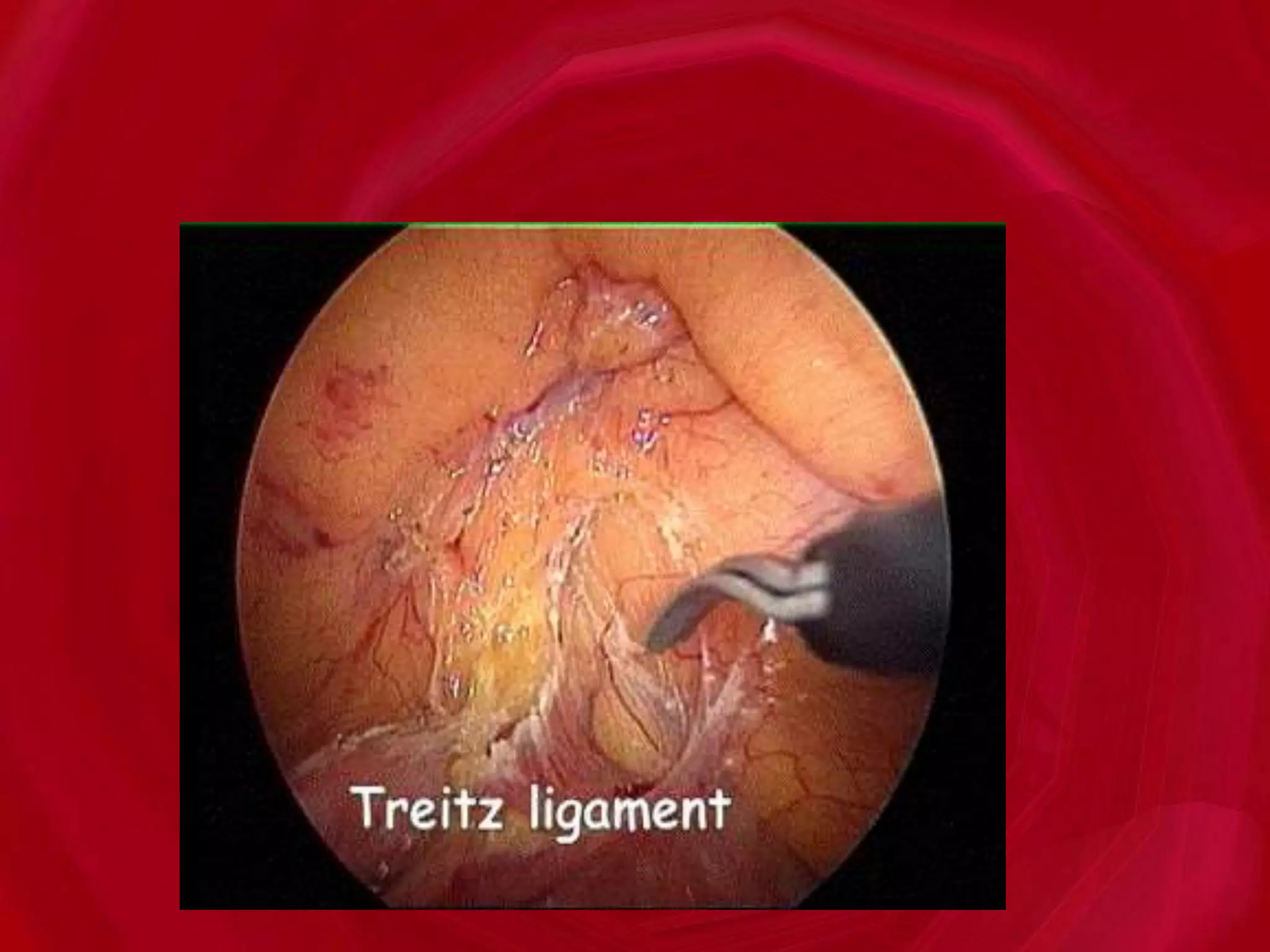
This document discusses gastrointestinal bleeding, including:
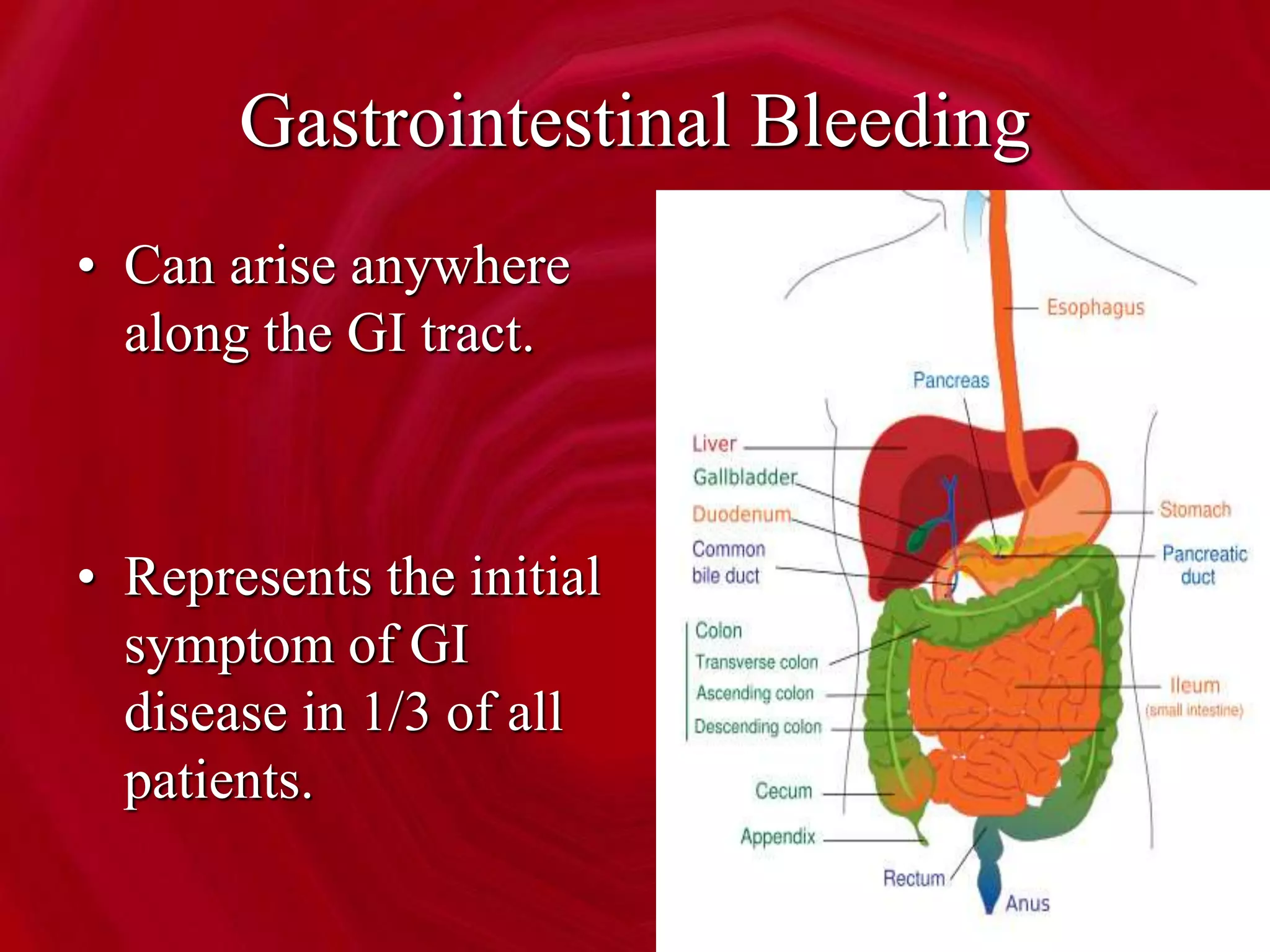
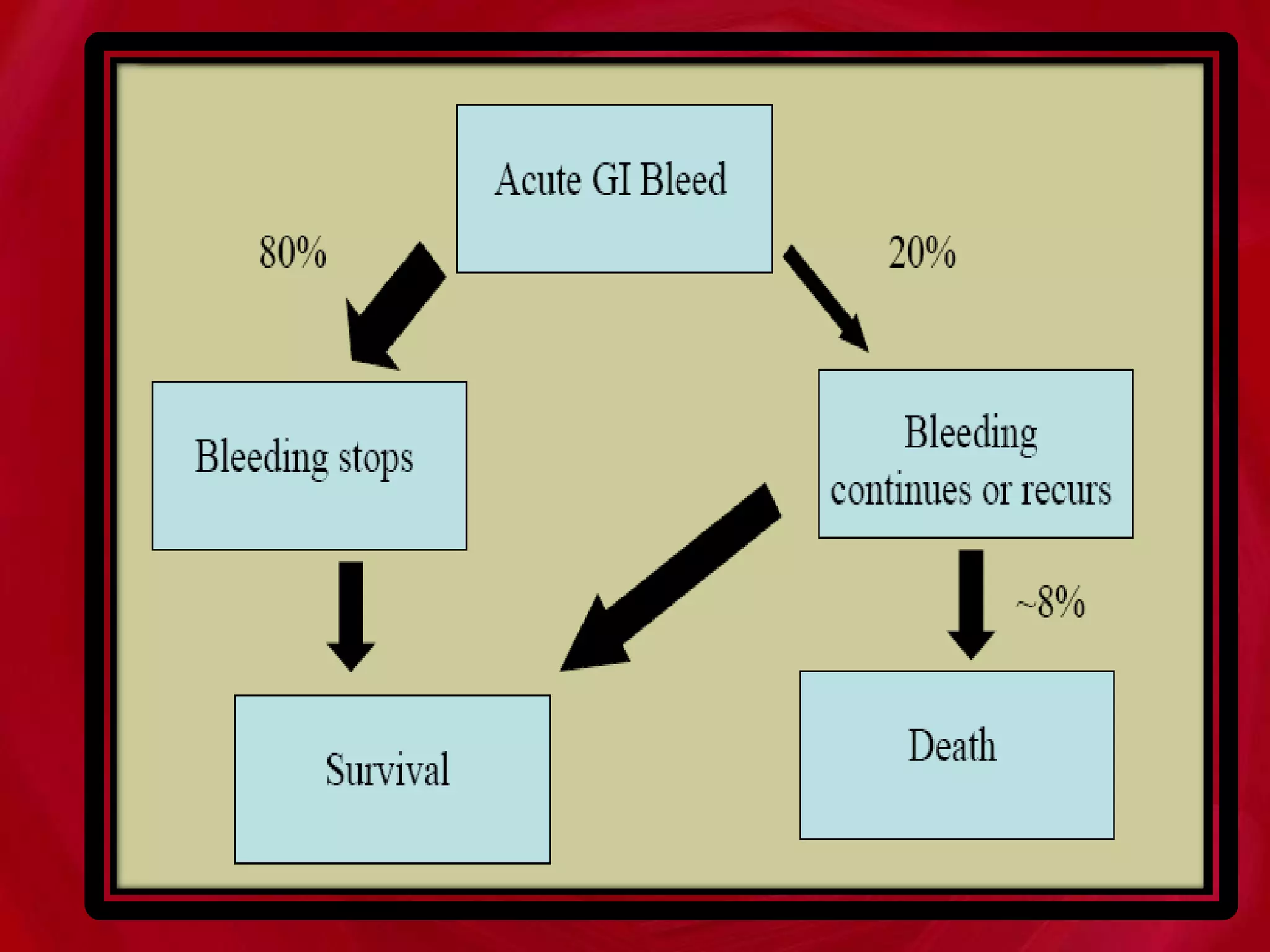
- Gastrointestinal bleeding can arise from any location in the GI tract and represents the initial symptom of GI disease in 1/3 of patients.
