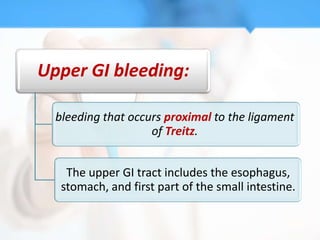
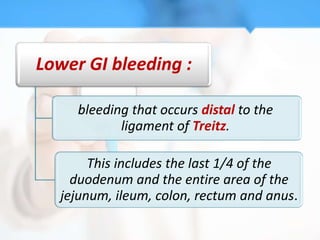
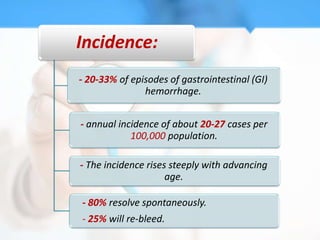
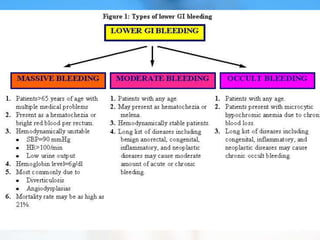
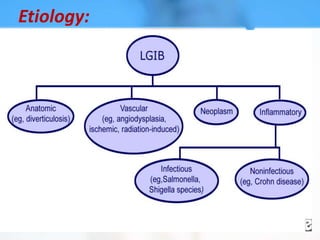
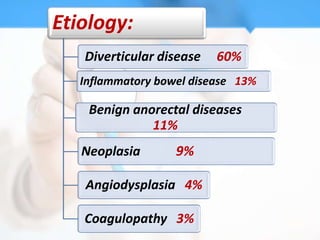
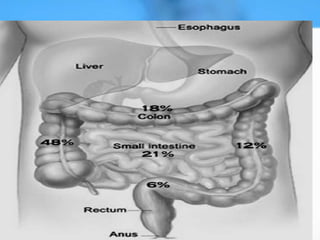
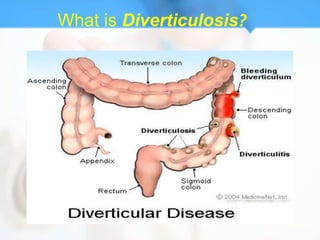
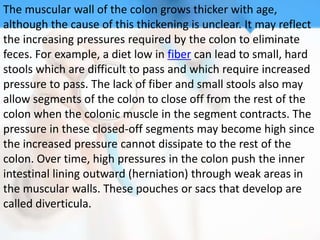
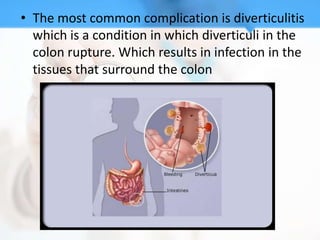
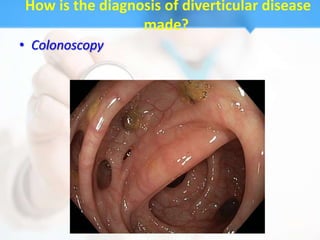
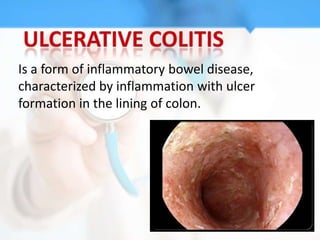
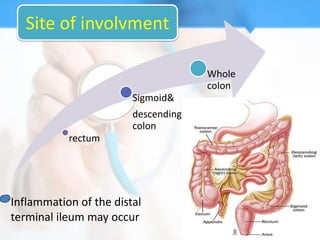
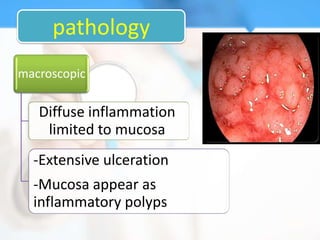
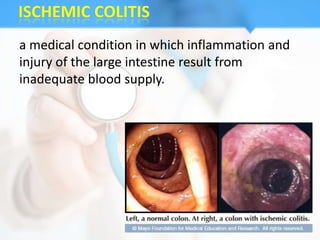
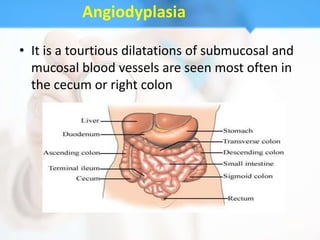
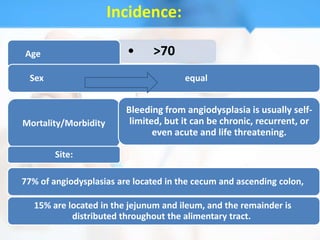
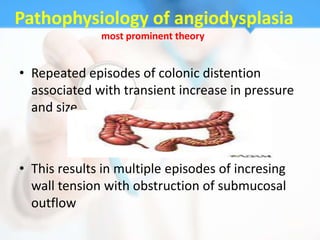
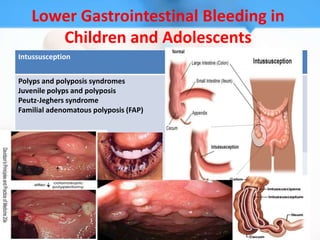
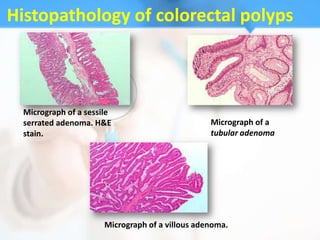
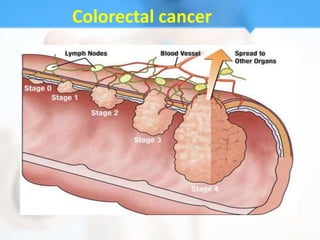
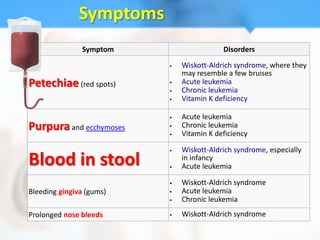
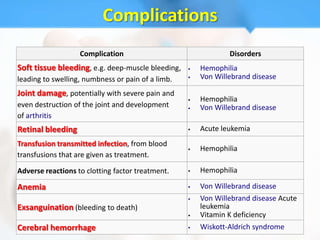
