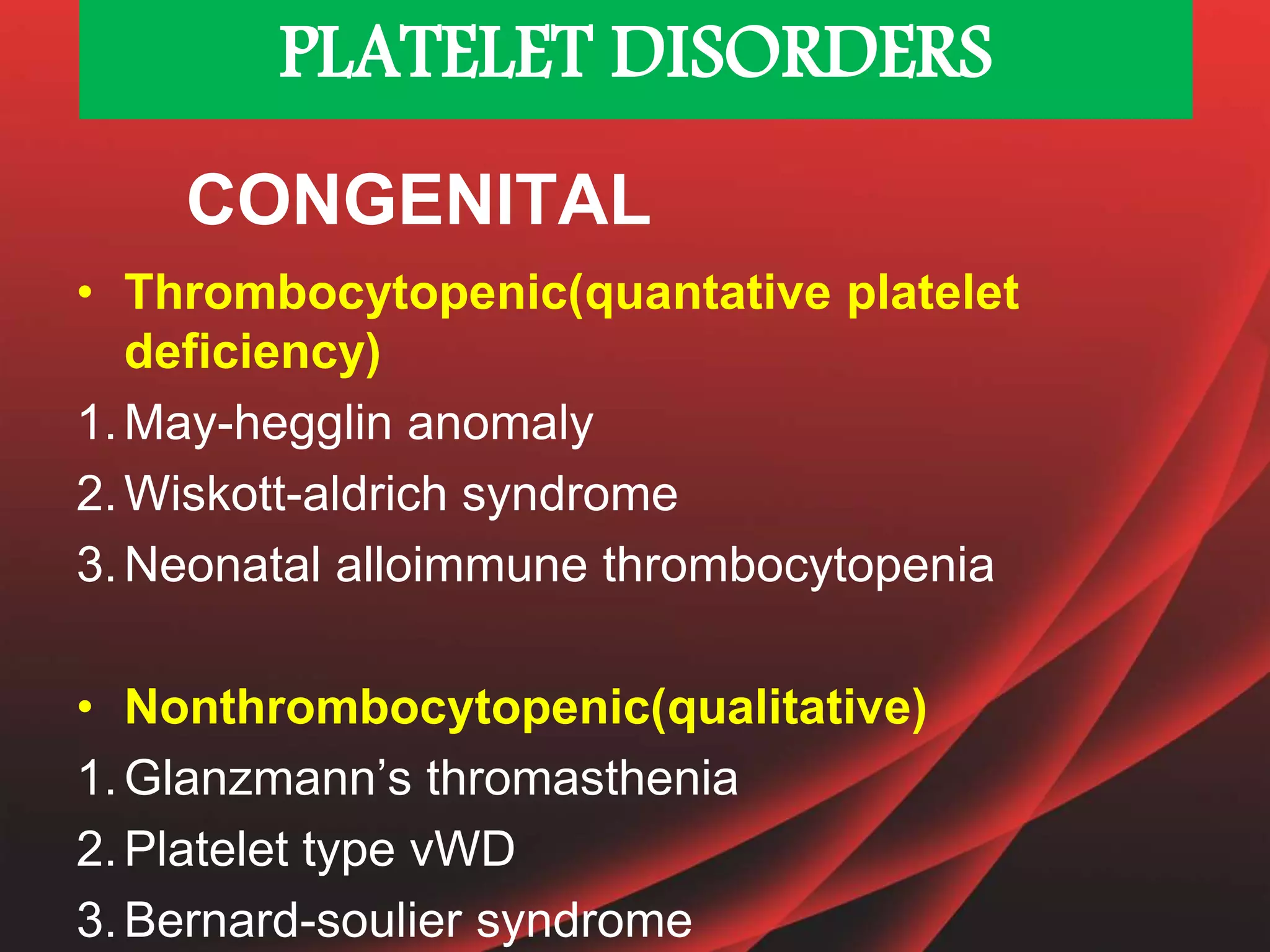
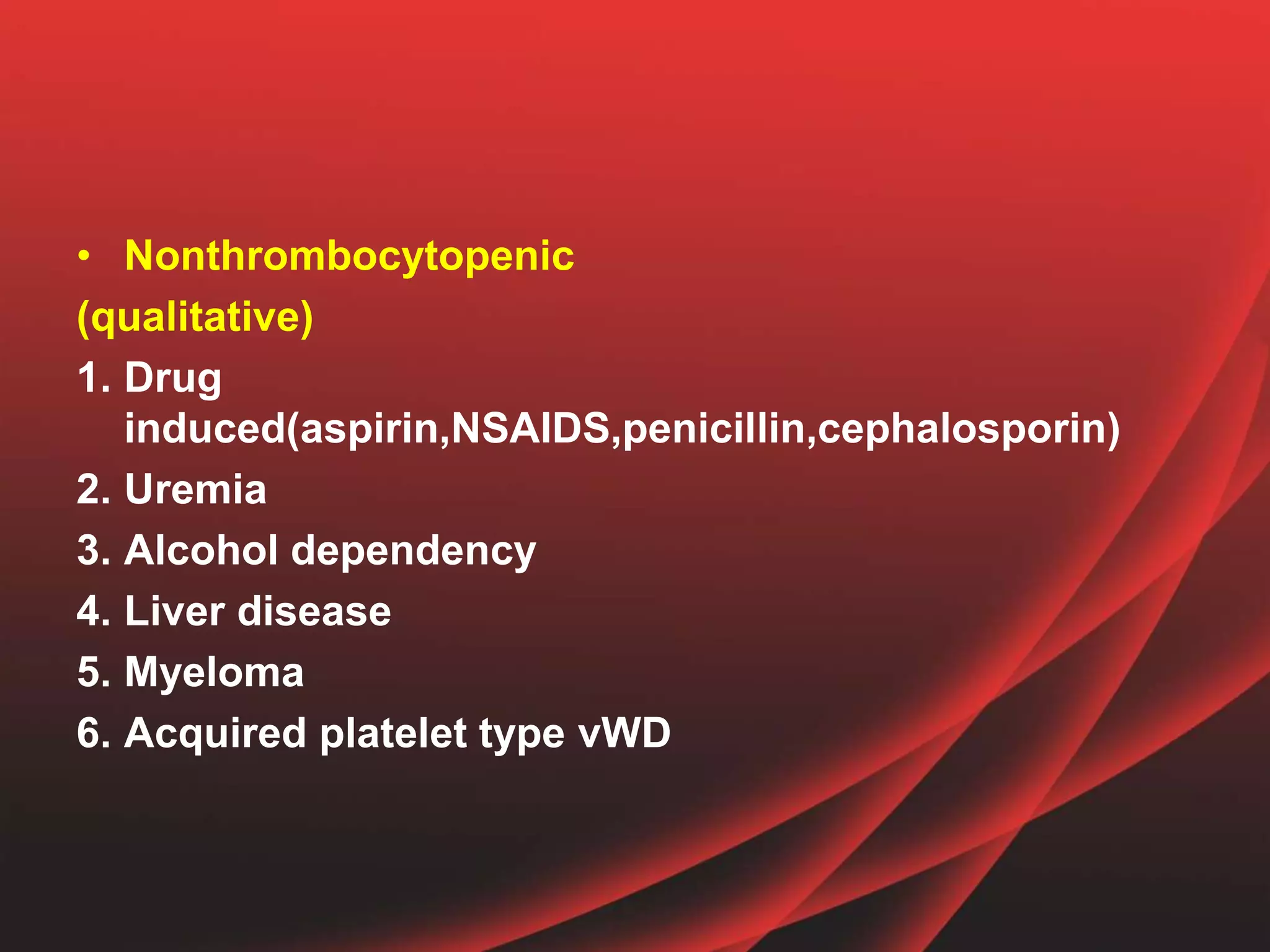
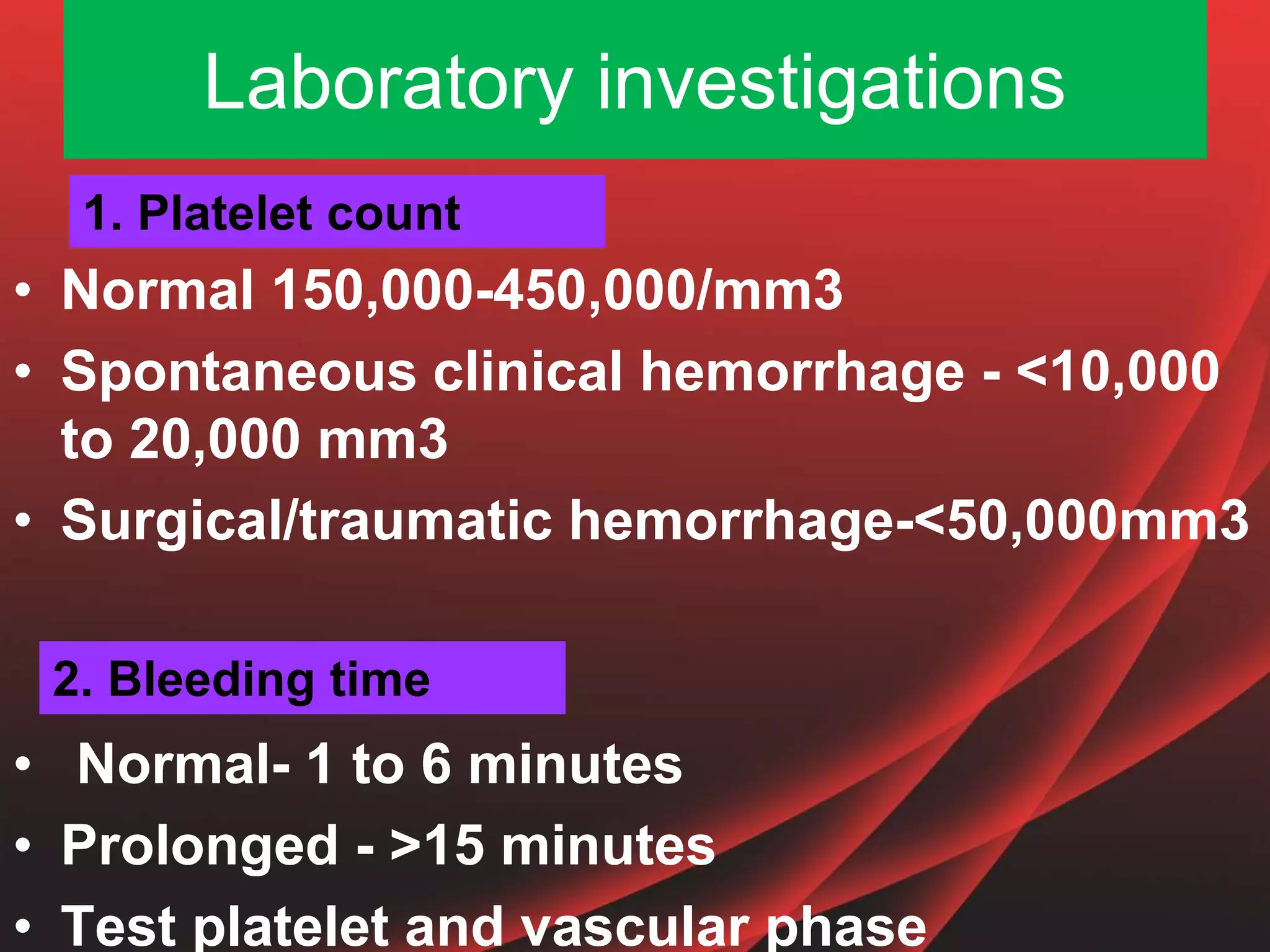