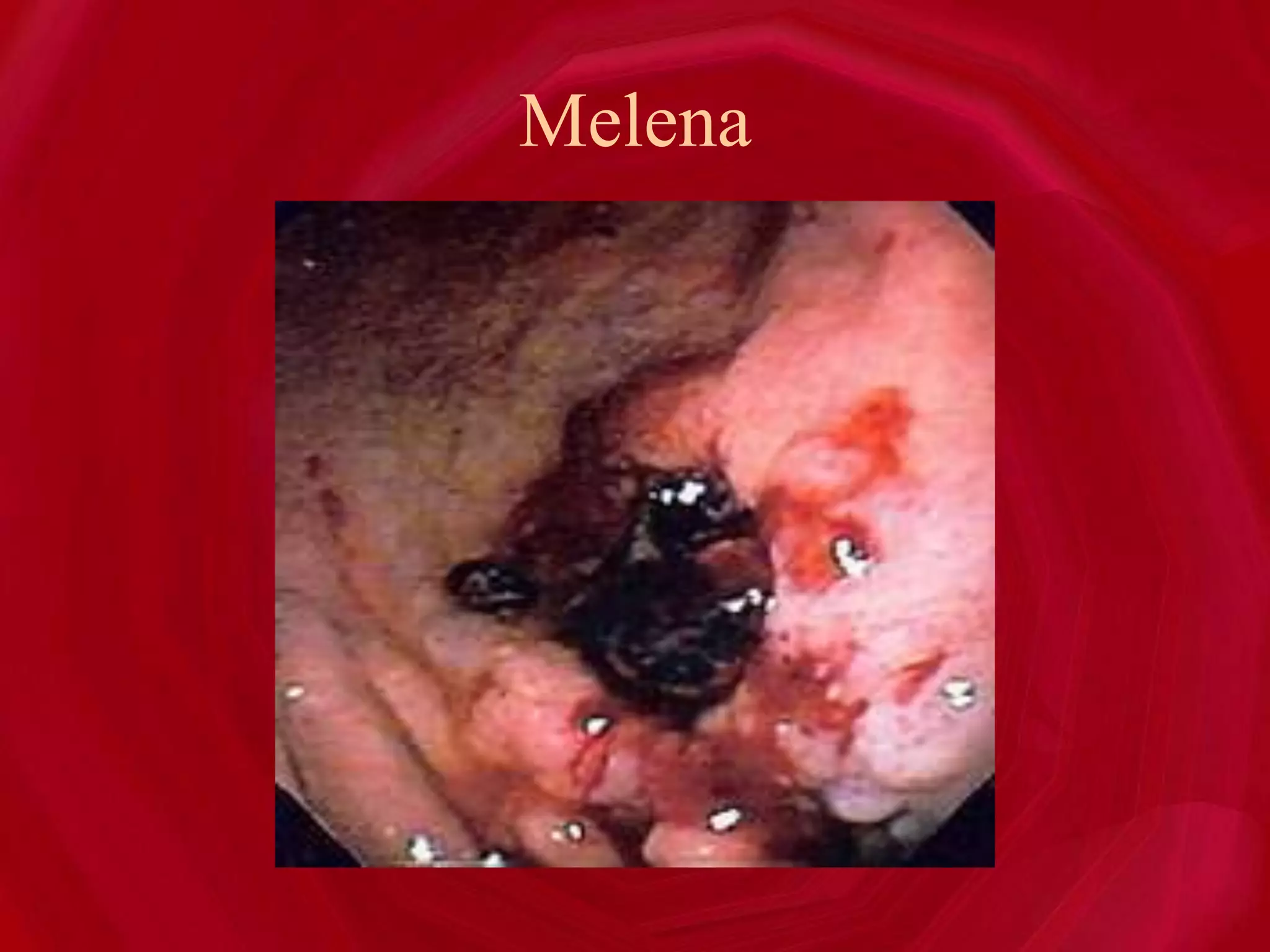
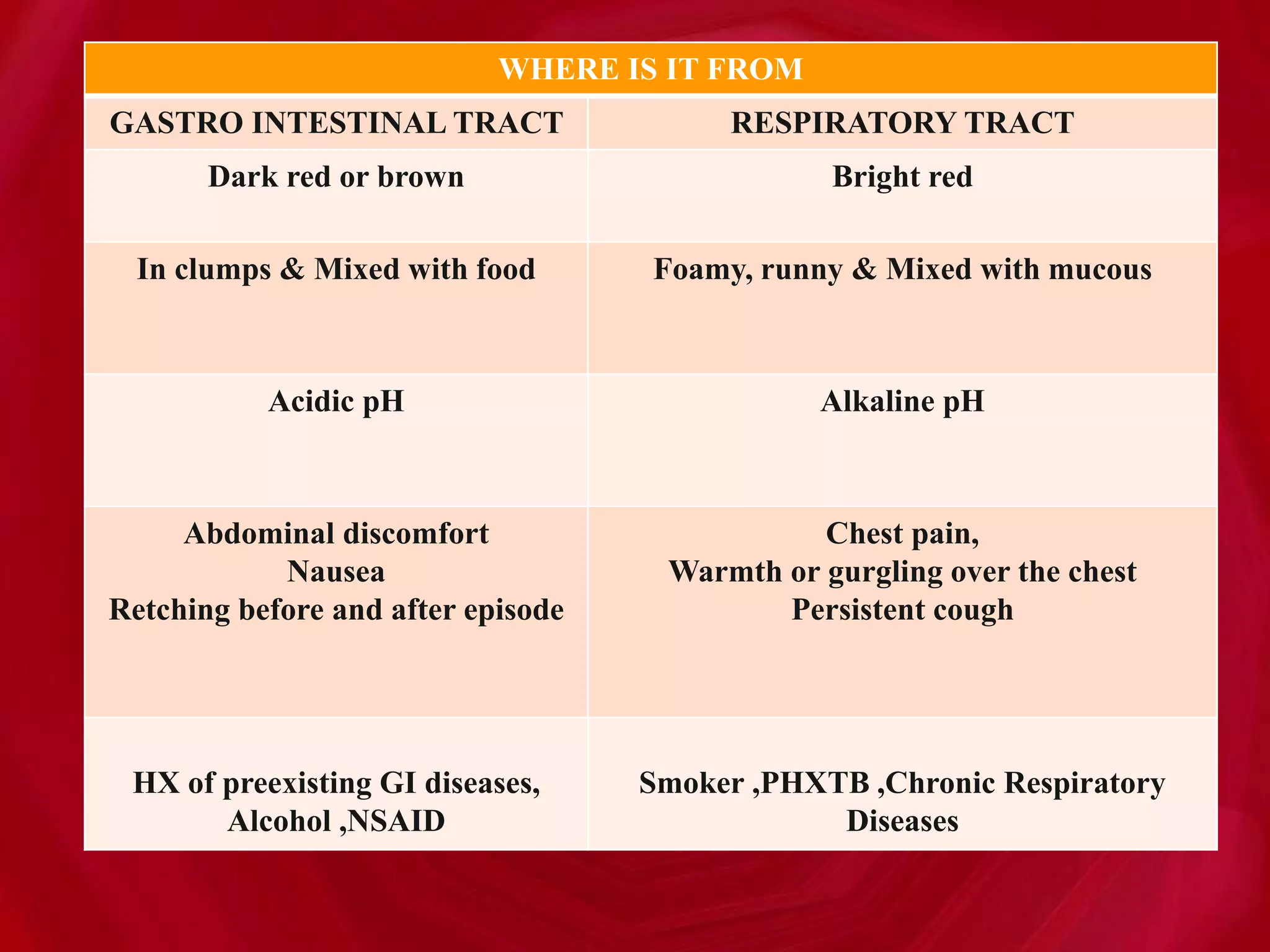
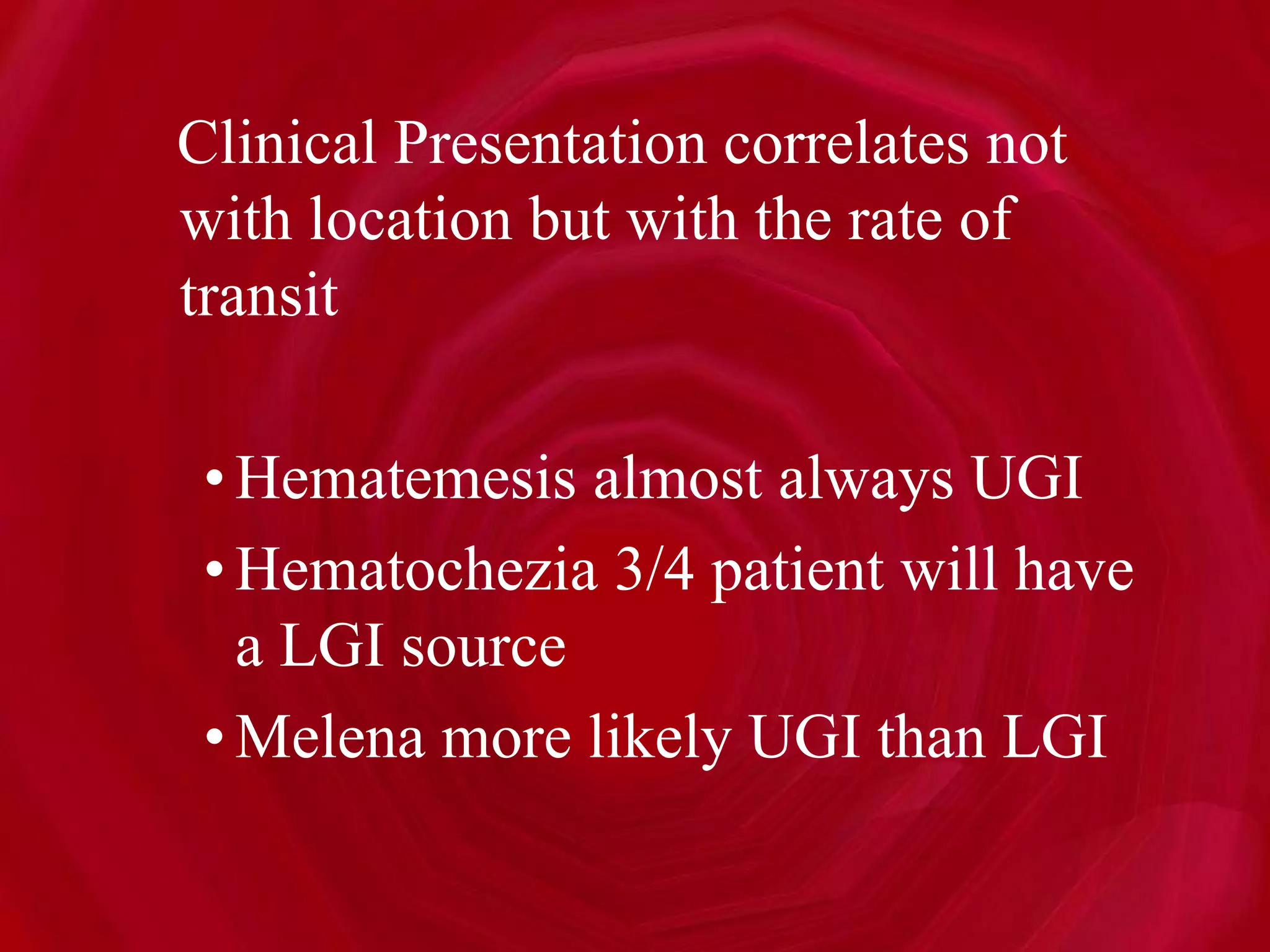
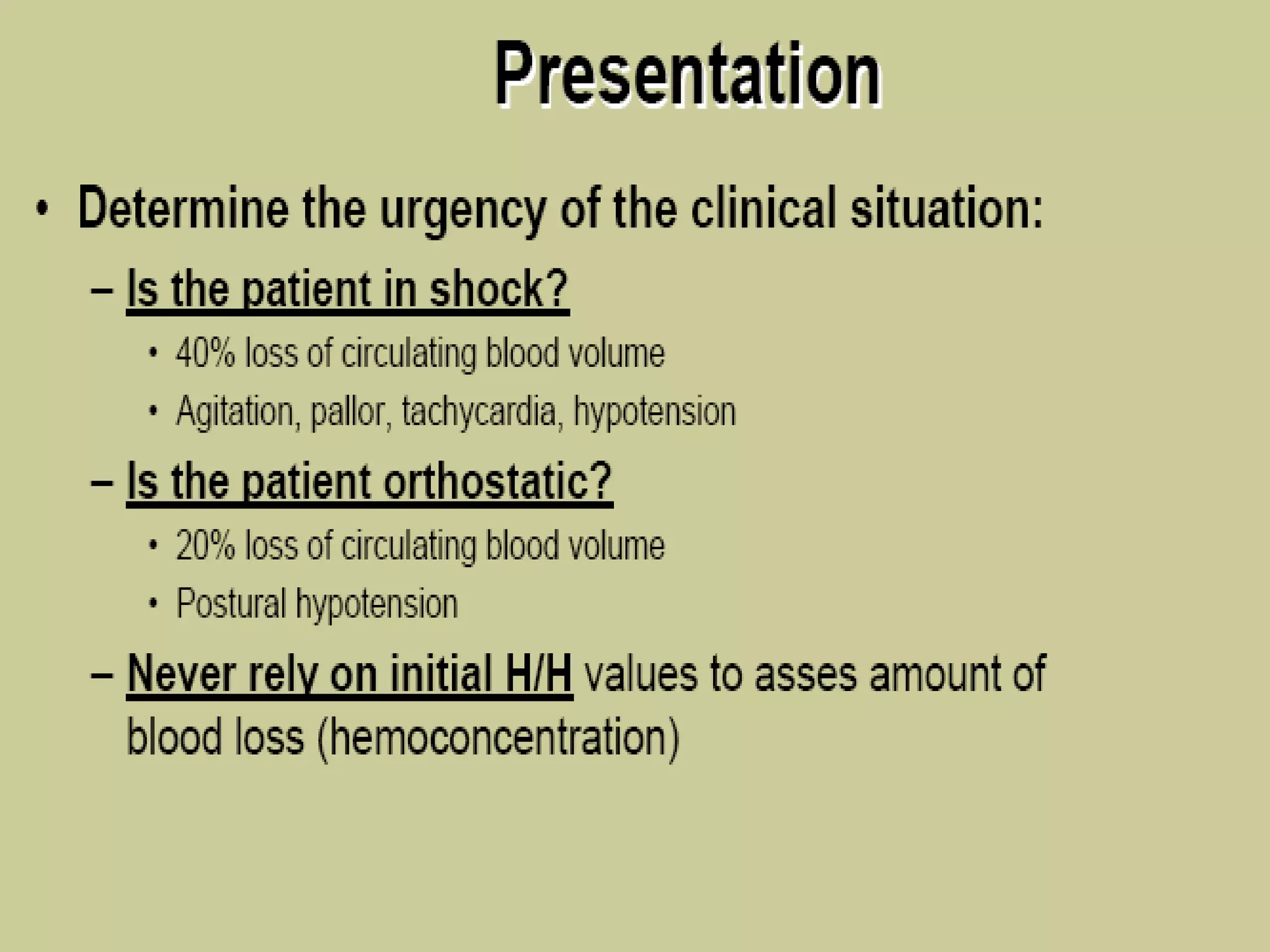
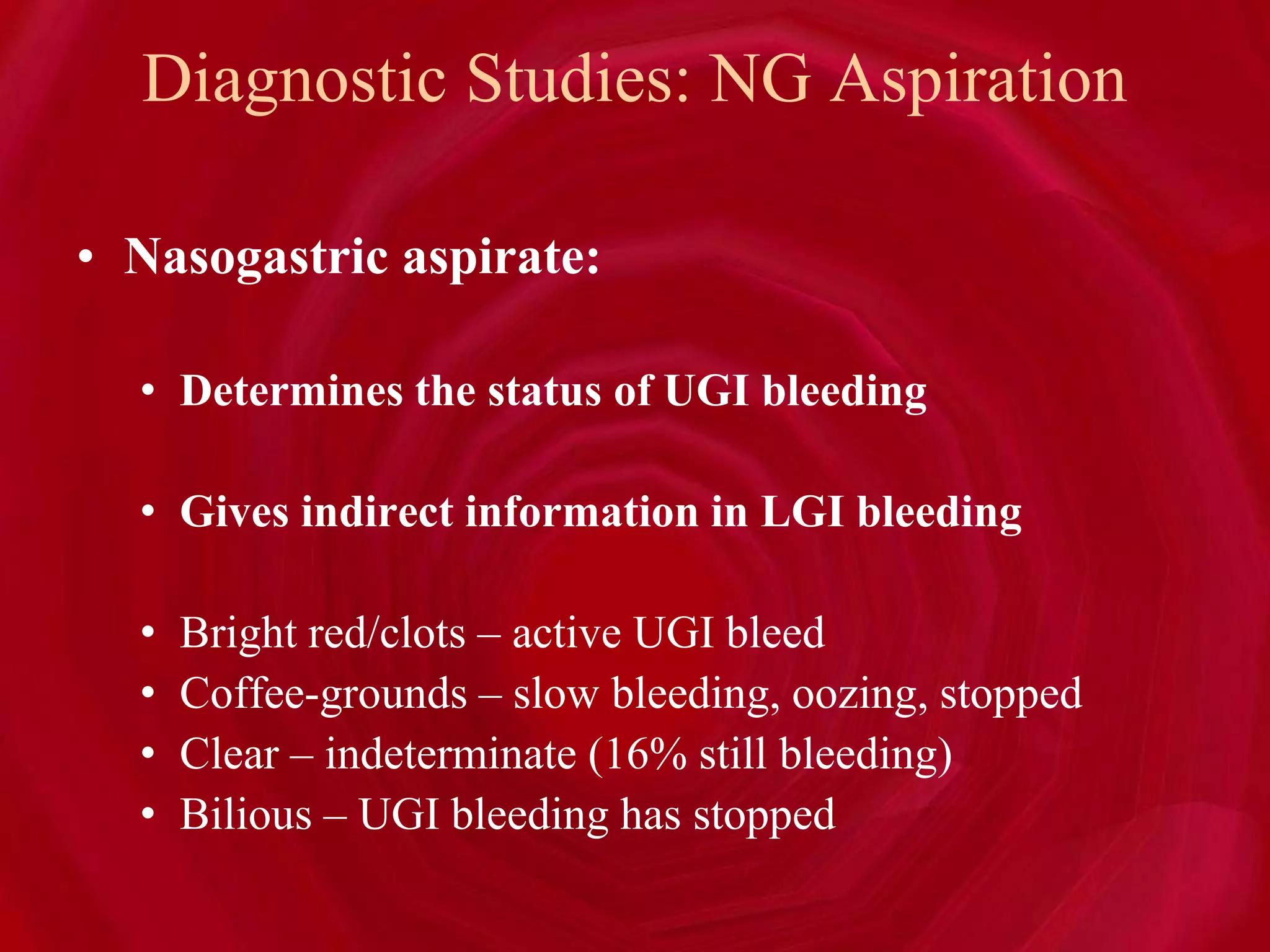
- Clinical presentations of GI bleeding include hematemesis, melena, hematochezia, occult bleeding, and symptoms of blood loss/anemia.