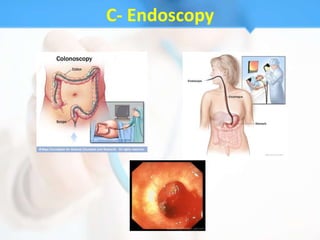
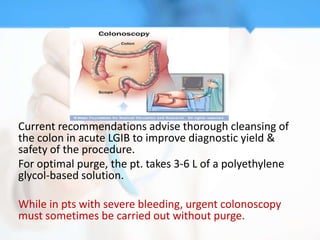
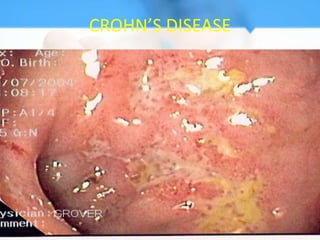
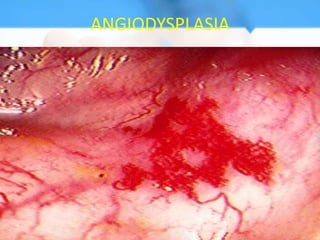
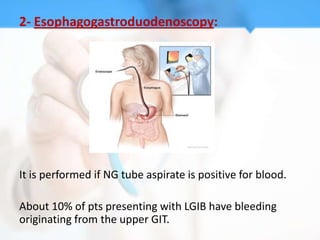
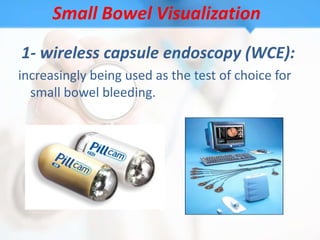
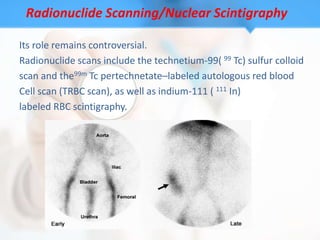
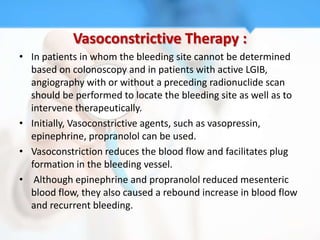
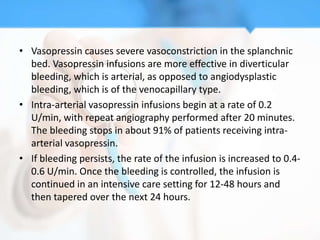
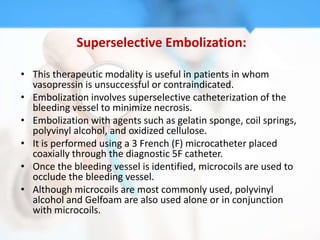
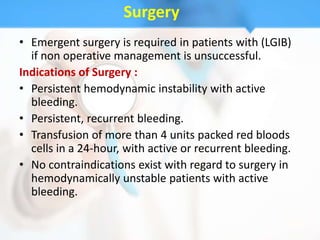
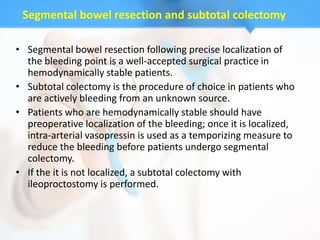
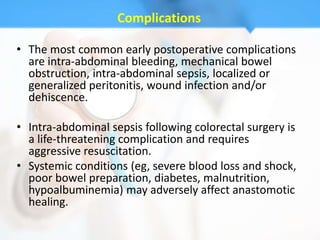
The document discusses lower gastrointestinal bleeding, including its definition, causes such as diverticular disease, inflammatory bowel disease, angiodysplasia, and coagulopathy. It covers the clinical presentation, various diagnostic tests including colonoscopy, capsule endoscopy and nuclear scintigraphy. Colonoscopy is the mainstay for evaluation as it can both diagnose the bleeding source and provide therapeutic treatment in many cases.