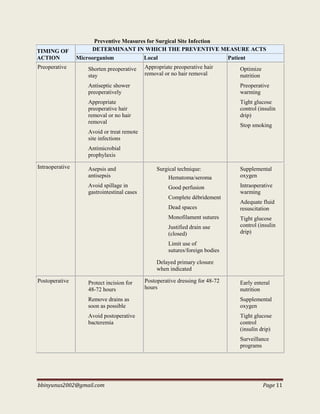
This document contains a compilation of surgical tutorials by Dr. Bashir Bin Yunus. It begins with definitions and characteristics of various types of surgical infections. Common organisms that cause surgical infections are discussed, including Staphylococci, Streptococci, Pneumococci, and various gram-negative bacteria. Three main types of infections of significance in surgical patients are described in detail: surgical site infections, which can be superficial, deep, or involve organs/spaces; bloodstream infections like bacteremia and septicemia; and systemic inflammatory response syndrome. Classification criteria and signs of infection are provided for each type.






















































































![bbinyunus2002@gmail.com Page 104
II. Personal Relationship
A. Genuine bond of communication and personal responsibilities.
B. Do not convey a sense of hurry and inadequate time for explanations.
C. Demonstrate skills to contribute to diagnosis and treatment.
D. Specific treatment.
E. Informed consent
III. General Preparation of the Patient
A. Psychological preparation
1. Pre-op steps should be enumerated, justified and explained.
2. Surgeons should not equivocate in discussing possible disfiguring operations.
HISTORY
Previous illness
Previous surgery and anaesthetic experience
Concurrent diseases
Drug therapy e.g prolonged use of steroids
Social hx: alcohol, smoking
EXAMINATION
Respiratory system: treat infections. Spirometry. BGA/PH checks
Cardiovascular system: anaesthesia reduces CO by about 20%. Note- predictors of
cardiac risk (MI, CCF, etc), pt’s functional capacity, the procedure to be carried out
Urinary system: Albumin, casts, cells, sugar, ketones, urea level
Gastrointestinal system: carious and loose tooth. Treat mouth infections. Stool exam
→deworm
Blood picture: CBC, Sickling test. Bld trx at least 3 days to time of surgery. May use parenteral
iron therapy or recombinant erythropoietin. For bleeding tendency/jaundiced pts-platelets,
prothrombin, bleeding and clotting time
Hydration and Nutrition: ↓ K → difficulties with reversal of muscle relaxants.
Malnutrition: BMI used (weight[kg]/ht2[m2])](https://image.slidesharecdn.com/surgerytutorialsformedicalstudents-151111181127-lva1-app6892/85/Surgery-tutorials-for-medical-students-104-320.jpg)