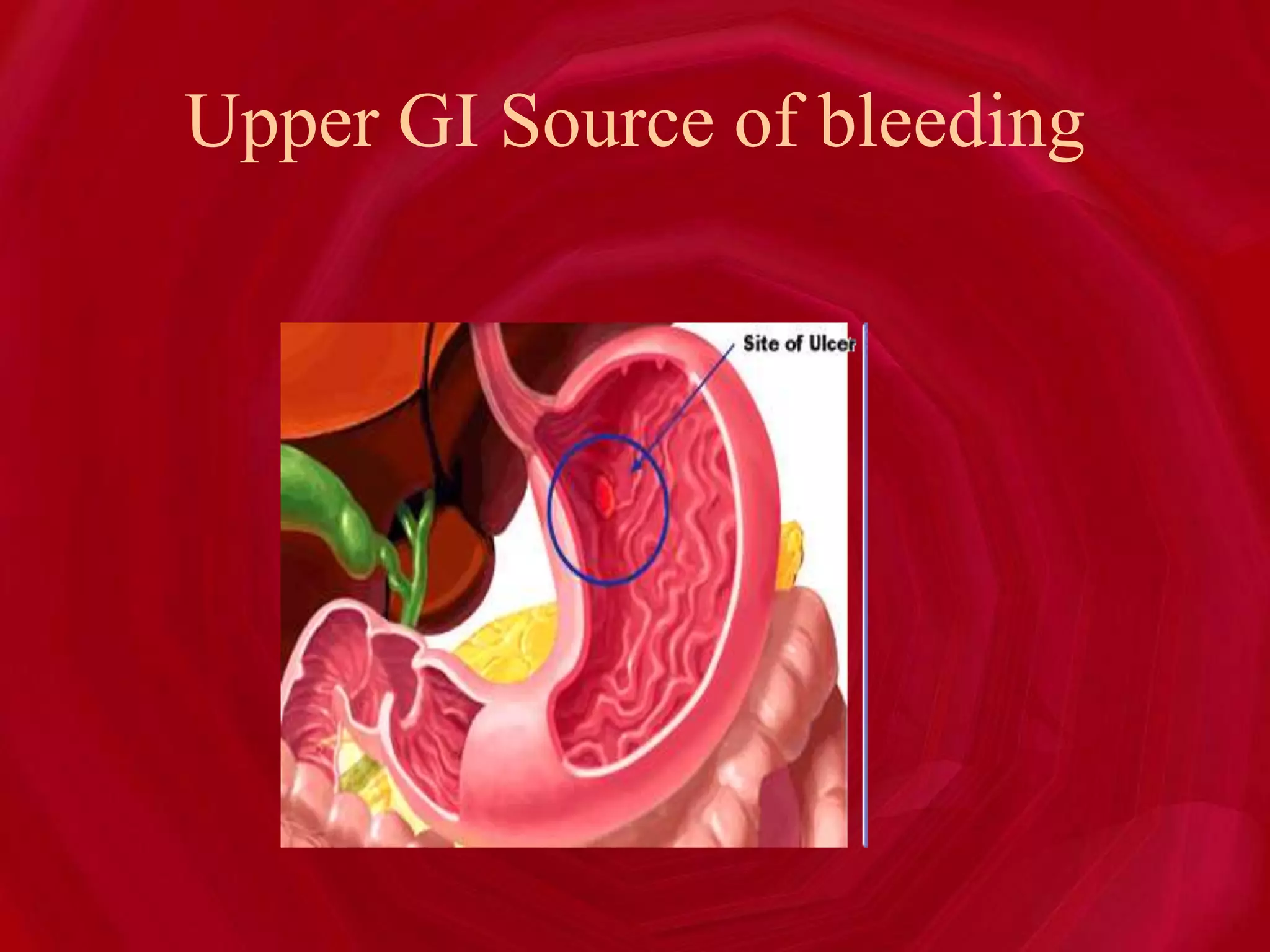
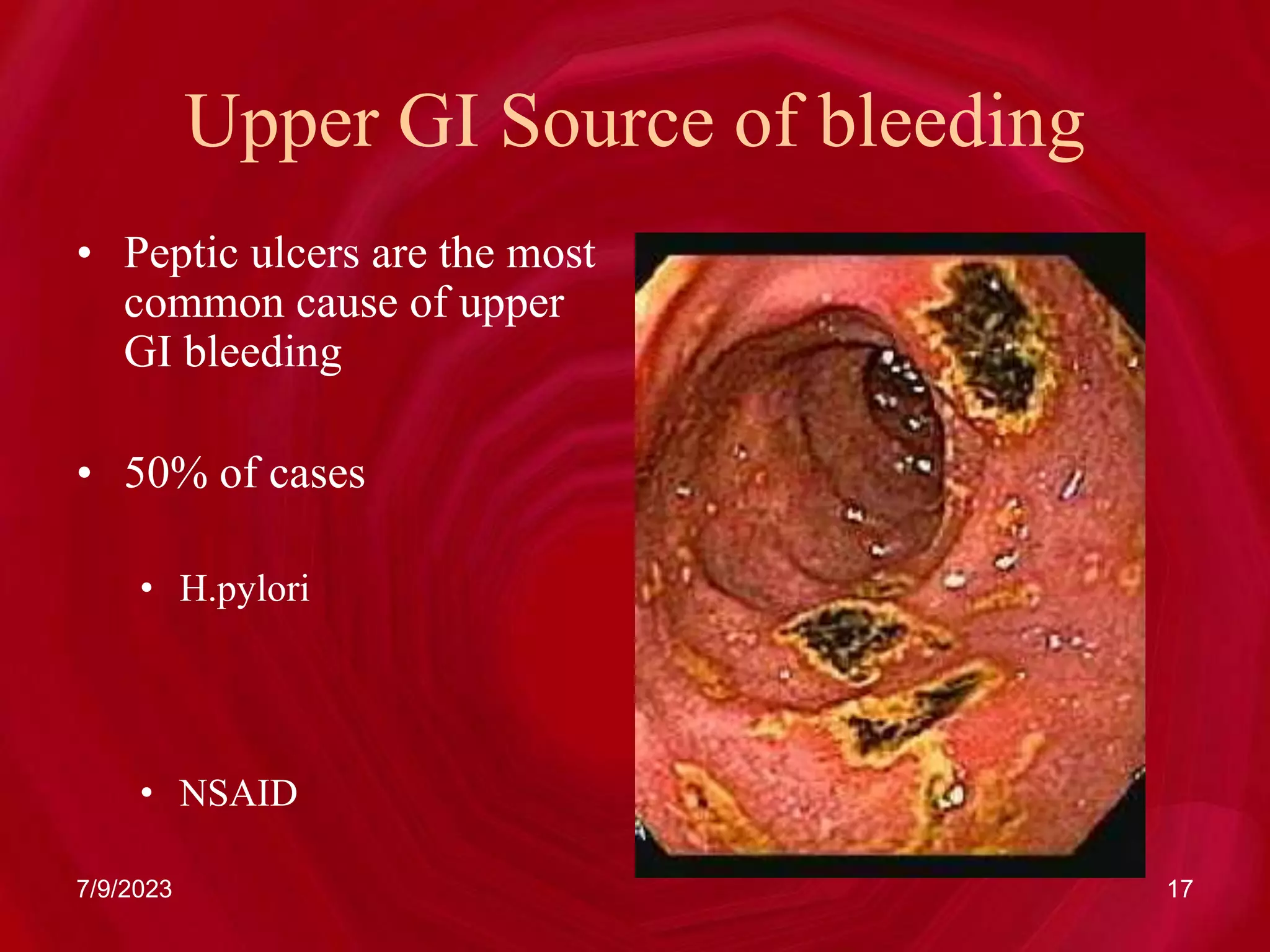
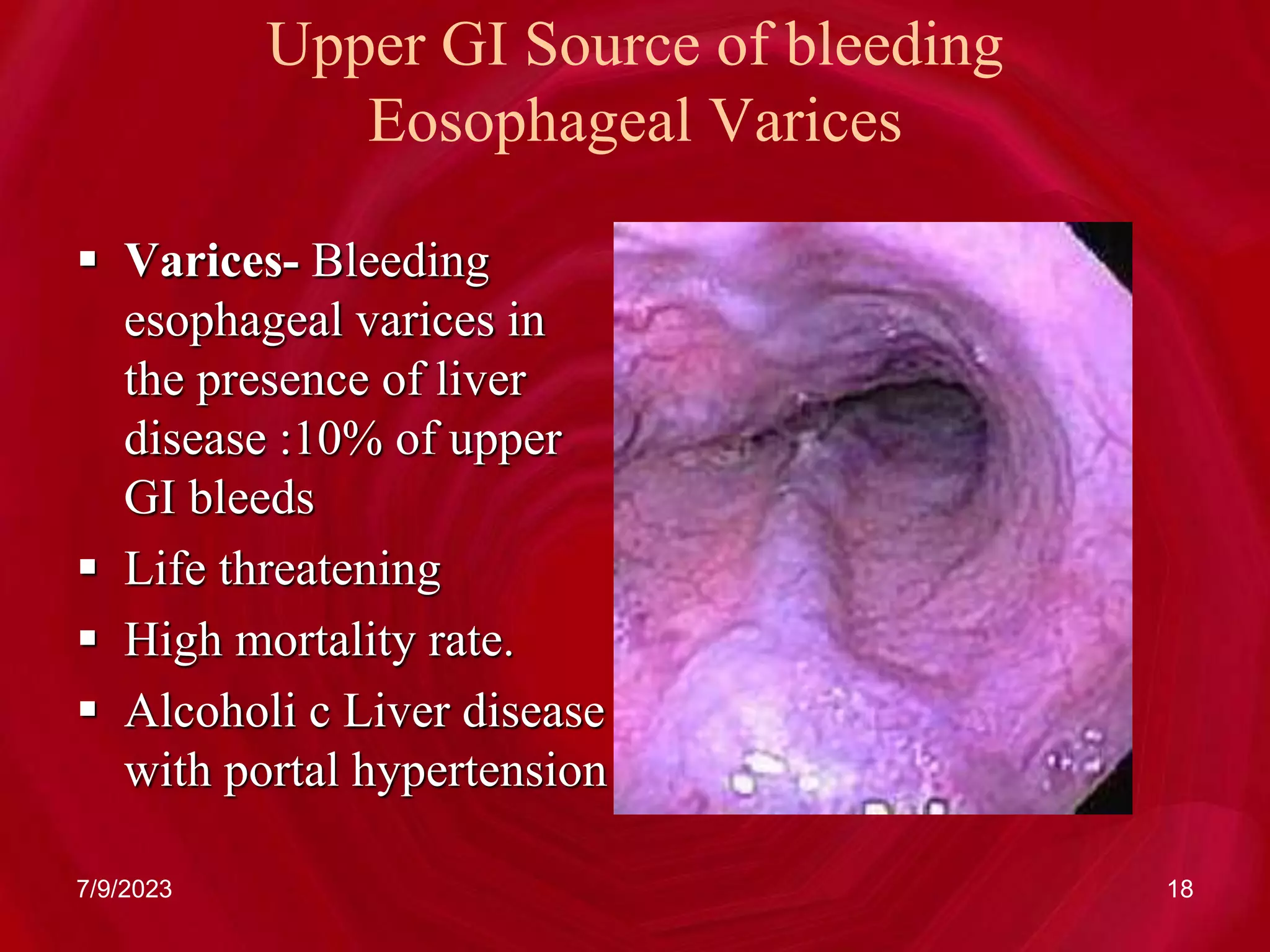
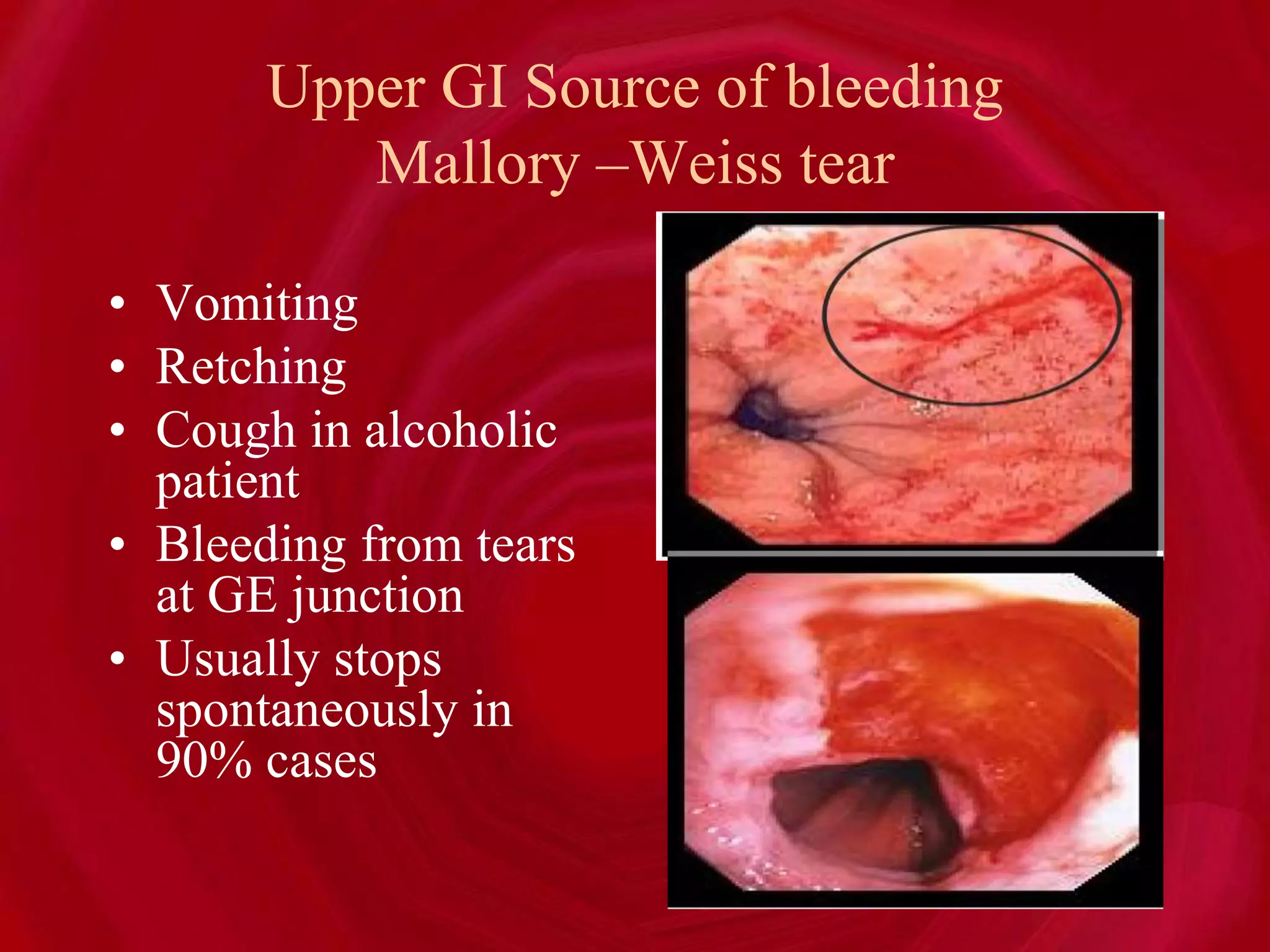
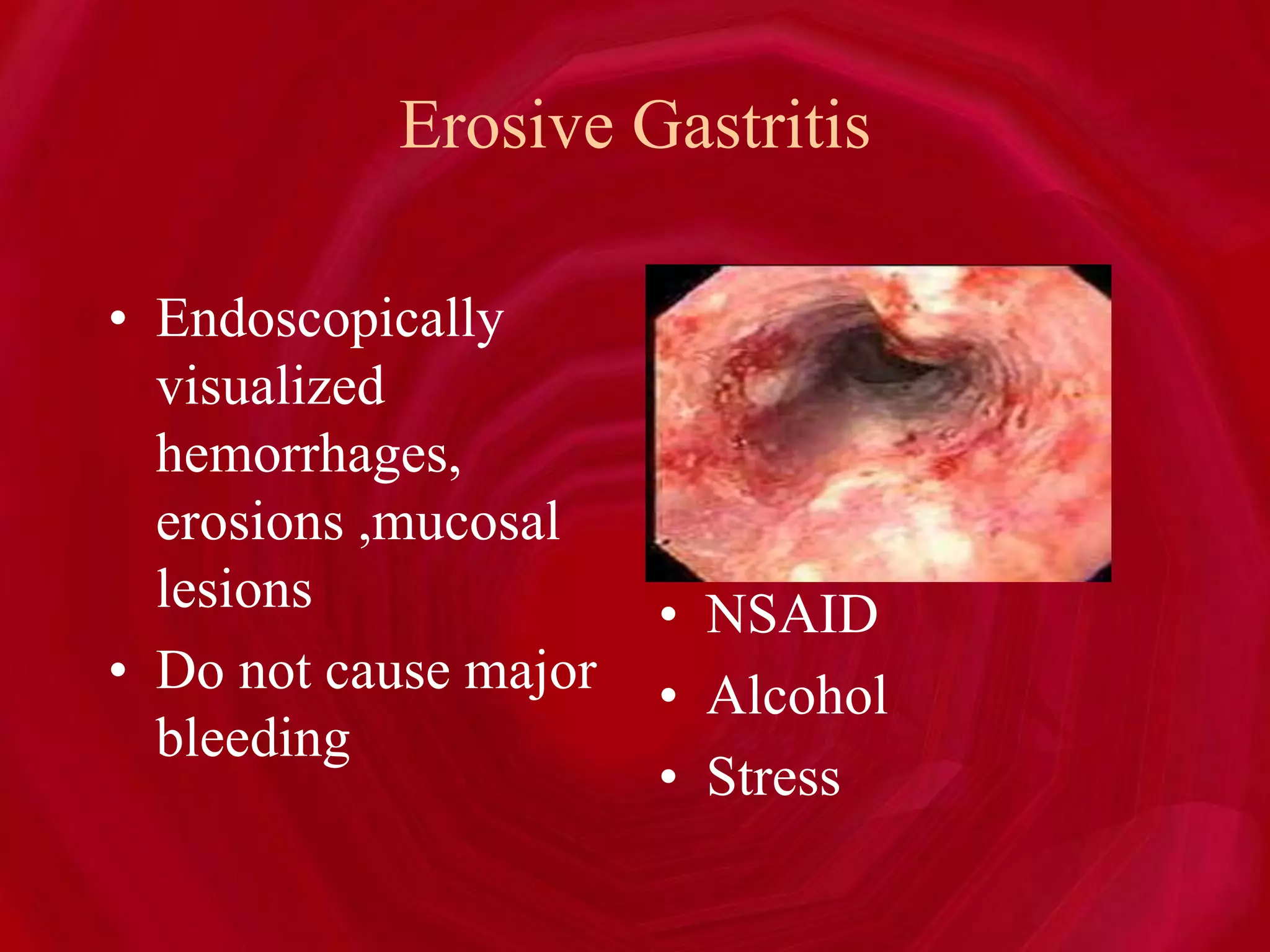
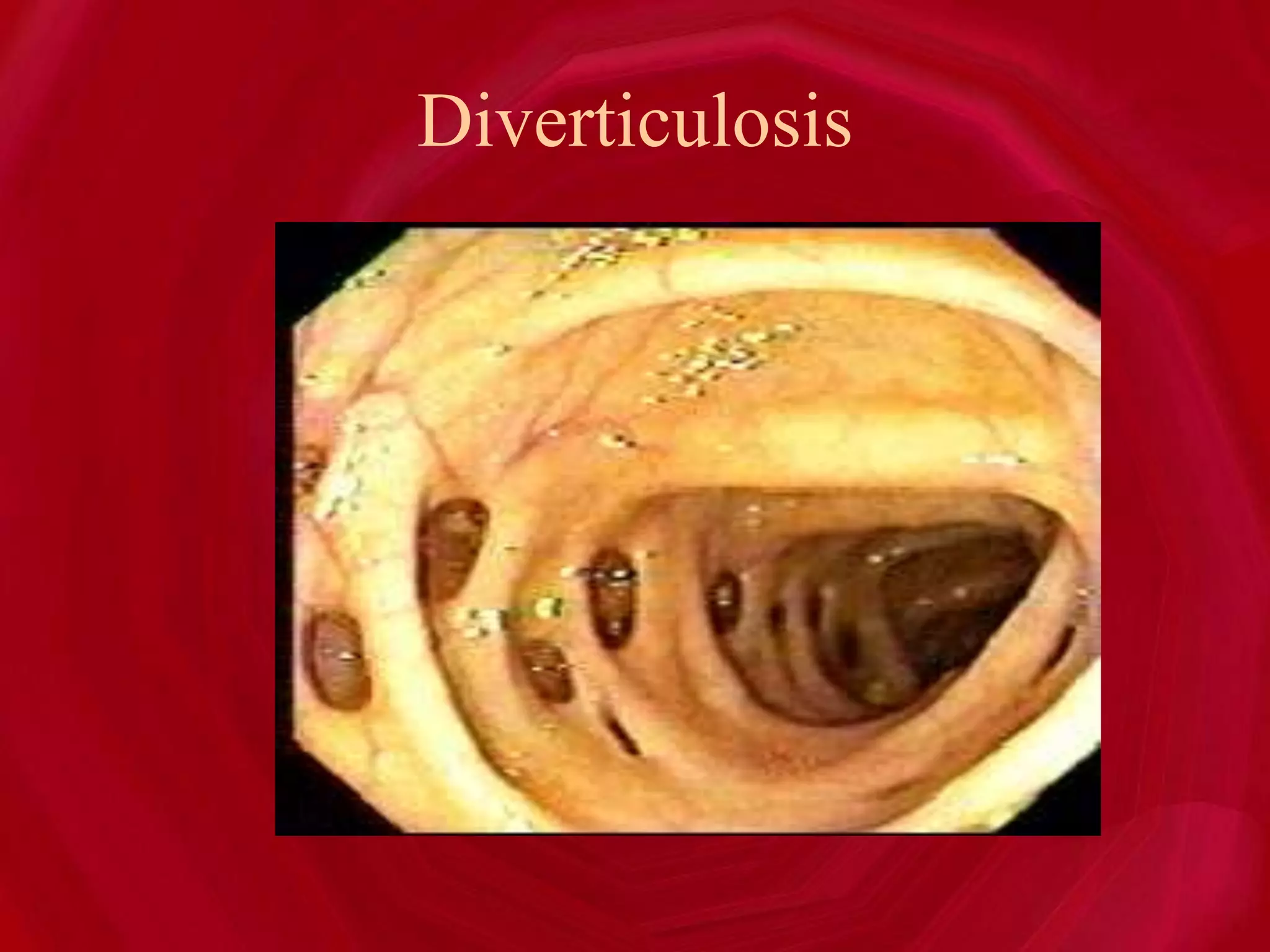