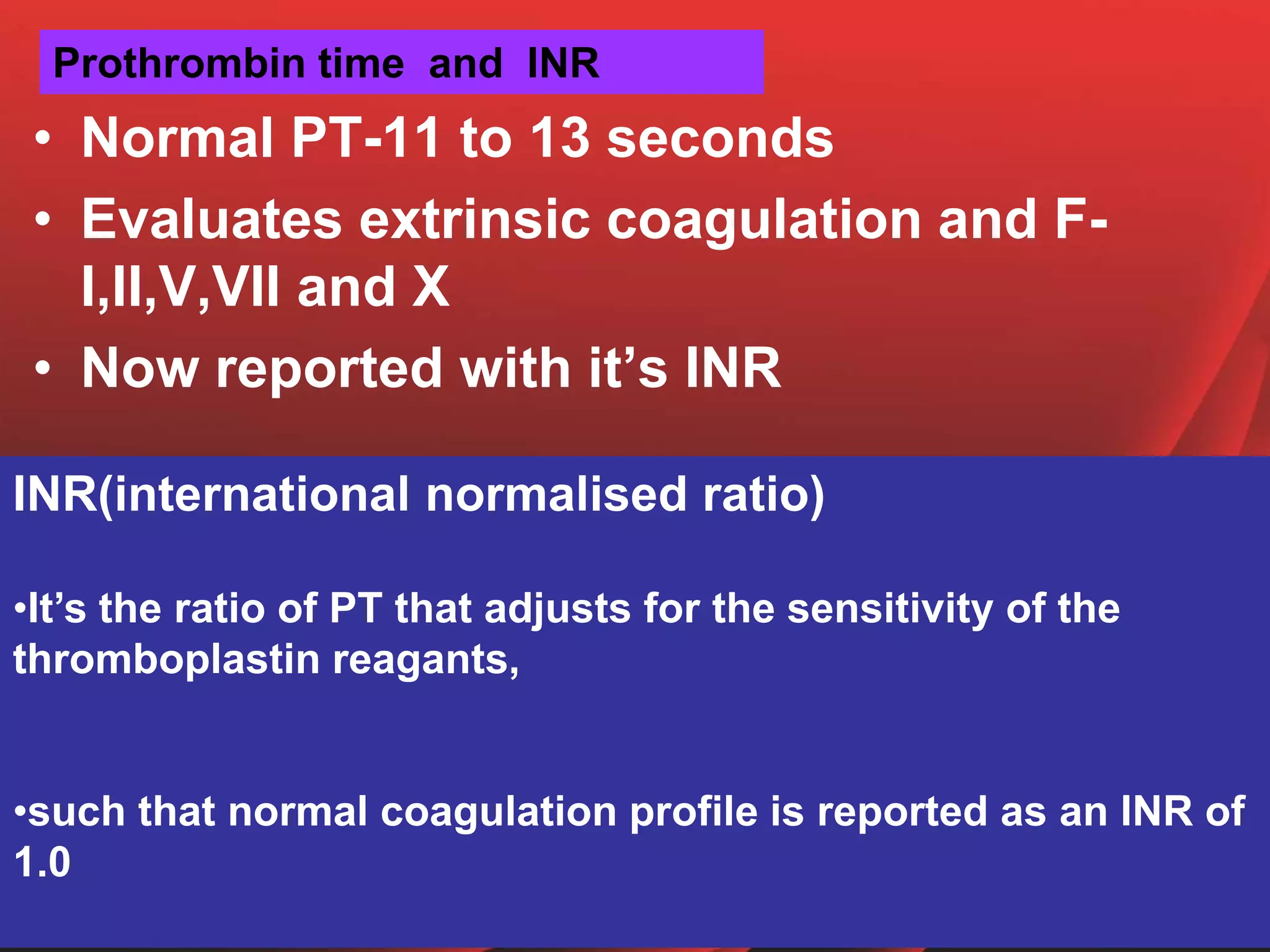
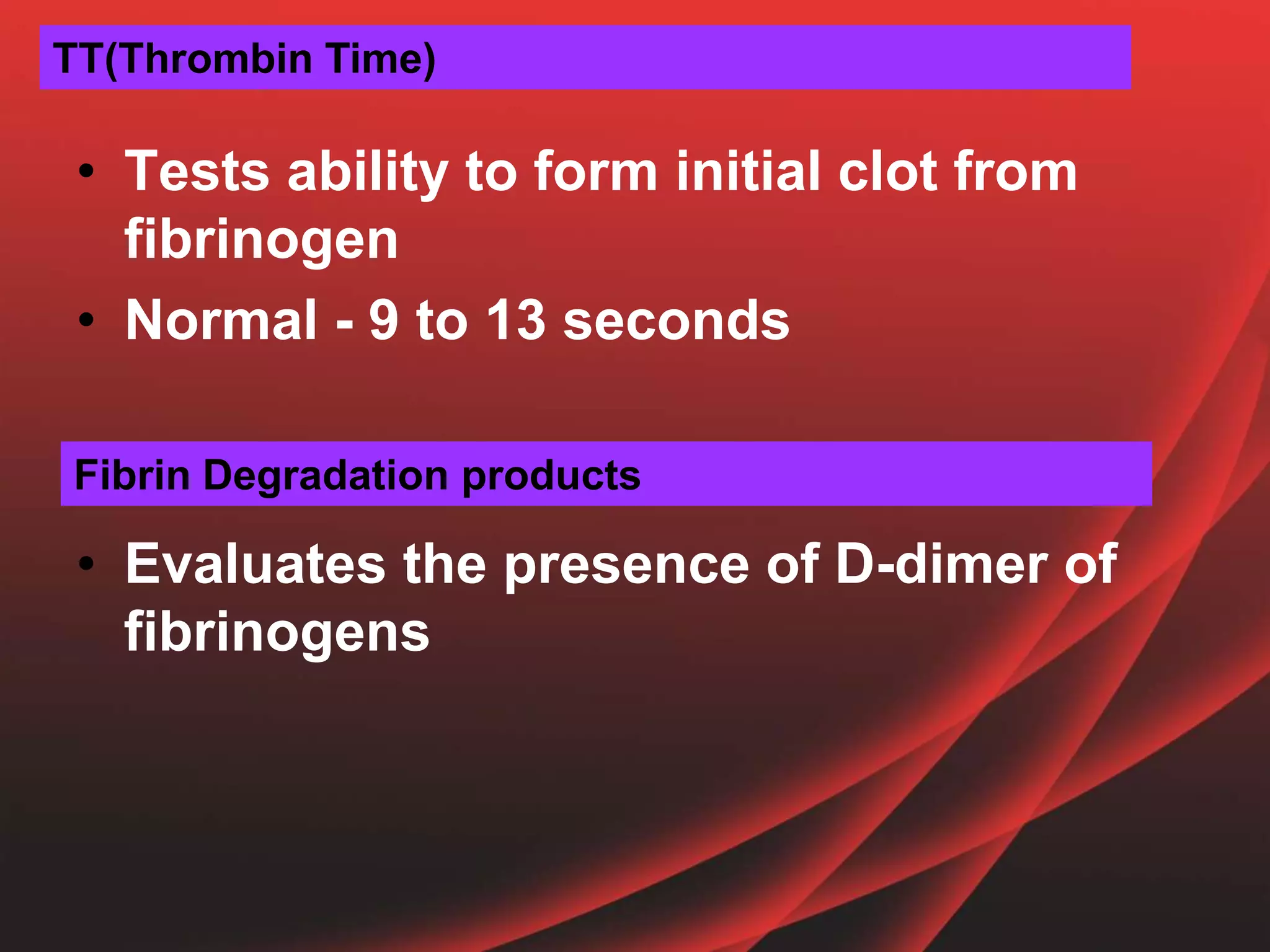
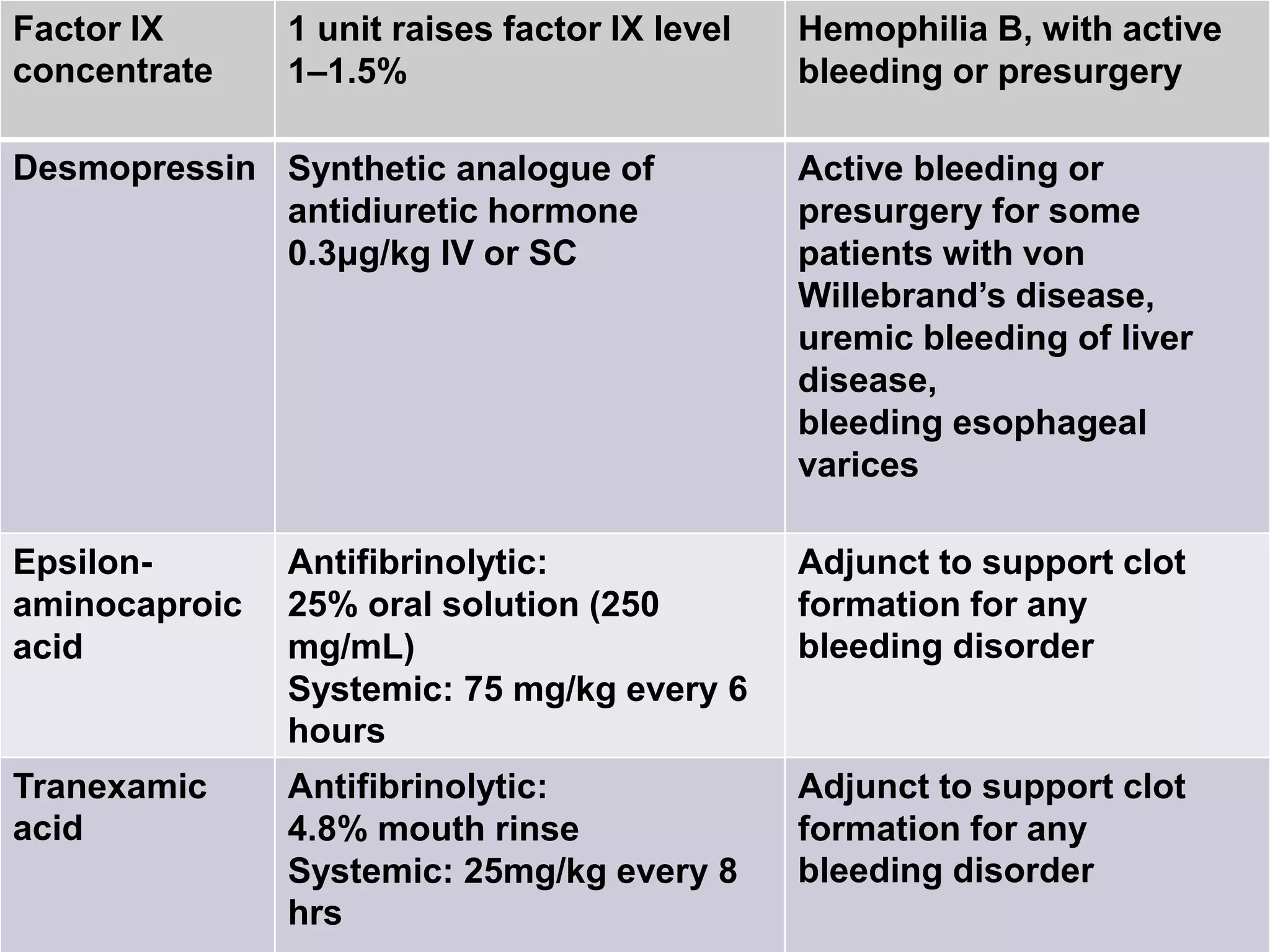
