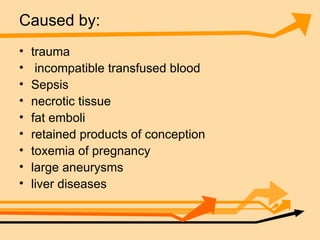
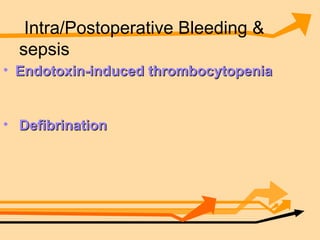
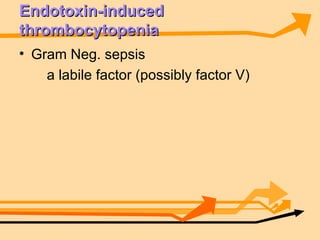
1. Excessive bleeding during or after surgery can be caused by ineffective local hemostasis, complications from blood transfusions, pre-existing coagulation disorders, or disseminated intravascular coagulation.
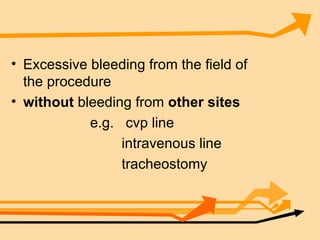
2. Ineffective local hemostasis can result in bleeding only from the surgical site, while other potential causes may lead to diffuse bleeding.
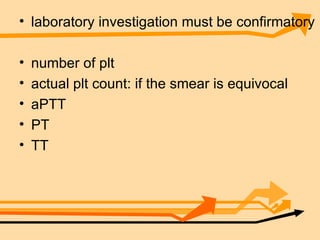
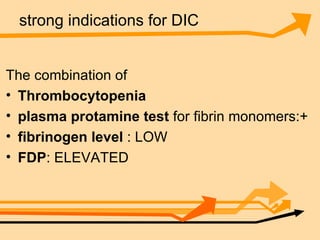
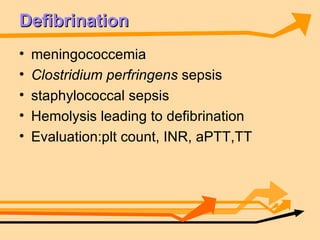
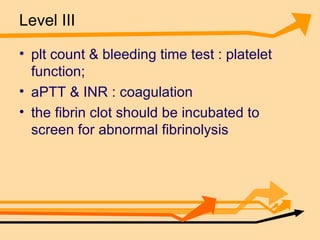
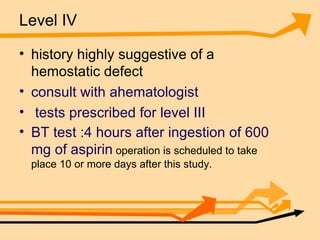
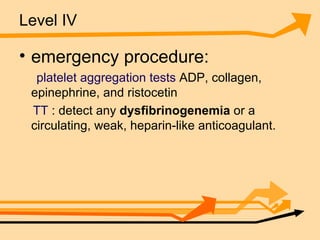
3. Various laboratory tests can help identify the underlying cause, guide treatment decisions, and distinguish between coagulation disorders and fibrinolysis.