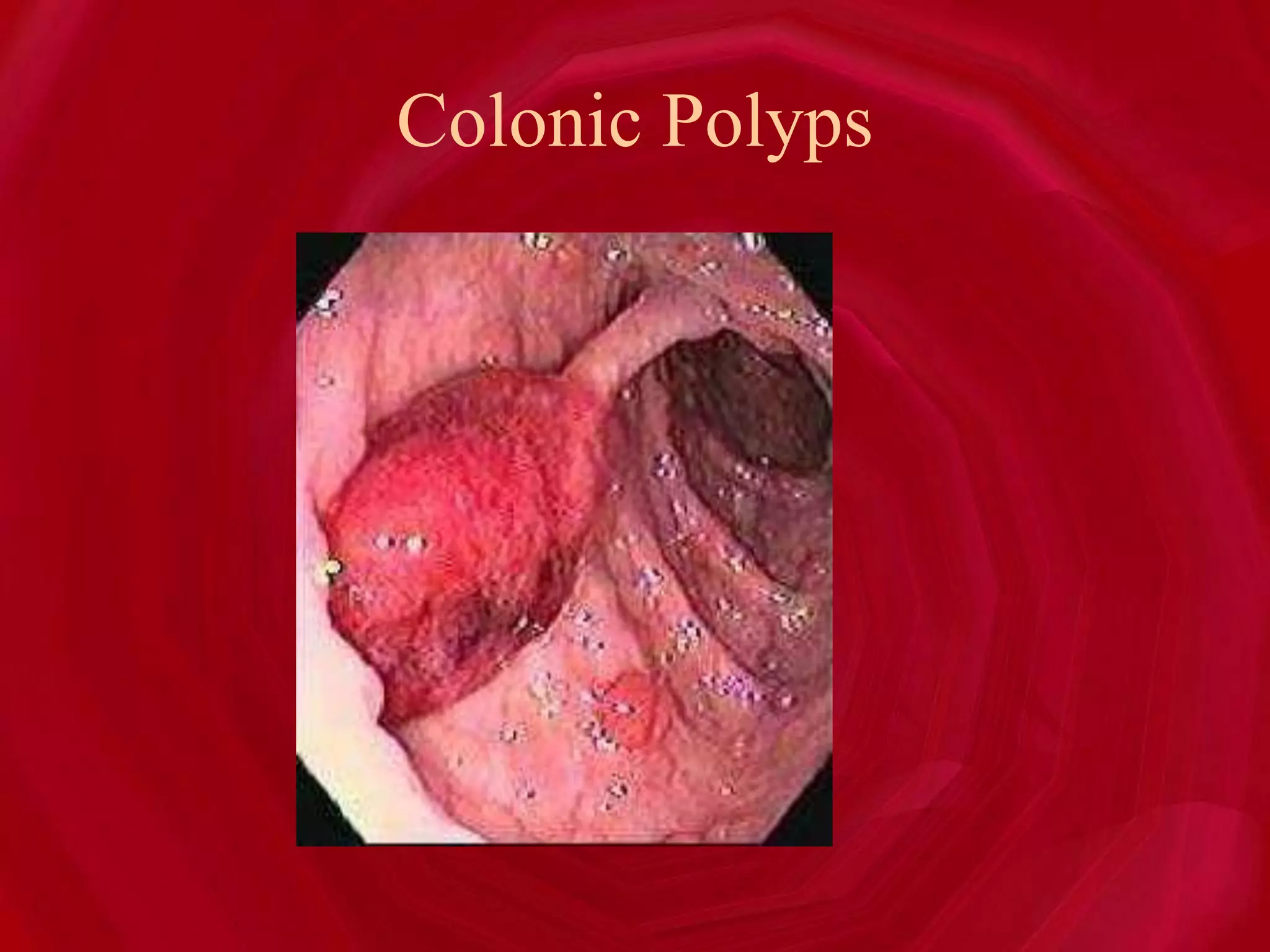
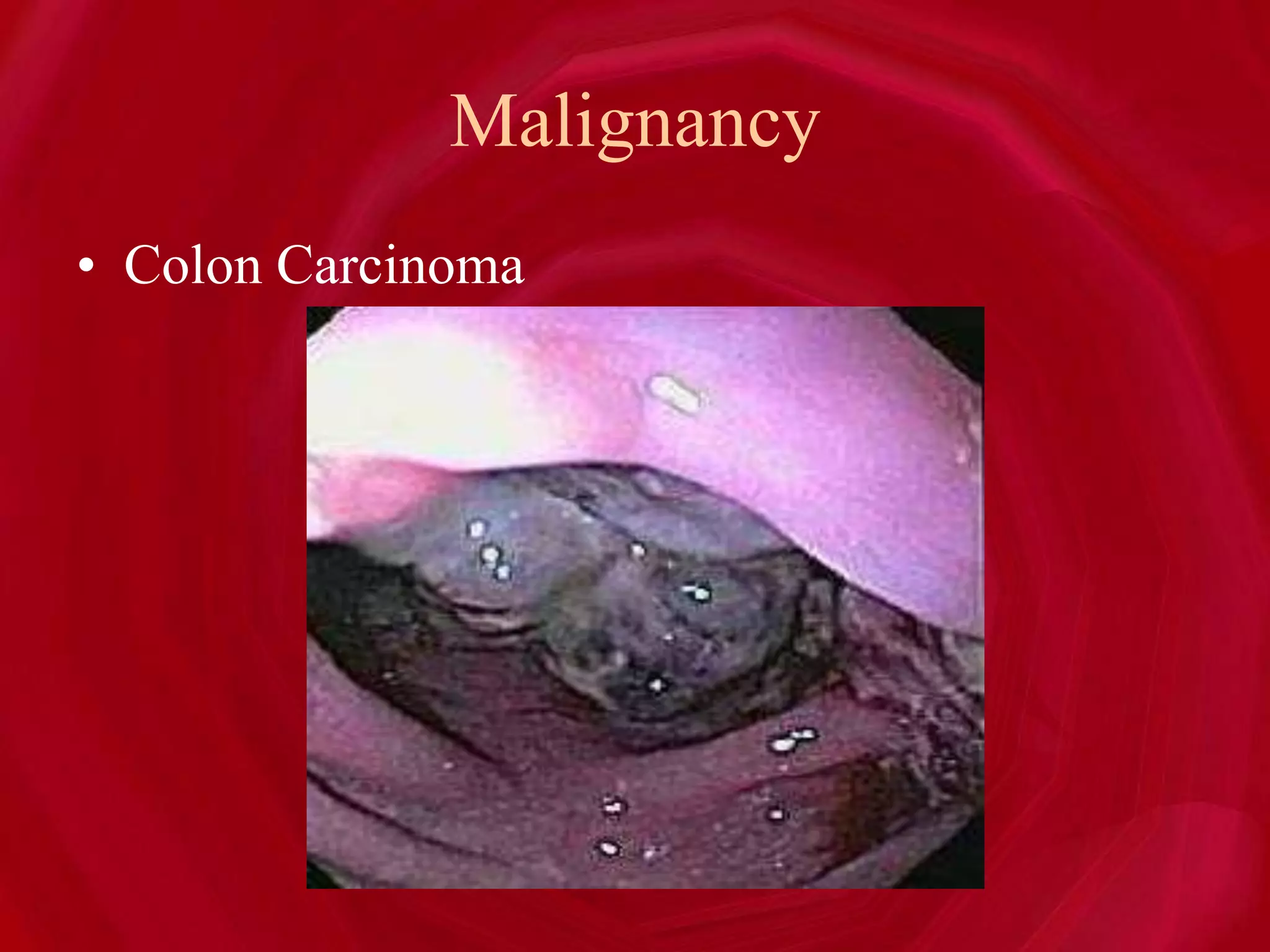
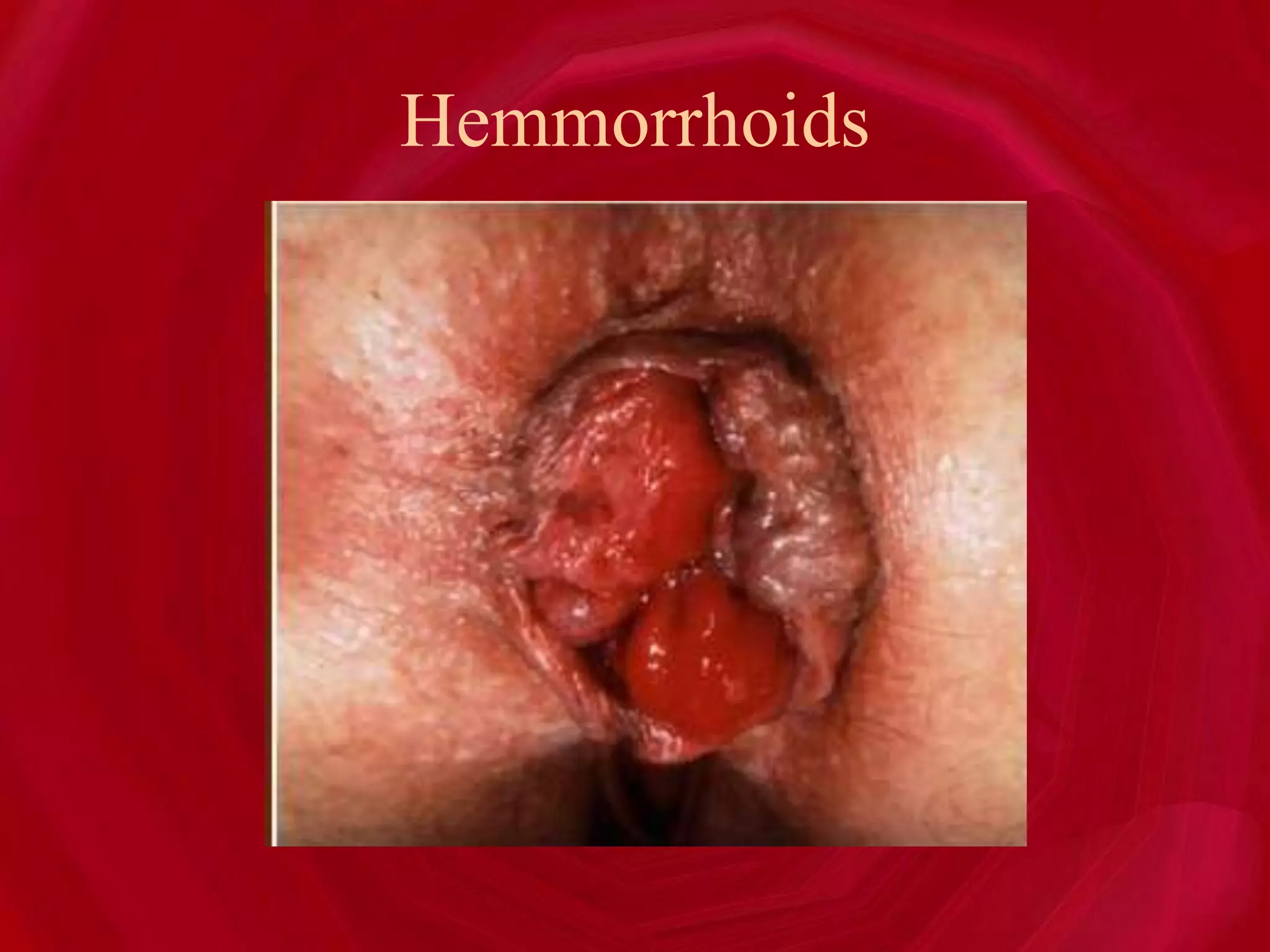
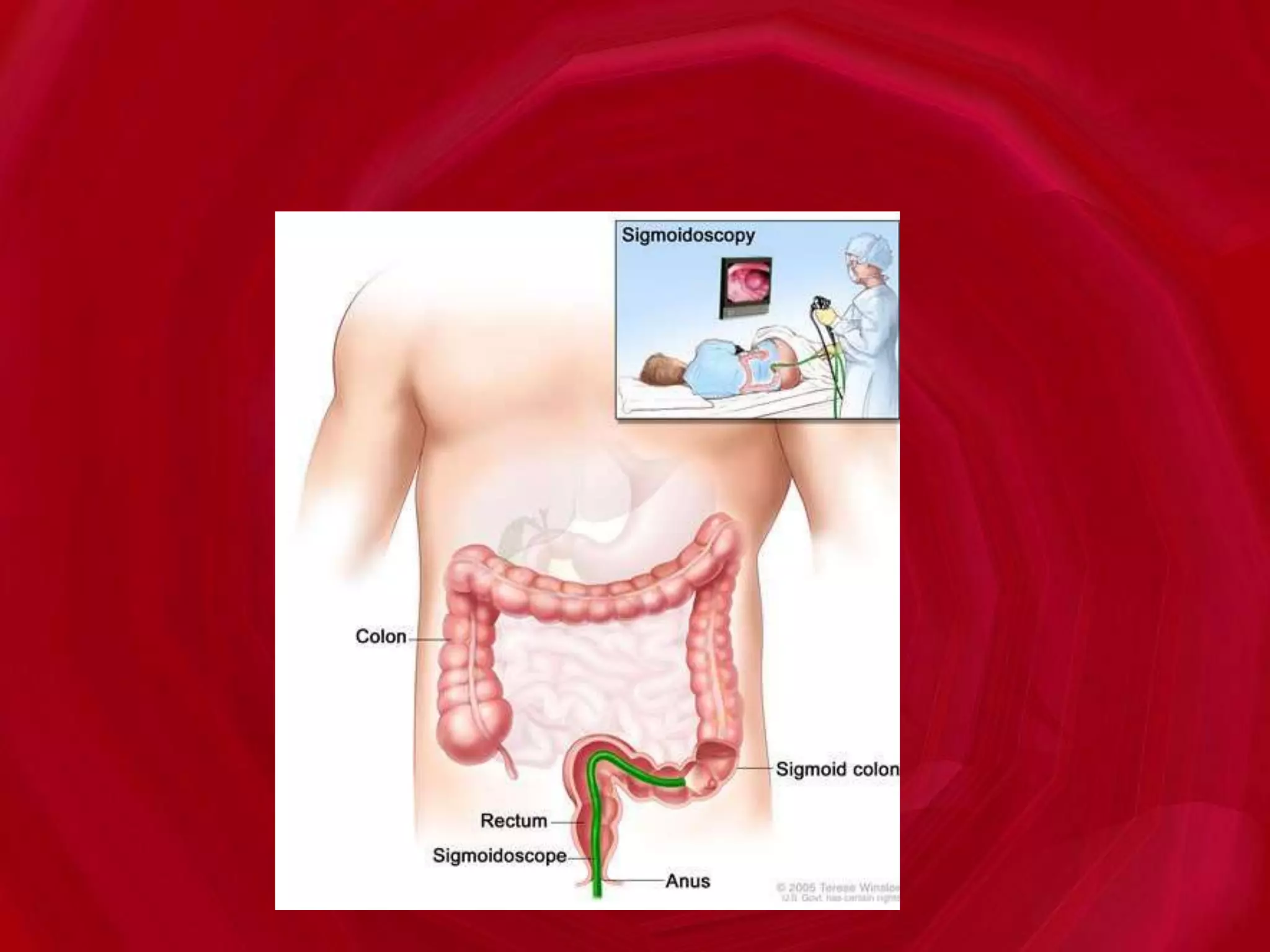
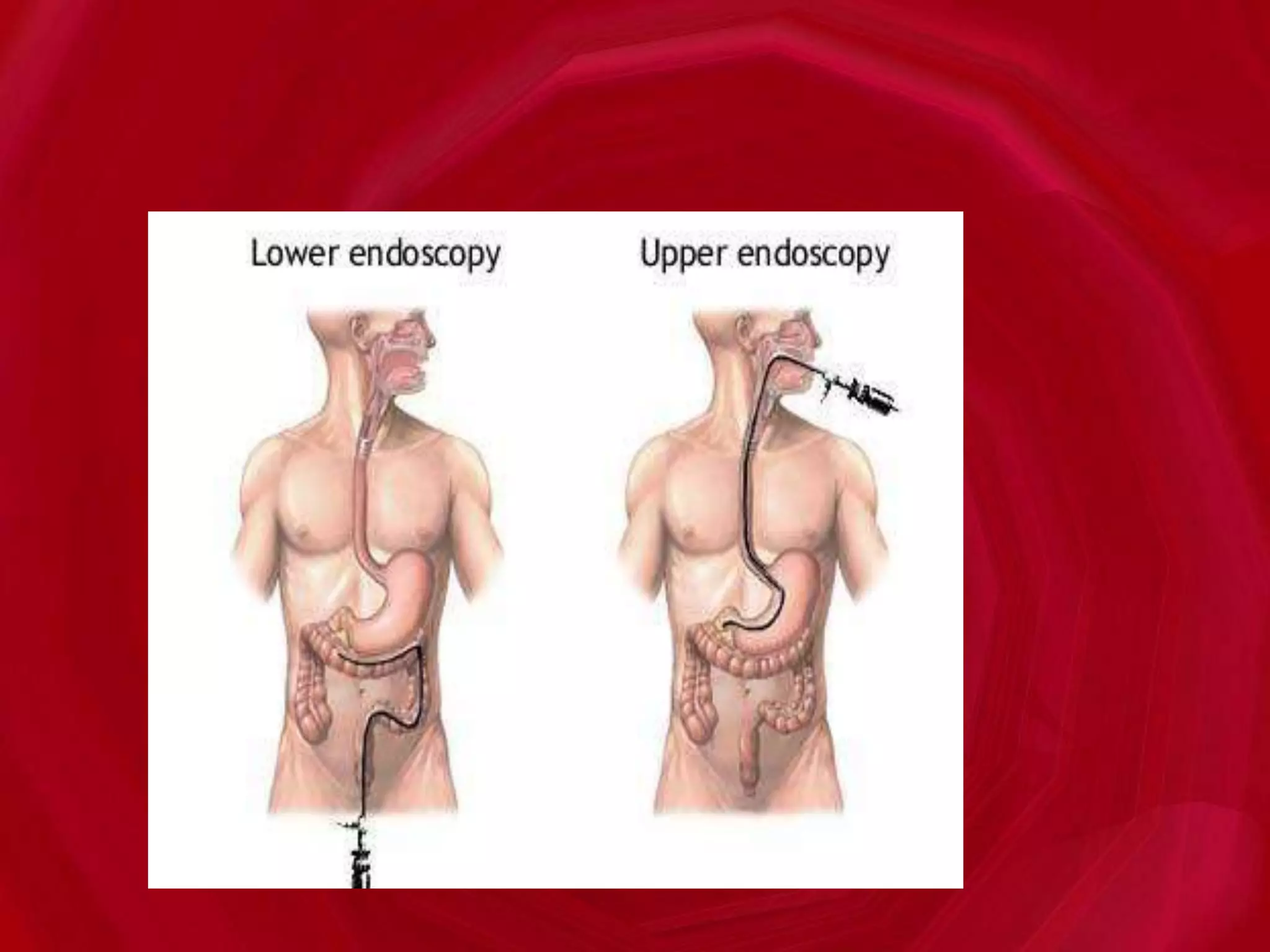
