This document discusses syncope (fainting), including:
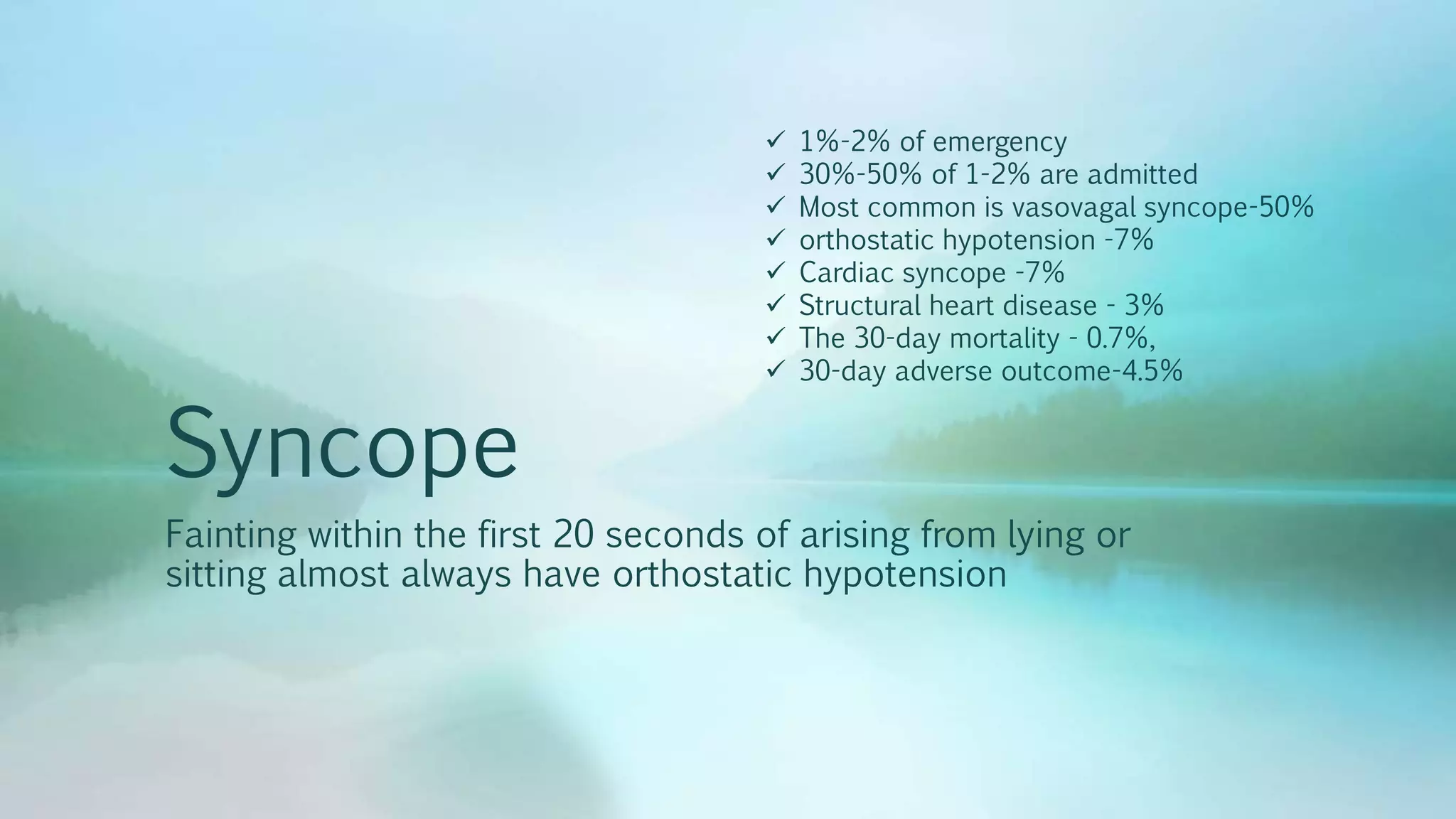
- Causes of syncope include vasovagal (50%), orthostatic hypotension (7%), and cardiac causes (7%).
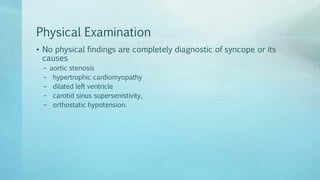
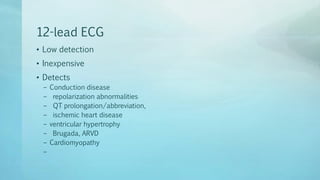
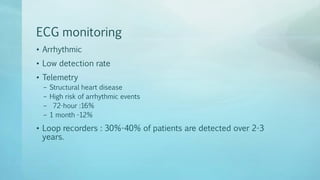
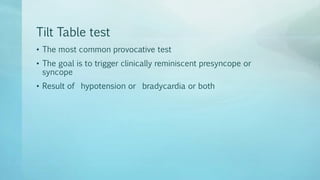
- Tests for syncope include ECG, echocardiogram, extended ECG monitoring, and tilt table testing. However, a good history is usually most useful and accurate.
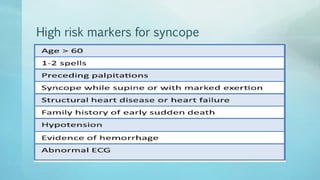
- Risk of adverse outcomes from syncope within 30 days includes mortality of 0.7% and other outcomes in 4.5% of patients. Structural heart disease is a risk factor.