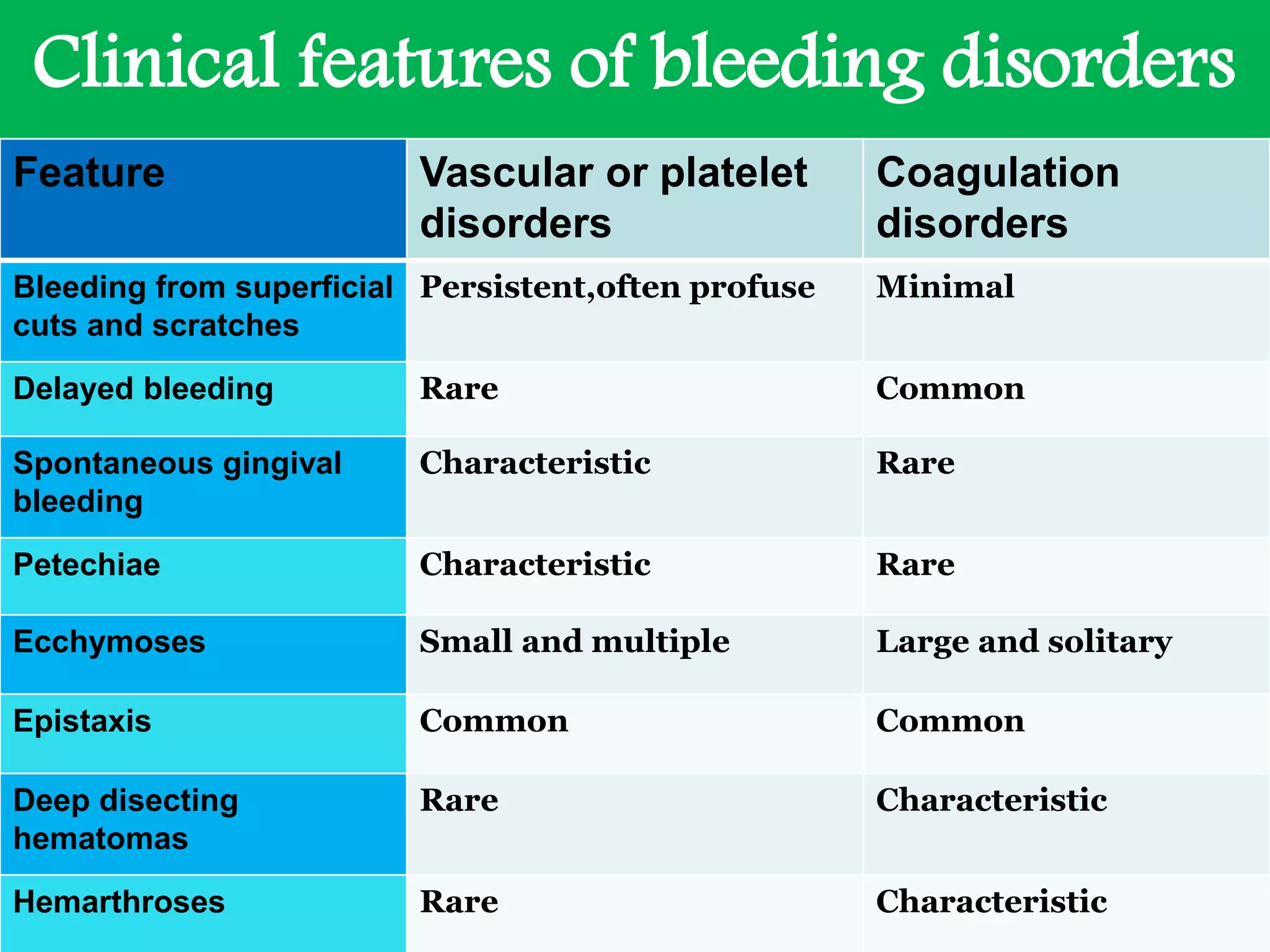
This document provides information on bleeding and clotting disorders. It discusses the pathophysiology of hemostasis including the vascular, platelet, coagulation, and fibrinolytic phases. It describes different types of bleeding disorders like vessel wall disorders, platelet disorders, and coagulation disorders. Laboratory tests for identifying bleeding disorders are outlined. Oral manifestations and dental considerations for management are summarized. Local hemostatic agents and systemic agents for different bleeding disorders are also mentioned.