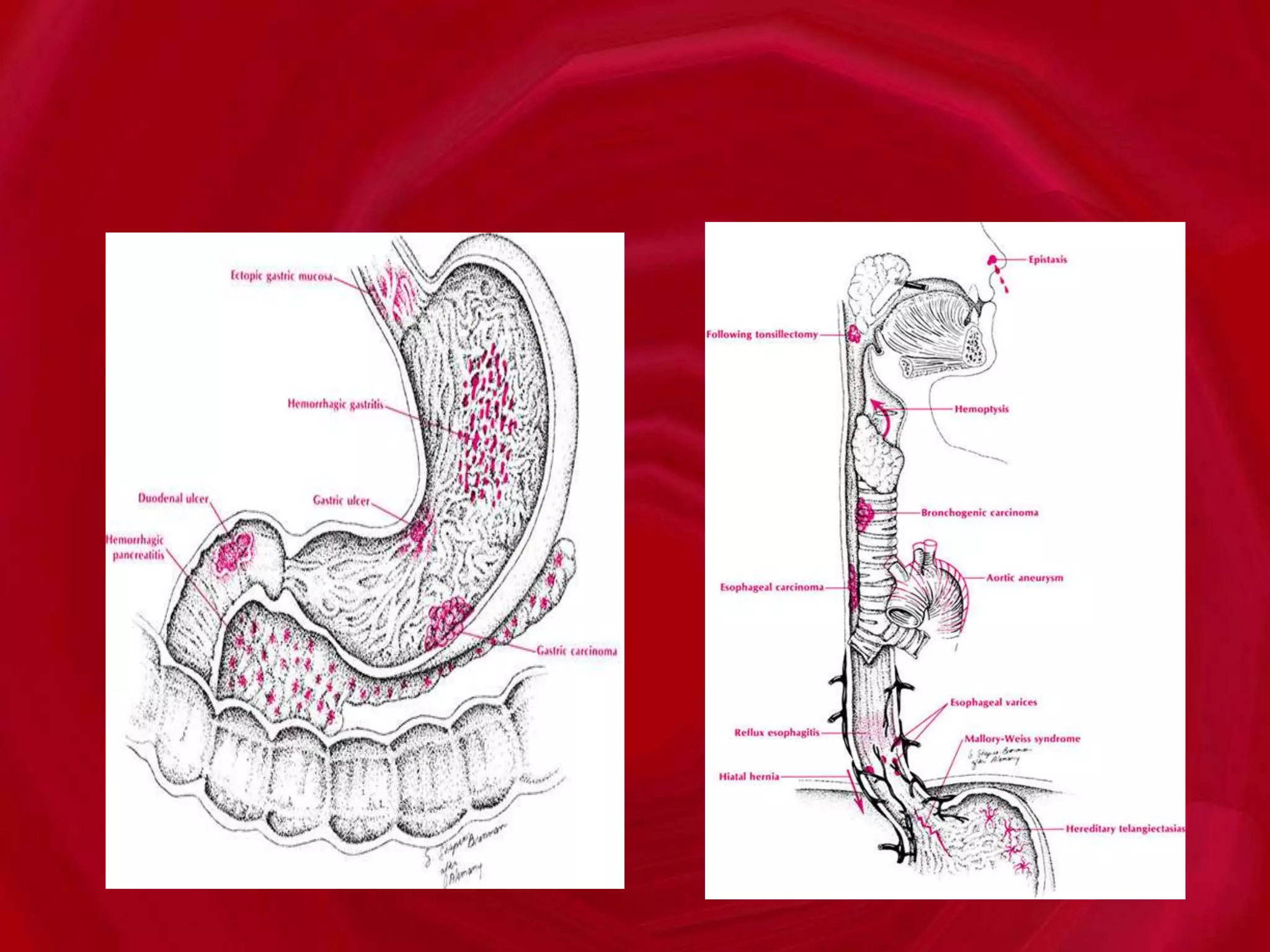
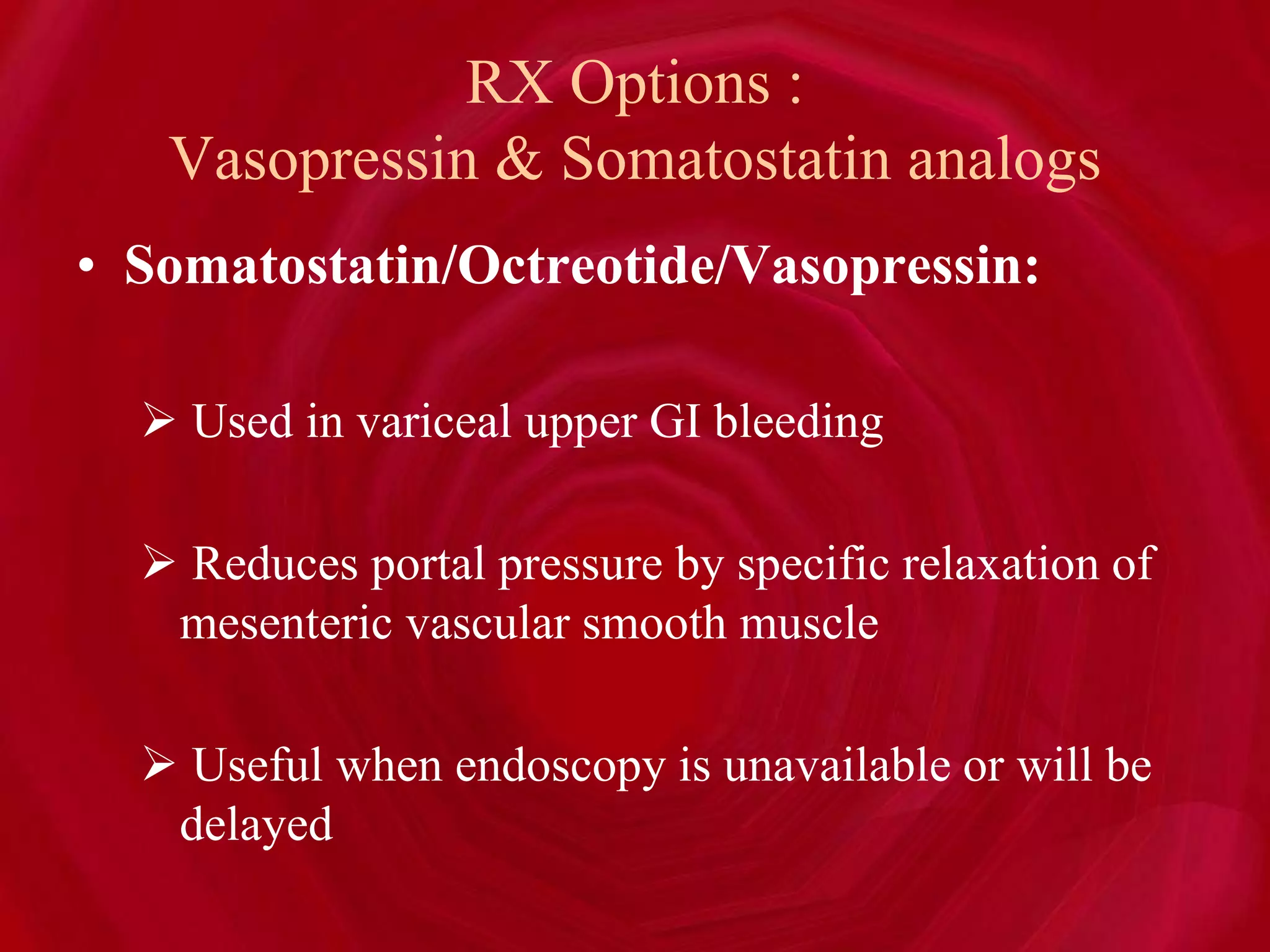
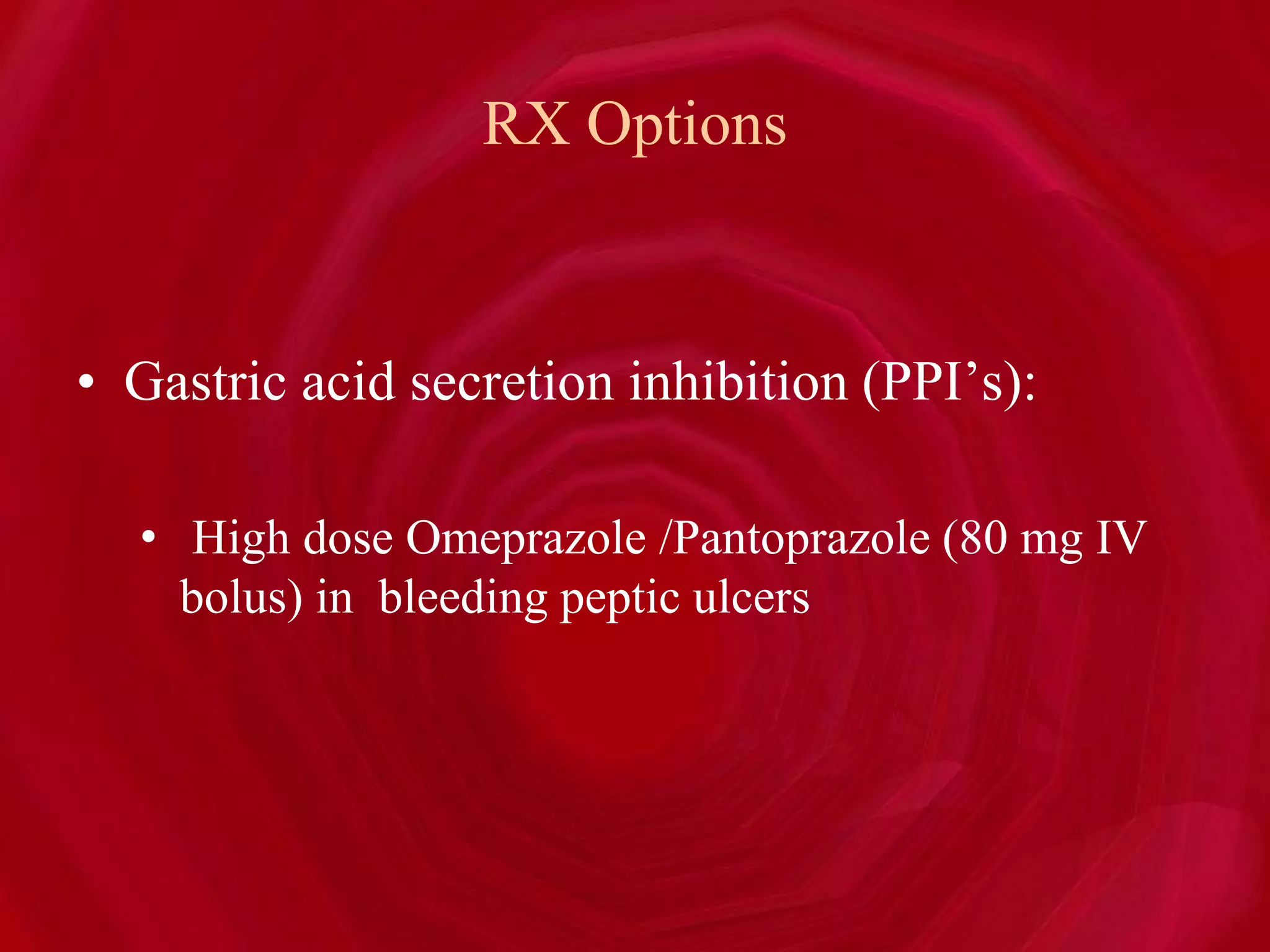
- Common causes of upper GI bleeding are peptic ulcers and esophageal varices, while diverticulosis and colon polyps are