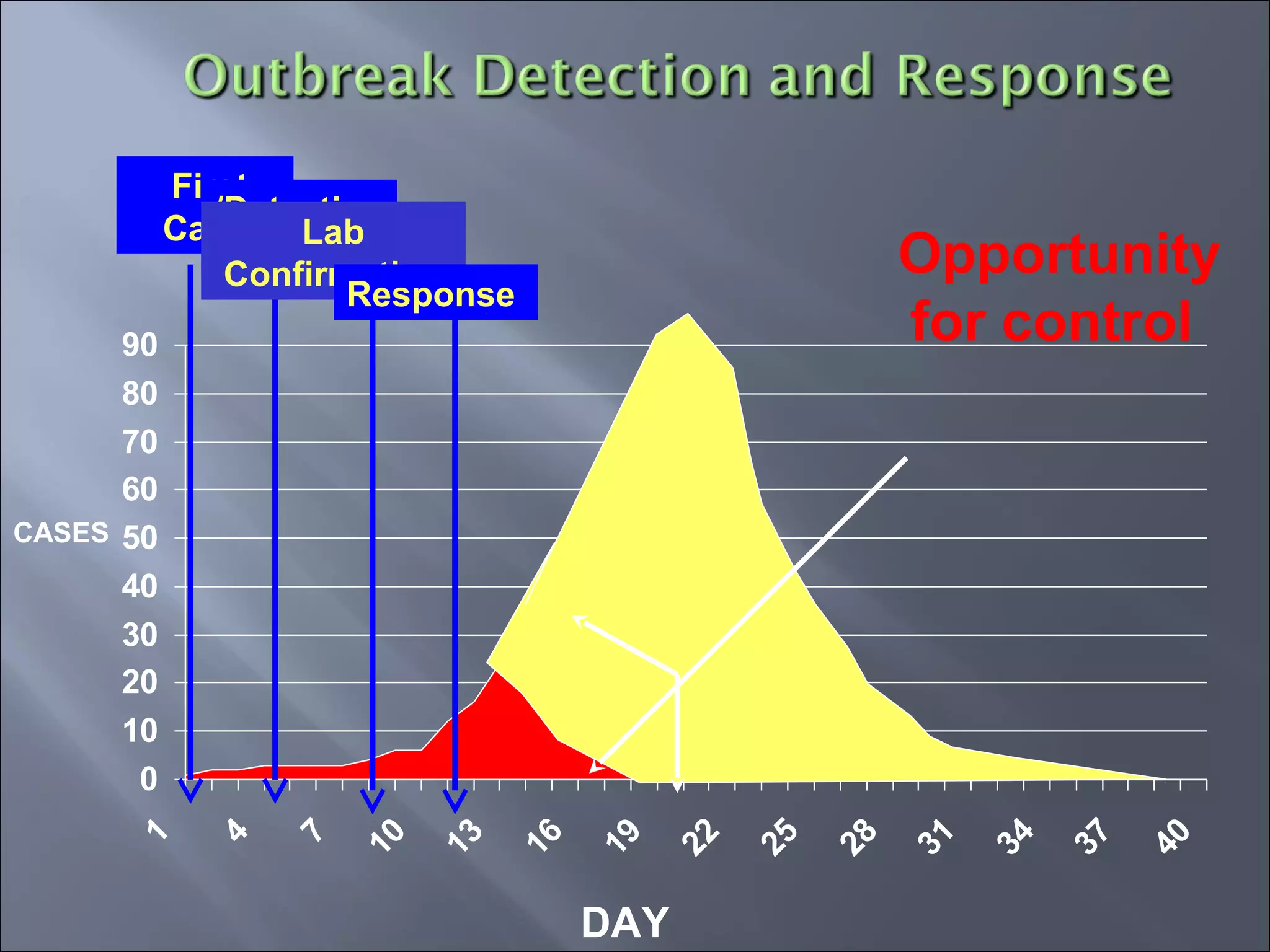
This document discusses healthcare-associated infections (HAIs) and outbreak investigations. It defines key terms like clusters, outbreaks, and epidemics. It also outlines the reasons to investigate outbreaks, how to recognize them, and the goals and steps of investigations. The steps include defining cases, identifying cases, analyzing person, place and time factors, developing and evaluating hypotheses, implementing controls, and communicating findings. The overall purpose is to identify the cause of the outbreak and implement measures to control it.