common causes of lower GI bleeding.
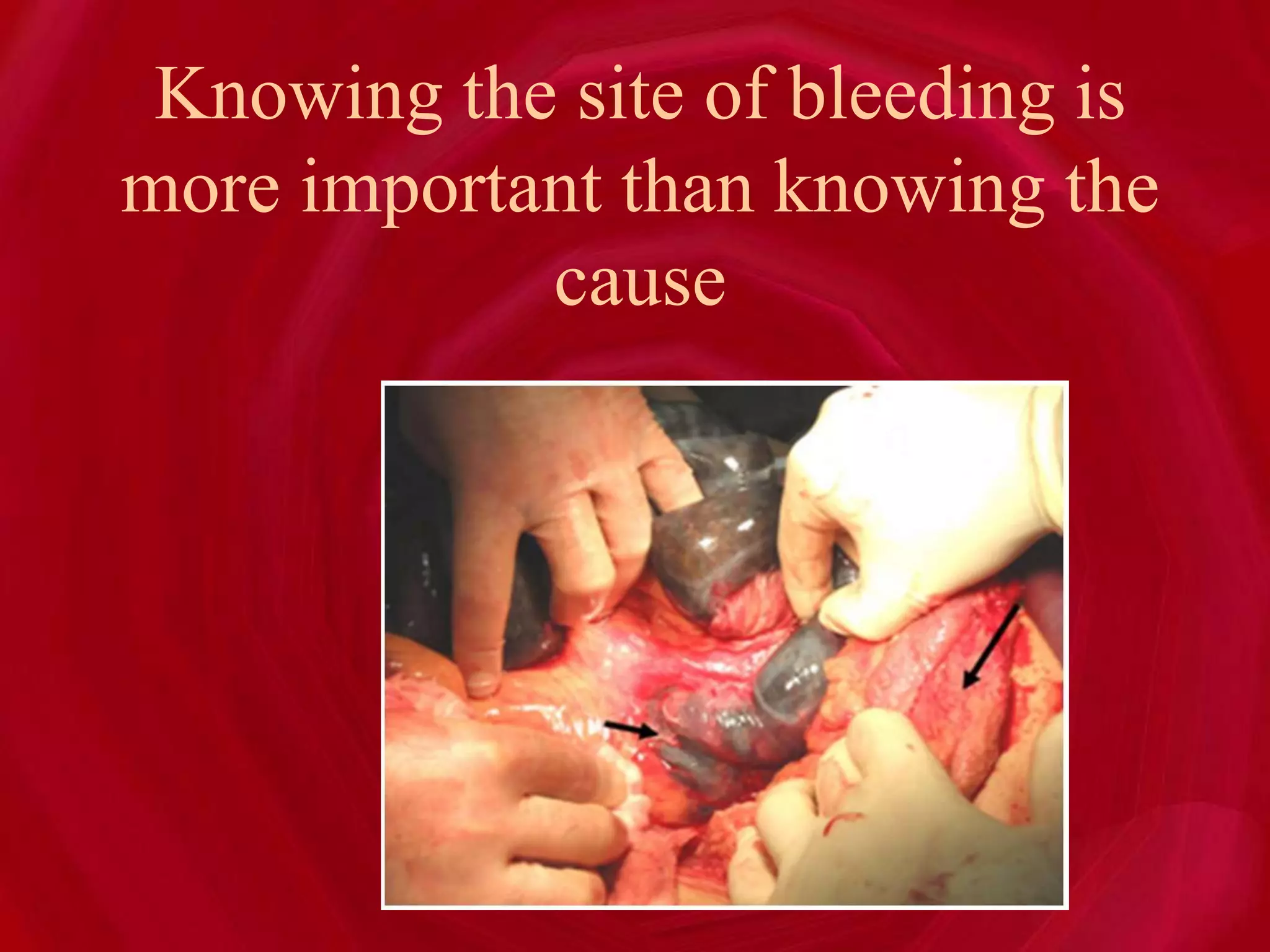
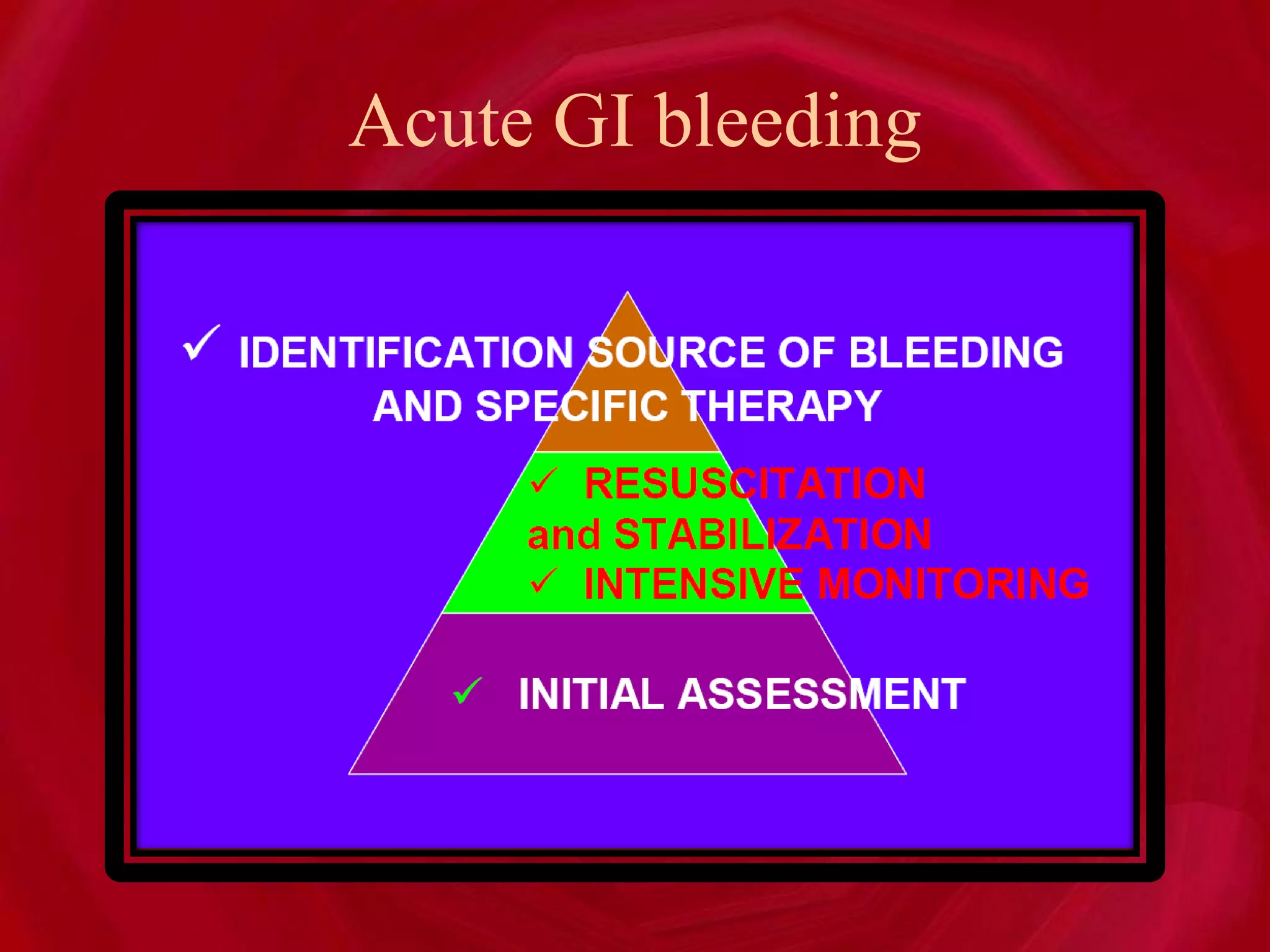
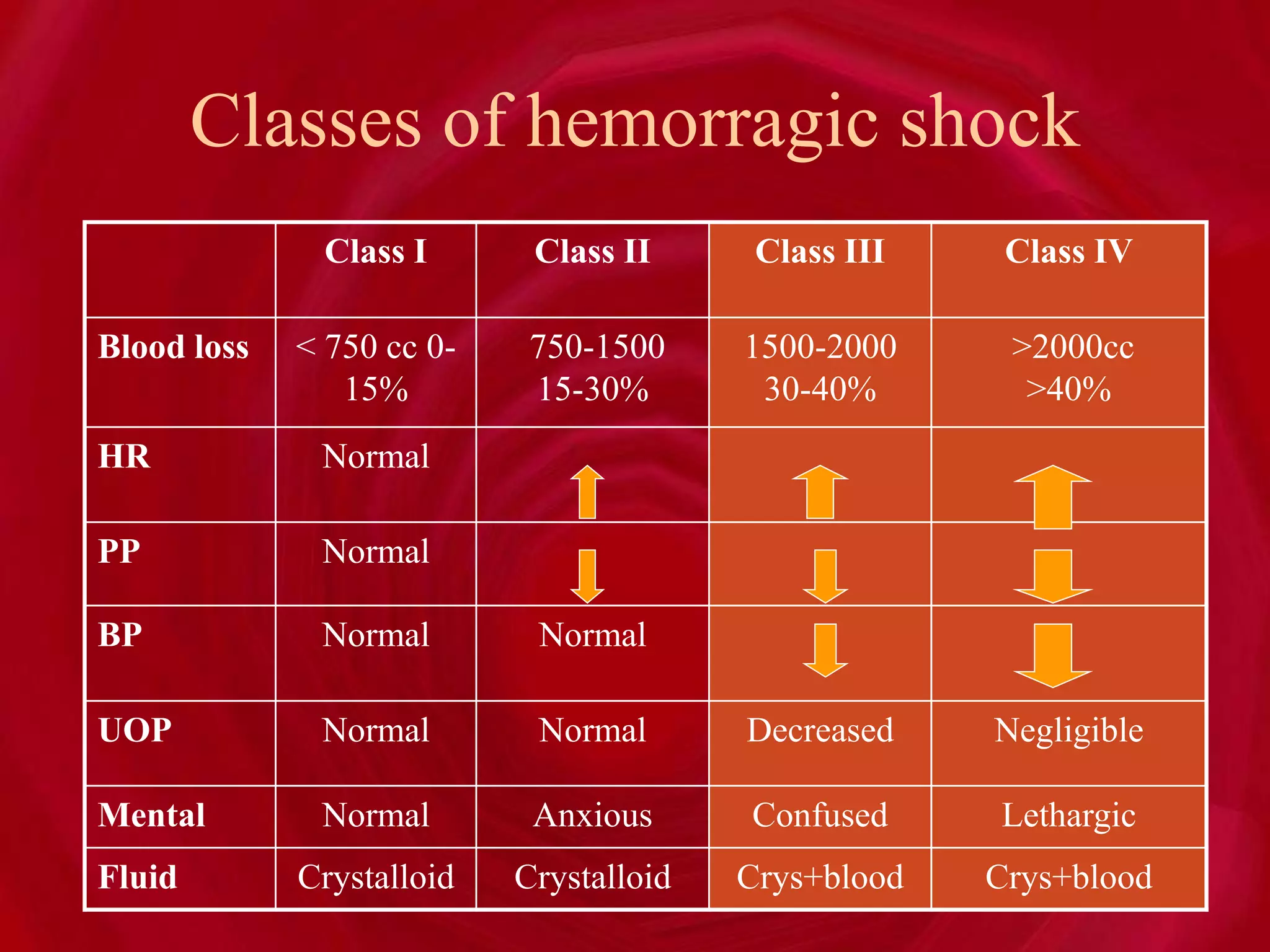
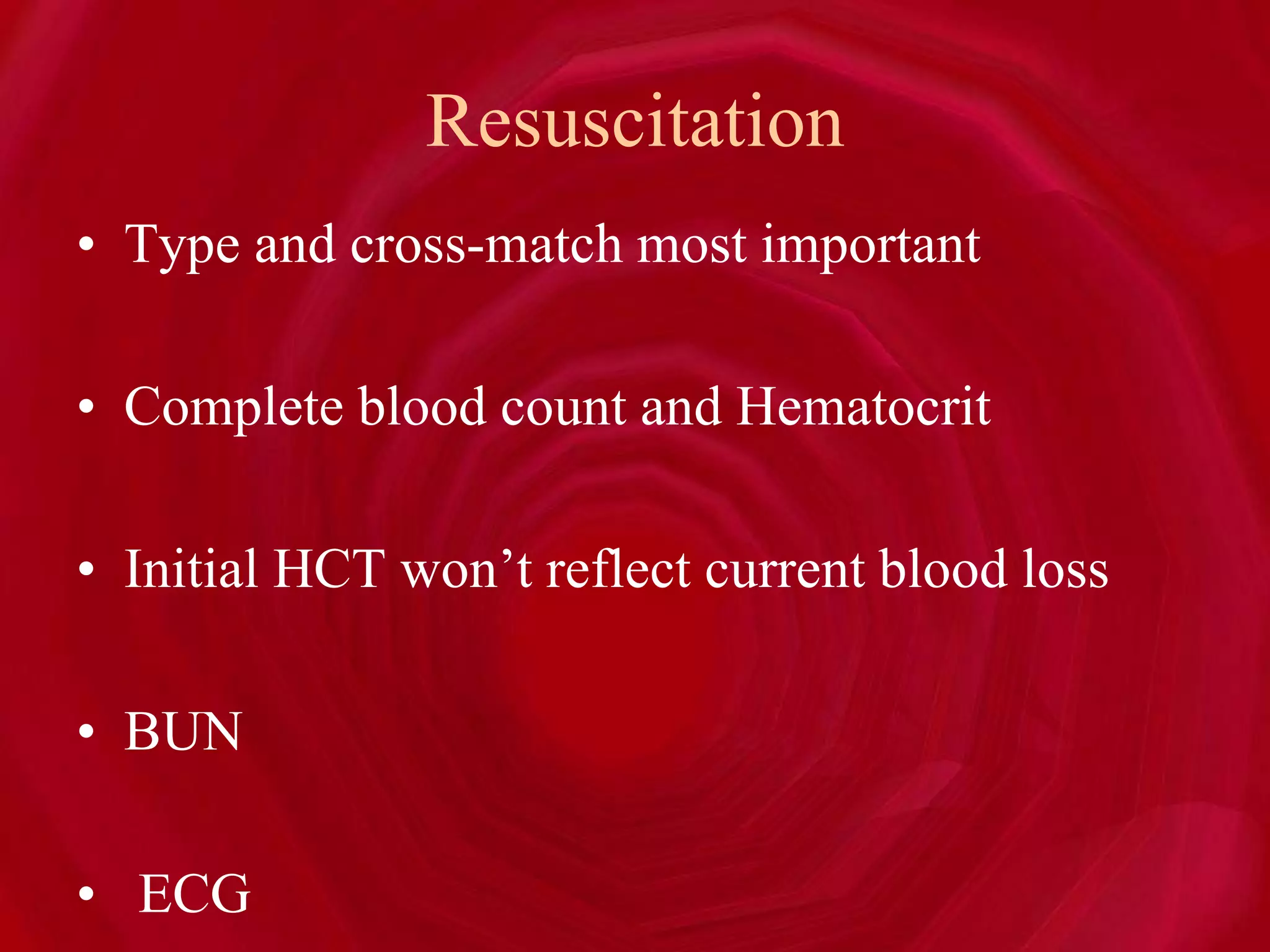
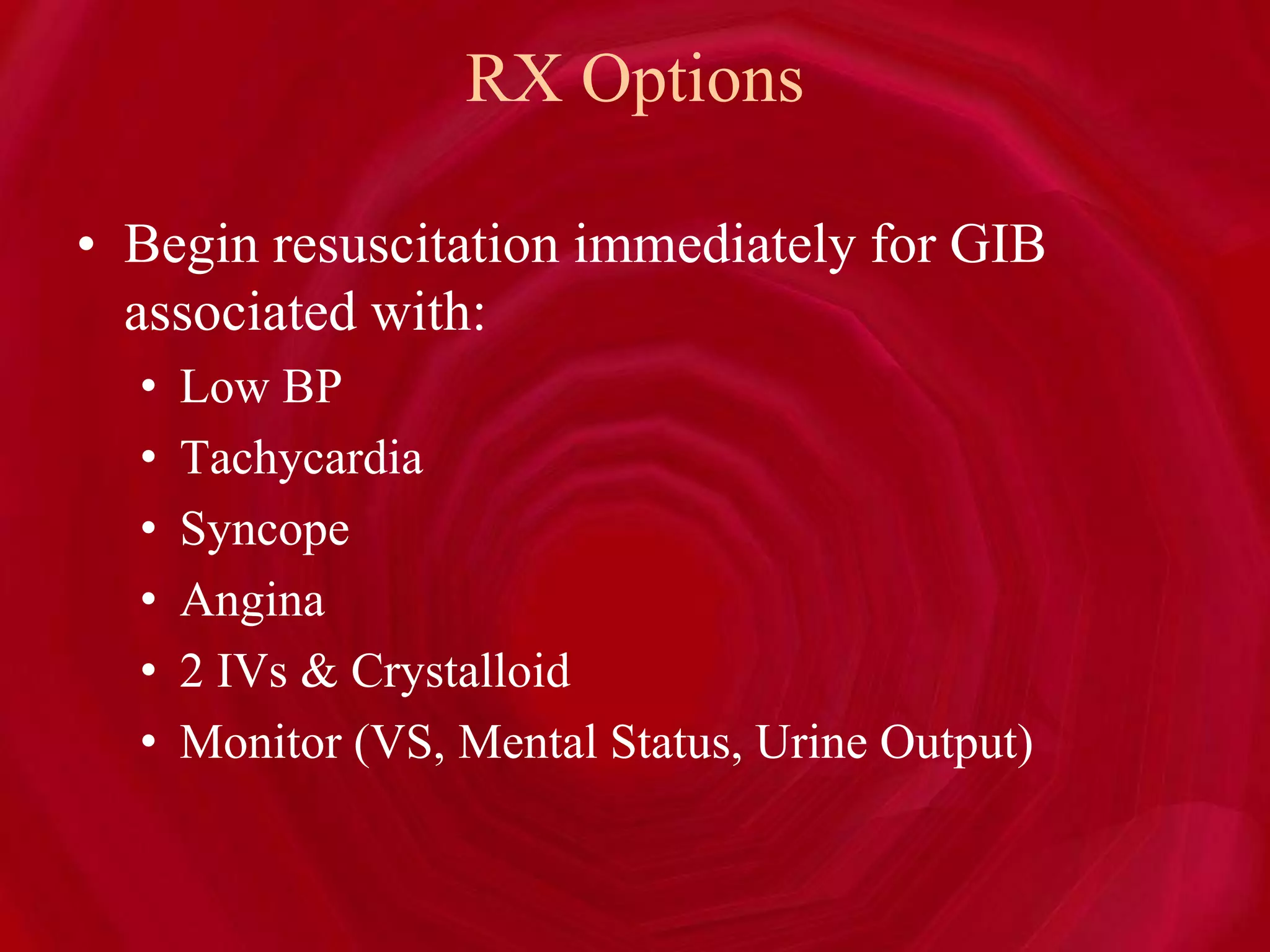
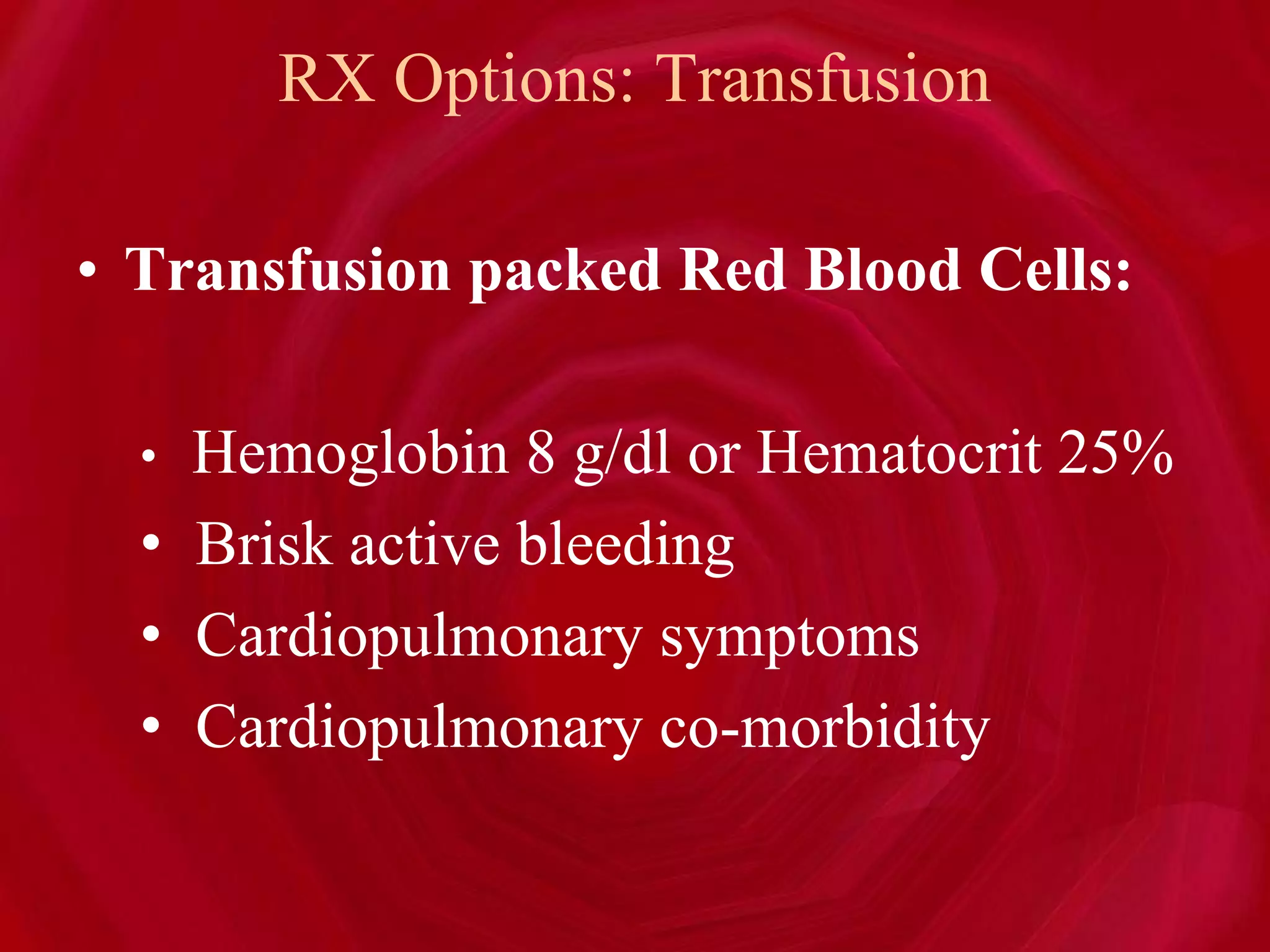
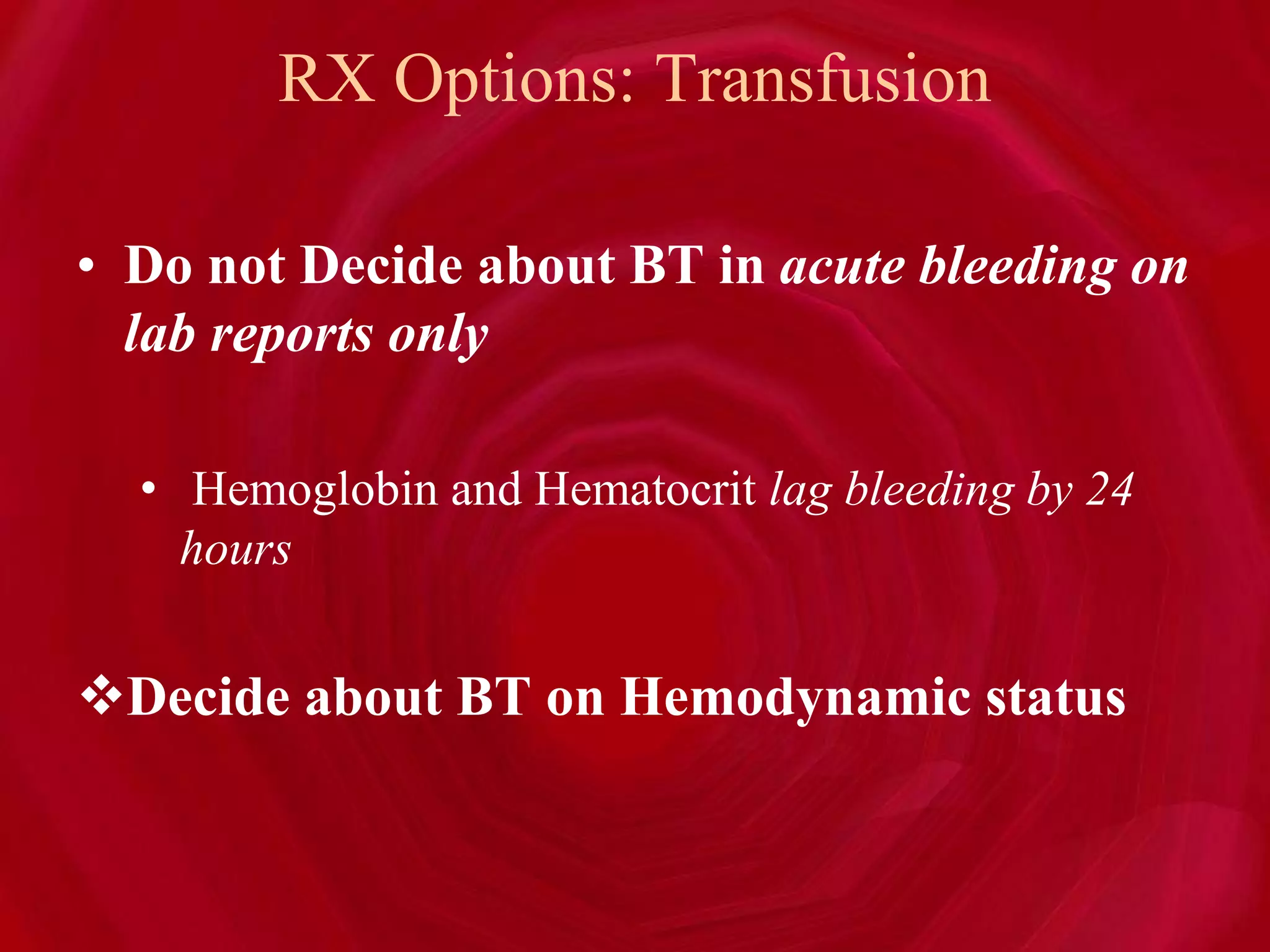
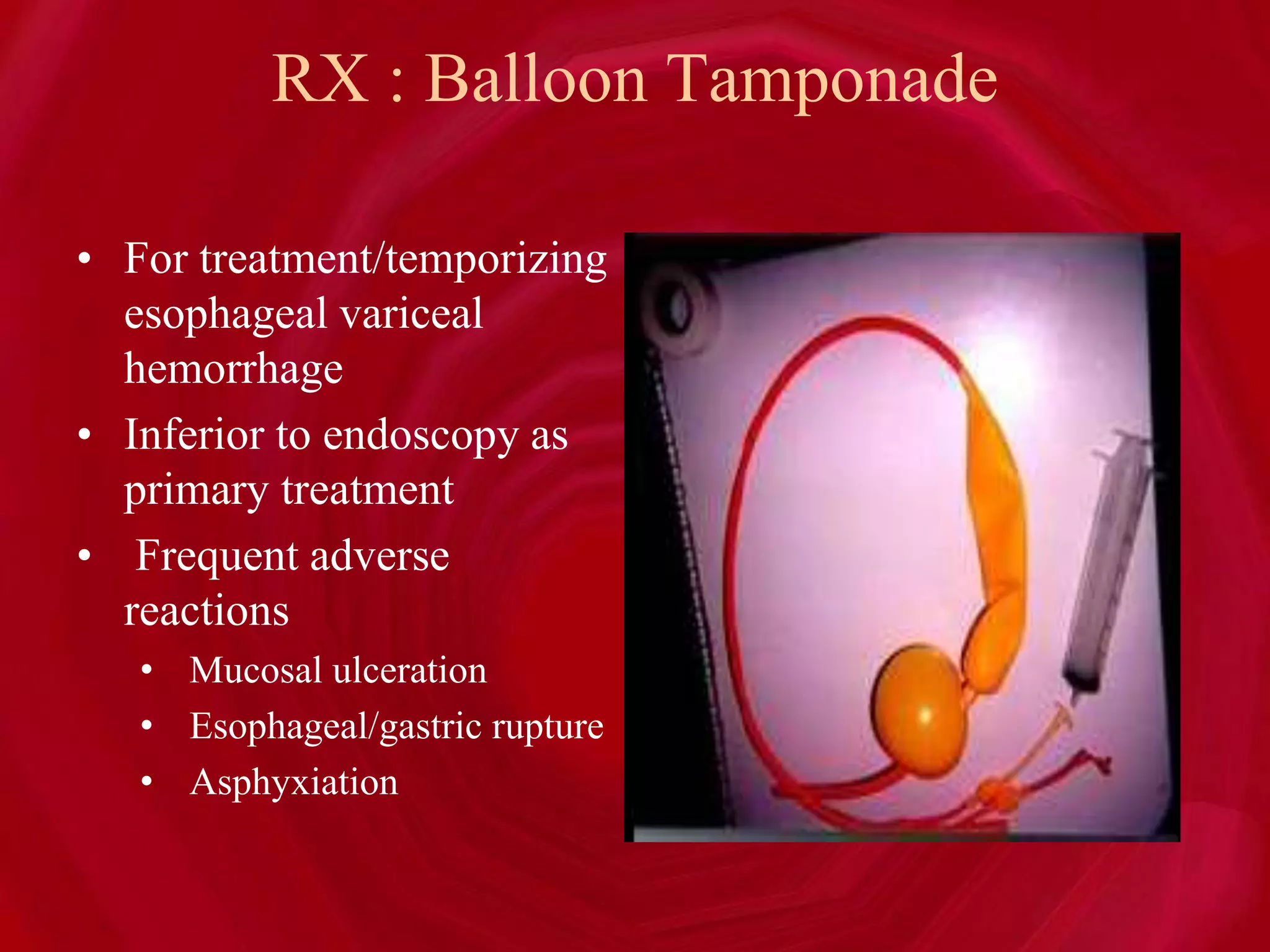
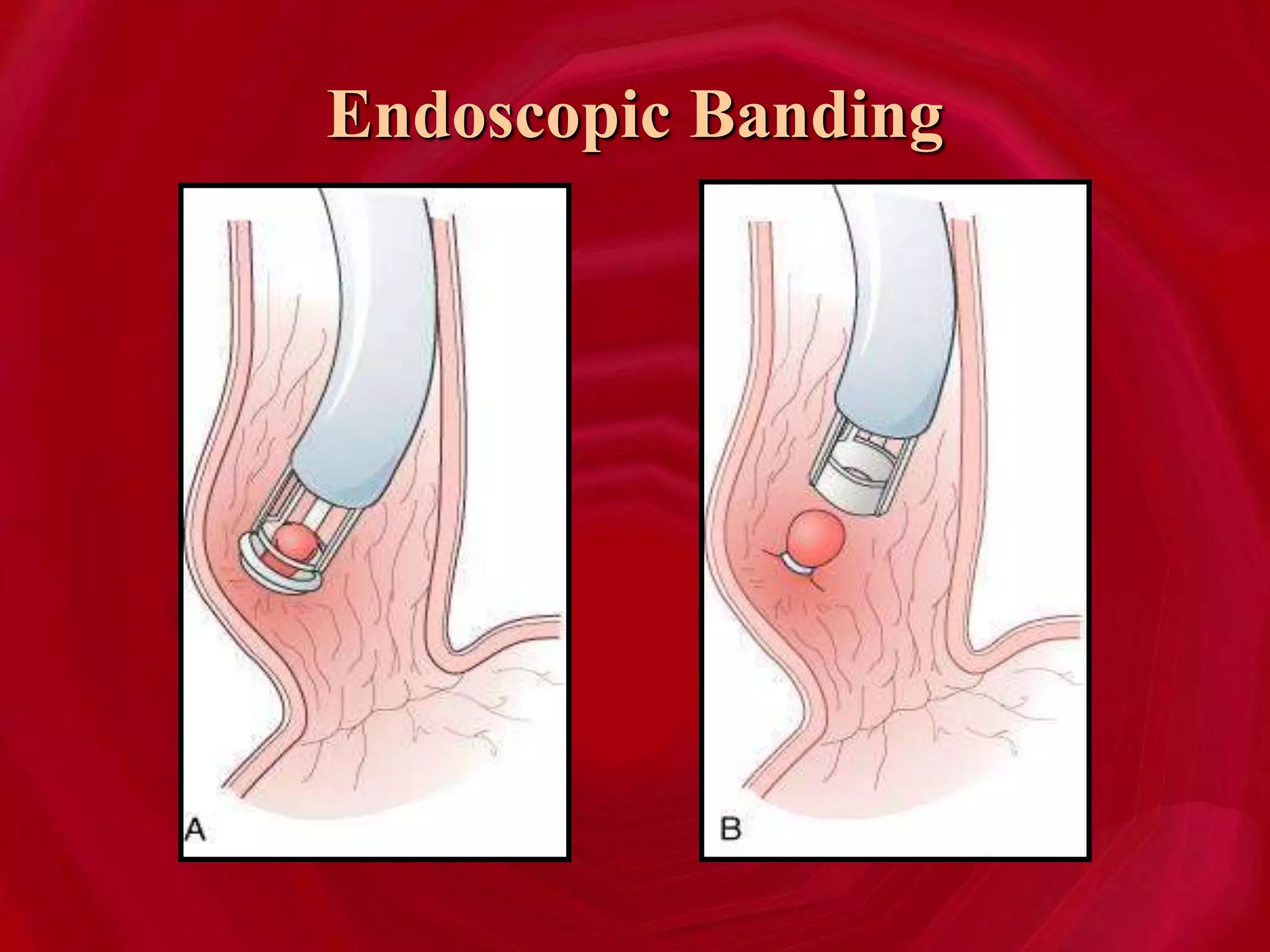
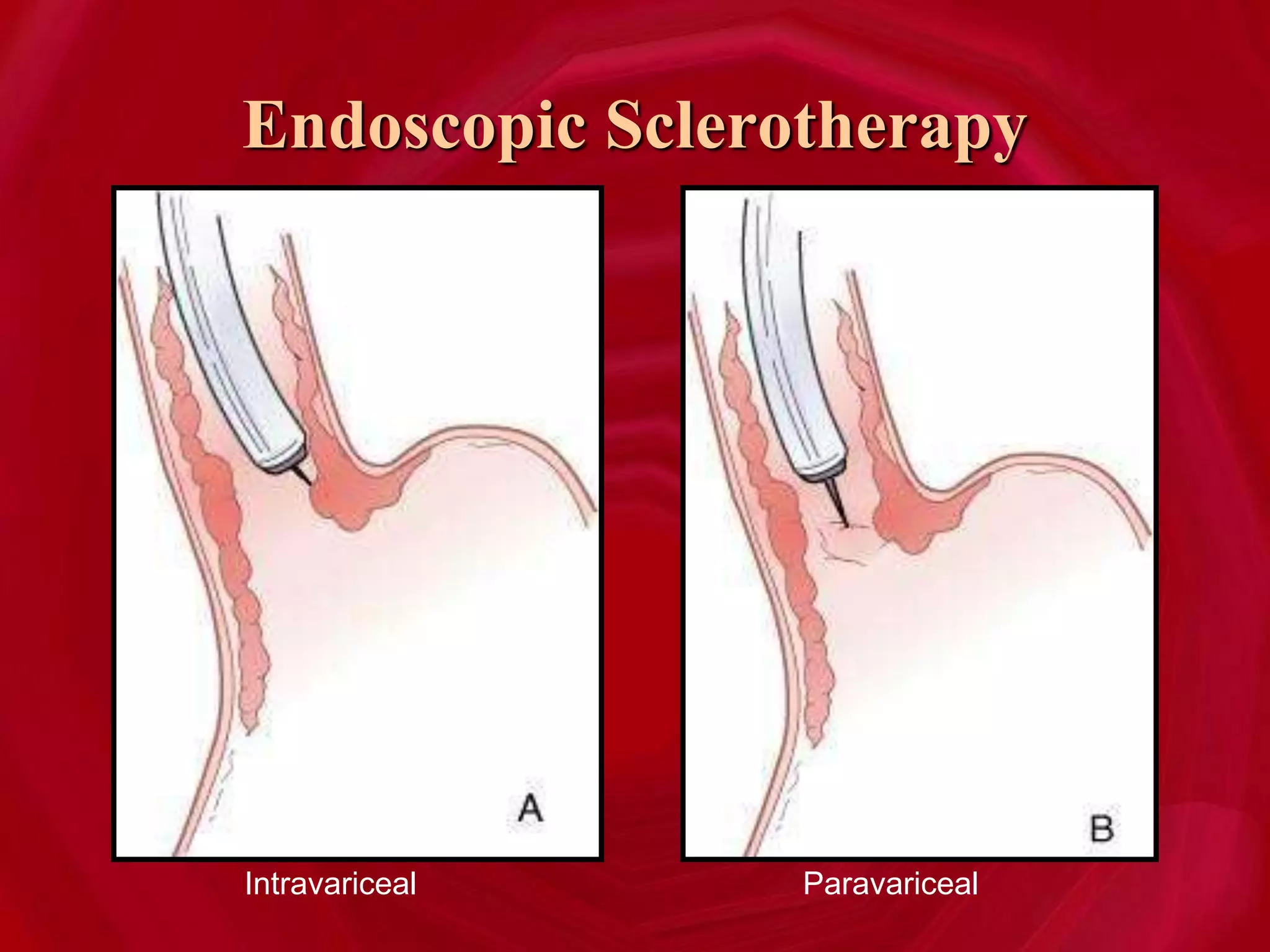
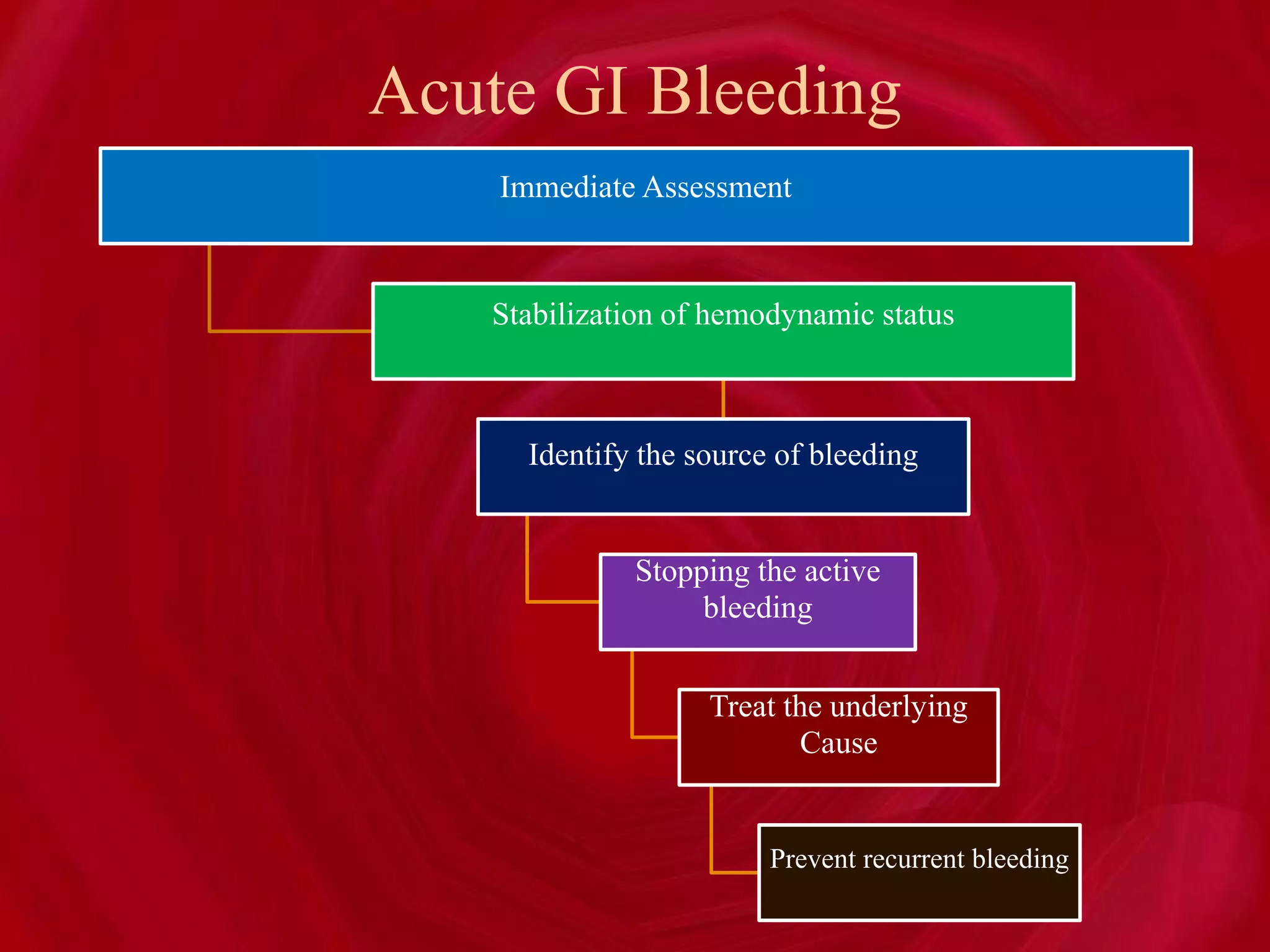
- The approach to a patient with GI bleeding involves stabilizing their hemodynamic status, identifying the source of bleeding, stopping active bleeding, treating the underlying cause, and preventing recurrent